Abstract
Background
Maternal exposure to polycyclic aromatic hydrocarbons (PAHs), ubiquitous constituents of air pollution, has been associated with adverse birth outcomes. Yet it remains unclear whether and how socioeconomic status (SES) affects gestational PAH exposure.
Objective
To examine whether there are socioeconomic disparities in PAHs exposure among pregnant women from Rochester, NY, and if so, to what extent disproportionate proximity to air pollution sources, measured by residential distance to transportation-related sources, contributed to the exposure disparity.
Methods
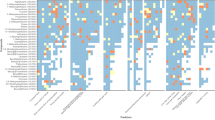
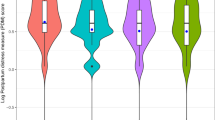
We measured 1-hydroxypyrene concentrations in 726 urine samples collected from 305 pregnant women up to three samples throughout pregnancy. Residential distances to transportation-related sources were calculated based on participants’ home addresses. We used linear mixed-effects models with random intercepts of participants to examine associations between 1-hydroxypyrene, SES indicators, and distance to transportation-related sources. We used structural equation modelling to assess to what extent distance to transportation-related sources contributes to the socioeconomic disparity in 1-hydroxypyrene concentrations.
Results
Reduced household income and maternal education level were both significant SES predictors of 1-hydroxypyrene concentrations, after the adjustment for other maternal demographic characteristics. Each interquartile range (IQR) increases in residential proximity to the airport (from 14.3 to 6.0 km), the railroad yard (from 22.3 to 6.0 km), and annual average daily traffic within 300 m (from 3796 to 99,933 vehicles/year) were associated with 15.0% (95%CI: 7.0–22.2%), 15.4% (95%CI: 6.5–23.5%), and 13.6% (95%CI: 4.7–23.3%) increases in 1-hydroxypyrene concentrations, respectively. Proximity to these sources jointly explained 10% (95%CI: 1.6–18.4%) of the 1-hydroxypyrene concentration change associated with decreases in SES as a latent variable defined by both household income and education level.
Impact statement
Our findings suggest that efforts to address disproportionate residential proximity to transportation-related sources may reduce the socioeconomic disparity in PAH exposure.

This is a preview of subscription content, access via your institution
Access options




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the author for external validation.
References
Perera FP, Rauh V, Tsai WY, Kinney P, Camann D, Barr D, et al. Effects of transplacental exposure to environmental pollutants on birth outcomes in a multiethnic population. Environ Health Perspect. 2003;111:201–5.
Wilhelm M, Ghosh JK, Su J, Cockburn M, Jerrett M, Ritz B. Traffic-related air toxics and preterm birth: a population-based case-control study in Los Angeles county. Calif Environ Heal. 2011;10:89.
Ferguson KK, McElrath T, Pace GG, Weller D, Zeng L, Pennathur S, et al. Urinary polycyclic aromatic hydrocarbon metabolite associations with biomarkers of inflammation, angiogenesis, and oxidative stress in pregnant women. Environ Sci Technol. 2017;acs.est.7b01252.
Cathey AL, Watkins DJ, Rosario ZY, Vélez Vega CM, Loch-Caruso R, Alshawabkeh AN, et al. Polycyclic aromatic hydrocarbon exposure results in altered CRH, reproductive, and thyroid hormone concentrations during human pregnancy. Sci Total Environ. 2020;749:141581.
Choi H, Rauh V, Garfinkel R, Tu Y, Perera FP. Prenatal exposure to airborne polycyclic aromatic hydrocarbons and risk of intrauterine growth restriction. Environ Health Perspect. 2008;116:658–65.
Bongaerts E, Nawrot TS, Van Pee T, Ameloot M, Bové H. Translocation of (ultra)fine particles and nanoparticles across the placenta; a systematic review on the evidence of in vitro, ex vivo, and in vivo studies. Part Fibre Toxicol. 2020;17:56.
Bové H, Bongaerts E, Slenders E, Bijnens EM, Saenen ND, Gyselaers W, et al. Ambient black carbon particles reach the fetal side of human placenta. Nat Commun. 2019;10:3866.
Yuan Y, Jin L, Wang L, Li Z, Zhang L, Zhu H, et al. Levels of PAH-DNA adducts in placental tissue and the risk of fetal neural tube defects in a Chinese population. Reprod Toxicol. 2013;37:70–5.
Ren A, Qiu X, Jin L, Ma J, Li Z, Zhang L, et al. Association of selected persistent organic pollutants in the placenta with the risk of neural tube defects. Proc Natl Acad Sci USA. 2011;108:12770–5.
Kim KH, Jahan SA, Kabir E, Brown RJC. A review of airborne polycyclic aromatic hydrocarbons (PAHs) and their human health effects. Environ Int. 2013;60:71–80.
Strickland P, Kang D, Sithisarankul P. Polycyclic aromatic hydrocarbon metabolites in urine as biomarkers of exposure and effect. Environ Health Perspect. 1996;104:927–32.
Poursafa P, Amin MM, Hajizadeh Y, Mansourian M, Pourzamani H, Ebrahim K, et al. Association of atmospheric concentrations of polycyclic aromatic hydrocarbons with their urinary metabolites in children and adolescents. Environ Sci Pollut Res. 2017;24:17136–44.
Gong J, Zhu T, Kipen H, Rich DQ, Huang W, Lin WT, et al. Urinary polycyclic aromatic hydrocarbon metabolites as biomarkers of exposure to traffic-emitted pollutants. Environ Int. 2015;85:104–10.
Llop S, Ballester F, Estarlich M, Ibarluzea J, Manrique A, Rebagliato M, et al. Urinary 1-hydroxypyrene, air pollution exposure and associated life style factors in pregnant women. Sci Total Environ. 2008;407:97–104.
Gearhart-Serna LM, Tacam M, Slotkin TA, Devi GR. Analysis of polycyclic aromatic hydrocarbon intake in the US adult population from NHANES 2005–2014 identifies vulnerable subpopulations, suggests interaction between tobacco smoke exposure and sociodemographic factors. Environ Res. 2021;201:111614.
Cathey A, Ferguson KK, McElrath TF, Cantonwine DE, Pace G, Alshawabkeh A, et al. Distribution and predictors of urinary polycyclic aromatic hydrocarbon metabolites in two pregnancy cohort studies. Environ Pollut. 2018;232:556–62.
Salami F, Hajizadeh Y, Yadegarfar G, Ebrahimpour K, Pourzamani H, Poursafa P. Urinary levels of PAH metabolites in pregnant women and their correlation with sociodemographic factors and PM2.5 exposure in an urban and a suburban area. Air Qual Atmos Heal. 2021;14:653–65.
Zhu J, Zhao X, Yang M, Zheng B, Sun C, Zou X, et al. Levels of urinary metabolites of benzene compounds, trichloroethylene, and polycyclic aromatic hydrocarbons and their correlations with socioeconomic, demographic, dietary factors among pregnant women in six cities of China. Environ Sci Pollut Res. 2022;29:6278–93.
Liu J, Clark LP, Bechle MJ, Hajat A, Kim SY, Robinson AL, et al. Disparities in Air Pollution Exposure in the United States by Race/Ethnicity and Income, 1990-2010. Environ Health Perspect. 2021;129:127005.
Hajat A, Hsia C, O’Neill MS. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Curr Environ Heal Rep. 2015;2:440–50.
O’Connor T, Best M, Brunner J, Ciesla AA, Cunning A, Kapula N, et al. Cohort profile: Understanding Pregnancy Signals and Infant Development (UPSIDE): A pregnancy cohort study on prenatal exposure mechanisms for child health. BMJ Open. 2021;11:e044798.
Kuiper JR, O’Brien KM, Ferguson KK, Buckley JP. Urinary specific gravity measures in the U.S. population: Implications for the adjustment of non-persistent chemical urinary biomarker data. Environ Int. 2021;156:106656.
Vollmar AKR, Rattray NJW, Cai Y, Santos-Neto ÁJ, Deziel NC, Jukic AMZ, et al. Normalizing untargeted periconceptional urinary metabolomics data: A comparison of approaches. Metabolites. 2019;9:198.
Wang Y, Hopke PK, Xia X, Rattigan OV, Chalupa DC, Utell MJ. Source apportionment of airborne particulate matter using inorganic and organic species as tracers. Atmos Environ. 2012;55:525–32.
Wang Y, Hopke PK, Rattigan OV, Chalupa DC, Utell MJ. Multiple-year black carbon measurements and source apportionment using Delta-C in Rochester, New York. J Air Waste Manag Assoc. 2012;62:880–7.
Hooper D, Coughlan J, Mullen MR. Structural equation modelling: Guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60.
Dominici F, Schwartz J, Di Q, Braun D, Choirat C, Zanobetti A. Assessing Adverse Health Effects of Long-Term Exposure to Low Levels of Ambient Air Pollution: Phase 1. Res Rep. Health Eff Inst. 2019;2022:1–51.
Di Q, Wang Y, Zanobetti A, Wang Y, Koutrakis P, Choirat C, et al. Air Pollution and Mortality in the Medicare Population. N Engl J Med. 2017;376:2513–22.
John EM, Koo J, Ingles SA, Keegan TH, Nguyen JT, Thomsen C, et al. Predictors of urinary polycyclic aromatic hydrocarbon metabolites in girls from the San Francisco Bay Area. Environ Res. 2022;205:112534.
Shahsavani S, Fararouei M, Soveid M, Dehghani M, Hoseini M. Exposure to polycyclic aromatic hydrocarbon-induced oxidative stress in Shiraz, Iran: urinary levels, health risk assessment and mediation effect of MDA on the risk of metabolic syndromes. Int Arch Occup Environ Health. 2022;95:1043–58.
Fernández SF, Pardo O, Hernández CS, Garlito B, Yusà V. Children’s exposure to polycyclic aromatic hydrocarbons in the Valencian Region (Spain): Urinary levels, predictors of exposure and risk assessment. Environ Int. 2021;153:106535.
Thai PK, Banks APW, Toms LML, Choi PM, Wang X, Hobson P, et al. Analysis of urinary metabolites of polycyclic aromatic hydrocarbons and cotinine in pooled urine samples to determine the exposure to PAHs in an Australian population. Environ Res. 2020;182:109048.
Liu S, Liu Q, Ostbye T, Story M, Deng X, Chen Y, et al. Levels and risk factors for urinary metabolites of polycyclic aromatic hydrocarbons in children living in Chongqing, China. Sci Total Environ. 2017;598:553–61.
Chen YT, Huang YK, Luvsan ME, Gombojav E, Ochir C, Bulgan J, et al. The influence of season and living environment on children’s urinary 1-hydroxypyrene levels in Ulaanbaatar, Mongolia. Environ Res. 2015;137:170–5.
Zhang YJ, Huang C, Lv YS, Ma SX, Guo Y, Zeng EY. Polycyclic aromatic hydrocarbon exposure, oxidative potential in dust, and their relationships to oxidative stress in human body: A case study in the indoor environment of Guangzhou, South China. Environ Int. 2021;149:106405.
Alhamdow A, Zettergren A, Kull I, Hallberg J, Andersson N, Ekström S, et al. Low-level exposure to polycyclic aromatic hydrocarbons is associated with reduced lung function among Swedish young adults. Environ Res. 2021;197:111169.
Lin Y, Qiu X, Yu N, Yang Q, Araujo JA, Zhu Y. Urinary Metabolites of Polycyclic Aromatic Hydrocarbons and the Association with Lipid Peroxidation: A Biomarker-Based Study between Los Angeles and Beijing. Environ Sci Technol. 2016;50:3738–45.
Hudda N, Gould T, Hartin K, Larson TV, Fruin SA. Emissions from an international airport increase particle number concentrations 4-fold at 10 km downwind. Environ Sci Technol. 2014;48:6628–35.
Masiol M, Hopke PK, Felton HD, Frank BP, Rattigan OV, Wurth MJ, et al. Analysis of major air pollutants and submicron particles in New York City and Long Island. Atmos Environ. 2017;148:203–14.
Austin E, Xiang J, Gould TR, Shirai JH, Yun S, Yost MG, et al. Distinct ultrafine particle profiles associated with aircraft and roadway traffic. Environ Sci Technol. 2021;55:2847–58.
Riley EA, Gould T, Hartin K, Fruin SA, Simpson CD, Yost MG, et al. Ultrafine particle size as a tracer for aircraft turbine emissions. Atmos Environ. 2016;139:20–9.
Hudda N, Simon MC, Zamore W, Brugge D, Durant JL. Aviation Emissions Impact Ambient Ultrafine Particle Concentrations in the Greater Boston Area. Environ Sci Technol. 2016;50:8514–21.
Jeong CH, Traub A, Evans GJ. Exposure to ultrafine particles and black carbon in diesel-powered commuter trains. Atmos Environ. 2017;155:46–52.
Tunno BJ, Tripathy S, Kinnee E, Michanowicz DR, Shmool JLC, Cambal L, et al. Fine-scale source apportionment including diesel-related elemental and organic constituents of PM2.5 across downtown Pittsburgh. Int J Environ Res Public Health. 2018;15:2177.
Wing SE, Larson TV, Hudda N, Boonyarattaphan S, Fruin S, Ritz B. Preterm birth among infants exposed to in utero ultrafine particles from aircraft emissions. Environ Health Perspect. 2020;128:047002.
Yang Z, Lin Y, Wang S, Liu X, Cullinan P, Chung KF, et al. Urinary Amino-Polycyclic Aromatic Hydrocarbons in Urban Residents: Finding a Biomarker for Residential Exposure to Diesel Traffic. Environ Sci Technol. 2021;55:10569–77.
Karner AA, Eisinger DS, Niemeier DA. Near-roadway air quality: Synthesizing the findings from real-world data. Environ Sci Technol. 2010;44:5334–44.
Eiguren-Fernandez A, Avol EL, Thurairatnam S, Hakami M, Froines JR, Miguel AH. Seasonal influence on vapor- and particle-phase polycyclic aromatic hydrocarbon concentrations in school communities located in Southern California. Aerosol Sci Technol. 2007;41:438–46.
Wei C, Bandowe BAM, Han Y, Cao J, Watson JG, Chow JC, et al. Polycyclic aromatic compounds (PAHs, oxygenated PAHs, nitrated PAHs, and azaarenes) in air from four climate zones of China: Occurrence, gas/particle partitioning, and health risks. Sci Total Environ. 2021;786:147234.
Lin Y, Ma Y, Qiu X, Li R, Fang Y, Wang J, et al. Sources, transformation, and health implications of PAHs and their nitrated, hydroxylated, and oxygenated derivatives in PM2.5 in Beijing. J Geophys Res. 2015;120:7219–28.
Houston D, Wu J, Ong P, Winer A. Structural disparities of urban traffic in Southern California: Implications for vehicle-related air pollution exposure in minority and high-poverty neighborhoods. J Urban Aff. 2004;26:565–92.
Do EK, Green TL, Prom-Wormley EC, Fuemmeler BF. Social determinants of smoke exposure during pregnancy: Findings from waves 1 & 2 of the Population Assessment of Tobacco and Health (PATH) Study. Prev Med Rep. 2018;12:312–20.
Wheeler DC, Boyle J, Jeremy Barsell D, Maguire RL, Zhang J (Jim), Oliver JA, et al. Tobacco Retail Outlets, Neighborhood Deprivation and the Risk of Prenatal Smoke Exposure. Nicotine Tob Res. 2022;24:2003–10.
Zhang Y, Ding J, Shen G, Zhong J, Wang C, Wei S, et al. Dietary and inhalation exposure to polycyclic aromatic hydrocarbons and urinary excretion of monohydroxy metabolites - A controlled case study in Beijing, China. Environ Pollut. 2014;184:515–22.
Lin Y, Zhu Y, Qiu X, Lu X, Yin F, Tseng CH, et al. Passive smoking and urinary oxidative biomarkers: A pilot study of healthy travelers from Los Angeles to Beijing. Int J Hyg Environ Health. 2022;246:114048.
Acknowledgements
Special thanks to Kelly Thevenet-Morrison for her assistance in data management.
Funding
This study is funded by National Institutes of Health (R01ES027495, UG3 OD023349, HD083369), The Wynne Center for Family Research. The project described in this publication was supported by the University of Rochester CTSA award number UL1 TR002001 from the National Center for Advancing Translational Sciences of the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
Conceptualization: YL, JZ, and DR; Subject recruitment and sample collection: BJ, TO’C; Laboratory analysis: YL, EC, XL, YG, ZY, and XW; Data analysis: YL, EC, and ST; Writing—Original draft preparation: YL and EC; Writing—Reviewing and Editing: YL, EC, XL, YG, BJ, XW, ZY, PH, RM, EB, ST, SM, TO’C, DQ, and JZ; Supervision: JZ and DR; Fund acquisitions: JZ and DR.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the University of Rochester Research Subjects Review Board and the Institutional Review Board of Duke University. All participants provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, Y., Craig, E., Liu, X. et al. Urinary 1-hydroxypyrene in pregnant women in a Northeastern U.S. city: socioeconomic disparity and contributions from air pollution sources. J Expo Sci Environ Epidemiol 34, 407–415 (2024). https://doi.org/10.1038/s41370-023-00555-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-023-00555-9
Keywords
This article is cited by
-
Urinary polycyclic aromatic hydrocarbon metabolites and their association with oxidative stress among pregnant women in Los Angeles
Environmental Health (2024)
-
Maternal and newborn metabolomic changes associated with urinary polycyclic aromatic hydrocarbon metabolite concentrations at delivery: an untargeted approach
Metabolomics (2023)