Abstract
Introduction
Obesity is an independent risk factor for postoperative atrial fibrillation (POAF) after coronary artery bypass grafting (CABG) surgery. POAF in patients with severe obesity (body mass index [BMI] ≥ 35 kg/m2) is less studied. Whether waist circumference (WC) improves prediction of POAF independently of BMI among patients with severe obesity remains unknown.
Aim
To evaluate the risk of POAF, the role of WC in predicting POAF and postoperative complications after CABG surgery in severe obesity.
Methods
Our cohort included 7995 patients undergoing CABG surgery (2006−19). POAF risk was compared across BMI and WC categories. In patients with severe obesity, the association of an increase in WC with POAF risk was assessed.
Results
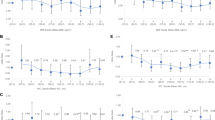
763 (9.5%) patients had a BMI ≥ 35 kg/m2. In this group, BMI was 38.5 ± 3.6 kg/m2 and WC was 123.4 ± 10.8 cm. More patients with severe obesity developed POAF compared to patients with a normal BMI (37 vs. 29%, aRR: 1.52[95%CI 1.36−1.72], p < 0.01). Within each BMI category, the risk of POAF was higher per increasing tertile of WC (p < 0.05). Among patients with a BMI ≥ 35 kg/m2, every 10 cm increment in WC was associated with an increased risk of POAF (aRR: 1.16[95%CI 1.08-1.24], p < 0.01). POAF in patients with severe obesity was associated with increased hospital length of stay.
Conclusions
Severe obesity increases the risk of POAF after CABG surgery. In this subgroup, elevated WC may provide additional prognostic value independently of BMI. Since POAF is associated with adverse long-term outcomes, abdominal obesity by measurement of WC should be assessed and targeted even in patient with severe obesity.

Central Illustration Increasing waist circumference associated with increased atrial fibrillation risk post coronary artery bypass grafting. Bar graph of the unadjusted absolute risk and 95% confidence interval of postoperative atrial fibrillation for each tertile of waist circumference per body mass index category. Comparison of postoperative atrial fibrillation risk with chi-square test showing an increasing risk of postoperative atrial fibrillation related to increasing waist circumference within each body mass index category. Abbreviations: BMI, body mass index; POAF, postoperative atrial fibrillation; WC, waist circumference.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51:793–801. https://doi.org/10.1016/j.jacc.2007.10.043.
Greenberg JW, Lancaster TS, Schuessler RB, Melby SJ. Postoperative atrial fibrillation following cardiac surgery: a persistent complication. Eur J Cardiothorac Surg. 2017;52:665–72. https://doi.org/10.1093/ejcts/ezx039.
Hernandez AV, Kaw R, Pasupuleti V, Bina P, Ioannidis JP, Bueno H, et al. Association between obesity and postoperative atrial fibrillation in patients undergoing cardiac operations: a systematic review and meta-analysis. Ann Thorac Surg. 2013;96:1104–16. https://doi.org/10.1016/j.athoracsur.2013.04.029.
Phan K, Khuong JN, Xu J, Kanagaratnam A, Yan TD. Obesity and postoperative atrial fibrillation in patients undergoing cardiac surgery: systematic review and meta-analysis. Int J Cardiol. 2016;217:49–57. https://doi.org/10.1016/j.ijcard.2016.05.002.
Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291:1720–9. https://doi.org/10.1001/jama.291.14.1720.
Almassi GH, Schowalter T, Nicolosi AC, Aggarwal A, Moritz TE, Henderson WG, et al. Atrial fibrillation after cardiac surgery: a major morbid event? Ann Surg. 1997;226:501–11. https://doi.org/10.1097/00000658-199710000-00011.
Wong CX, Sullivan T, Sun MT, Mahajan R, Pathak RK, Middeldorp M, et al. Obesity and the risk of incident, post-operative, and post-ablation atrial fibrillation: a meta-analysis of 626,603 individuals in 51 studies. JACC Clin Electrophysiol. 2015;1:139–52. https://doi.org/10.1016/j.jacep.2015.04.004.
Echahidi N, Mohty D, Pibarot P, Després JP, O’Hara G, Champagne J, et al. Obesity and metabolic syndrome are independent risk factors for atrial fibrillation after coronary artery bypass graft surgery. Circulation. 2007;116:I213–9. https://doi.org/10.1161/CIRCULATIONAHA.106.681304.
Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Obesity and risk of new-onset atrial fibrillation after cardiac surgery. Circulation. 2005;112:3247–55. https://doi.org/10.1161/CIRCULATIONAHA.105.553743.
Javed S, Gupta D, Lip GYH. Obesity and atrial fibrillation: making inroads through fat. Eur Heart J Cardiovasc Pharmacother. 2021;7:59–67. https://doi.org/10.1093/ehjcvp/pvaa013.
Wong CX, Sun MT, Odutayo A, Emdin CA, Mahajan R, Lau DH, et al. Associations of epicardial, abdominal, and overall adiposity with atrial fibrillation. Circ Arrhythm Electrophysiol. 2016;9:e004378. https://doi.org/10.1161/CIRCEP.116.004378.
Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126:1301–13. https://doi.org/10.1161/CIRCULATIONAHA.111.067264.
Piché ME, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity and body fat distribution to cardiovascular disease: an update. Prog Cardiovasc Dis. 2018;61:103–13. https://doi.org/10.1016/j.pcad.2018.06.004.
Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases. Circ Res. 2020;126:1477–1500. https://doi.org/10.1161/CIRCRESAHA.120.316101.
Powell-Wiley TM, Poirier P, Burke LE, Després JP, Gordon-Larsen P, Lavie CJ, et al. Obesity and cardiovascular disease: a scientific statement from the american heart association. Circulation. 2021;143:e984–1010. https://doi.org/10.1161/CIR.0000000000000973.
Nazare JA, Smith J, Borel AL, Aschner P, Barter P, Van Gaal L, et al. Usefulness of measuring both body mass index and waist circumference for the estimation of visceral adiposity and related cardiometabolic risk profile (from the INSPIRE ME IAA study). Am J Cardiol. 2015;115:307–15. https://doi.org/10.1016/j.amjcard.2014.10.039.
Aune D, Sen A, Schlesinger S, Norat T, Janszky I, Romundstad P, et al. Body mass index, abdominal fatness, fat mass and the risk of atrial fibrillation: a systematic review and dose-response meta-analysis of prospective studies. Eur J Epidemiol. 2017;32:181–92. https://doi.org/10.1007/s10654-017-0232-4.
Chassé M, Mathieu P, Voisine P, Després JP, Pibarot P, Baillot R, et al. The underestimated belly factor: waist circumference is linked to significant morbidity following isolated coronary artery bypass grafting. Can J Cardiol. 2016;32:327–35. https://doi.org/10.1016/j.cjca.2015.06.031.
Borel AL, Coumes S, Reche F, Ruckly S, Pépin JL, Tamisier R, et al. Waist, neck circumferences, waist-to-hip ratio: Which is the best cardiometabolic risk marker in women with severe obesity? The SOON cohort. PLoS ONE. 2018;13:e0206617. https://doi.org/10.1371/journal.pone.0206617.
Lemieux I, Drapeau V, Richard D, Bergeron J, Marceau P, Biron S, et al. Waist girth does not predict metabolic complications in severely obese men. Diabetes Care. 2006;29:1417–9. https://doi.org/10.2337/dc06-0441.
Drapeau V, Lemieux I, Richard D, Bergeron J, Tremblay A, Biron S, et al. Waist circumference is useless to assess the prevalence of metabolic abnormalities in severely obese women. Obes Surg. 2007;17:905–9. https://doi.org/10.1007/s11695-007-9168-1.
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight 403 and Obesity in Adults-The Evidence Report. National Institutes of Health. Obes Res 6 51S-209S, 1998.
Lohman T, Roche A, Martorell R Chapter 4: circumferences. Roche and Martorell, editors. In: Anthropometric Standardization Reference Manual. Champaign, Illinois: Human Kinetics Books; 1988:39–80.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol In Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97. https://doi.org/10.1001/jama.285.19.2486.
Andrade JG, Aguilar M, Atzema C, Bell A, Cairns JA, Cheung CC, et al. The 2020 Canadian Cardiovascular Society/Canadian Heart Rhythm Society Comprehensive Guidelines for the Management of Atrial Fibrillation. Can J Cardiol. 2020;36:1847–948. https://doi.org/10.1016/j.cjca.2020.09.001.
Sousa-Uva M, Head SJ, Milojevic M, Collet JP, Landoni G, Castella M, et al. 2017 EACTS Guidelines on perioperative medication in adult cardiac surgery. Eur J Cardiothorac Surg. 2018;53:5–33. https://doi.org/10.1093/ejcts/ezx314.
Takagi H, Umemoto T. ALICE (All-Literature Investigation of Cardiovascular Evidence) Group. Overweight, but not obesity, paradox on mortality following coronary artery bypass grafting. J Cardiol. 2016;68:215–21. https://doi.org/10.1016/j.jjcc.2015.09.015.
Jin R, Grunkemeier GL, Furnary AP, Handy JR Jr. Is obesity a risk factor for mortality in coronary artery bypass surgery? Circulation. 2005;111:3359–65. https://doi.org/10.1161/CIRCULATIONAHA.104.489880.
Girerd N, Pibarot P, Fournier D, Daleau P, Voisine P, O’Hara G, et al. Middle-aged men with increased waist circumference and elevated C-reactive protein level are at higher risk for postoperative atrial fibrillation following coronary artery bypass grafting surgery. Eur Heart J. 2009;30:1270–8. https://doi.org/10.1093/eurheartj/ehp091.
Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: pathophysiology and management. J Am Coll Cardiol. 2018;71:69–84. https://doi.org/10.1016/j.jacc.2017.11.011.
Pouliot MC, Després JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, et al. Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol. 1994;73:460–8. https://doi.org/10.1016/0002-9149(94)90676-9.
Abed HS, Samuel CS, Lau DH, Kelly DJ, Royce SG, Alasady M, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm. 2013;10:90–100. https://doi.org/10.1016/j.hrthm.2012.08.043.
Goette A, Kalman JM, Aguinaga L, Akar J, Cabrera JA, Chen SA, et al. EHRA/HRS/APHRS/SOLAECE expert consensus on atrial cardiomyopathies: definition, characterization, and clinical implication. Europace. 2016;18:1455–90. https://doi.org/10.1093/europace/euw161.
Mahajan R, Nelson A, Pathak RK, Middeldorp ME, Wong CX, Twomey DJ. et al.Electroanatomical remodeling of the Atria in obesity impact of adjacent epicardial fat.JACC Clin Electrophysiol.2018;4:1529–40. https://doi.org/10.1016/j.jacep.2018.08.014.
Wong CX, Ganesan AN, Selvanayagam JB. Epicardial fat and atrial fibrillation: current evidence, potential mechanisms, clinical implications, and future directions. Eur Heart J. 2017;38:1294–302. https://doi.org/10.1093/eurheartj/ehw045.
Dobrev D, Aguilar M, Heijman J, Guichard JB, Nattel S. Postoperative atrial fibrillation: mechanisms, manifestations and management. Nat Rev Cardiol. 2019;16:417–36. https://doi.org/10.1038/s41569-019-0166-5.
Andrade J, Khairy P, Dobrev D, Nattel S. The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res. 2014;114:1453–68. https://doi.org/10.1161/CIRCRESAHA.114.303211.
Vyas V, Lambiase P. Obesity and atrial fibrillation: epidemiology, pathophysiology and novel therapeutic opportunities. Arrhythm Electrophysiol Rev. 2019;8:28–36. https://doi.org/10.15420/aer.2018.76.2.
Akintoye E, Sellke F, Marchioli R, Tavazzi L, Mozaffarian D. Factors associated with postoperative atrial fibrillation and other adverse events after cardiac surgery. J Thorac Cardiovasc Surg. 2018;155:242–.e10. https://doi.org/10.1016/j.jtcvs.2017.07.063.
Elahi M, Hadjinikolaou L, Galiñanes M. Incidence and clinical consequences of atrial fibrillation within 1 year of first-time isolated coronary bypass surgery. Circulation. 2003;108:II207–12. https://doi.org/10.1161/01.cir.0000089188.45285.fd.
Mathew JP, Parks R, Savino JS, Friedman AS, Koch C, Mangano DT, et al. Atrial fibrillation following coronary artery bypass graft surgery: predictors, outcomes, and resource utilization. MultiCenter Study of Perioperative Ischemia Research Group. JAMA. 1996;276:300–6.
Attaran S, Shaw M, Bond L, Pullan MD, Fabri BM. Atrial fibrillation postcardiac surgery: a common but a morbid complication. Interact Cardiovasc Thorac Surg. 2011;12:772–7. https://doi.org/10.1510/icvts.2010.243782.
Bessissow A, Khan J, Devereaux PJ, Alvarez-Garcia J, Alonso-Coello P. Postoperative atrial fibrillation in non-cardiac and cardiac surgery: an overview. J Thromb Haemost. 2015;13:S304–12. https://doi.org/10.1111/jth.12974.
Wigfield CH, Lindsey JD, Muñoz A, Chopra PS, Edwards NM, Love RB. Is extreme obesity a risk factor for cardiac surgery? An analysis of patients with a BMI > or = 40. Eur J Cardiothorac Surg. 2006;4:434–40. https://doi.org/10.1016/j.ejcts.2006.01.016.
Thorén E, Wernroth ML, Christersson C, Grinnemo KH, Jidéus L, Ståhle E. Compared with matched controls, patients with postoperative atrial fibrillation (POAF) have increased long-term AF after CABG, and POAF is further associated with increased ischemic stroke, heart failure and mortality even after adjustment for AF. Clin Res Cardiol. 2020;109:1232–42. https://doi.org/10.1007/s00392-020-01614-z.
Acknowledgements
The authors thank Ms. Stéphanie Dionne for her contribution to the registry.
Funding
AP is supported by doctoral/fellowship scholarships from the Canadian Institutes for Health Research (Canada), Fonds de recherche du Québec – Santé (Québec, Canada), Association des cardiologues du Québec (Québec, Canada), Laval University Dean’s Scholarship (Québec, Québec, Canada) and Réseau de recherche en cardiométabolique, diabète et obésité (Québec, Canada). SO is supported by doctoral research scholarships from the Canadian Institutes for Health Research (Canada), Fonds de recherche du Québec – Santé (Québec, Canada). MEP is recipient of a Junior 1 clinician-researcher scholar from the Fonds de Recherche du Québec-Santé (FRQS) (Québec, Canada).
Author information
Authors and Affiliations
Contributions
JR and MEP conceived of the presented idea. SO performed the analysis. JR drafted the manuscript. AP designed the figures and the central illustration. JR, AP and SO contributed to the interpretation of the results. MEP was in charge of overall direction and planning. MEP and PP guided the orientation of the manuscript. AP, SO, MEP and PP provided comments on the drafted manuscript. PV and JPD provided critical feedback and discussed the results and analysis. All authors contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in accordance with the ethical standards set forth by the Declaration of Helsinki and approved approved by the ethics committee of the IUCPQ-ULaval Research Center (reference number 2024-4062). The need for patient consent was waived due to the retrospective nature of the analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Roberge, J., Paquin, A., Poirier, P. et al. Postoperative atrial fibrillation following cardiac surgery in severe obesity: the added value of waist circumference. Int J Obes 49, 827–834 (2025). https://doi.org/10.1038/s41366-024-01707-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-024-01707-z
This article is cited by
-
Waist circumference as a measure of obesity associated with postoperative atrial fibrillation?
International Journal of Obesity (2025)