Abstract
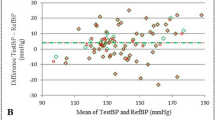
The importance of accurate blood pressure (BP) measurement is well-established. However, there is little quantitative comparative data on the influence of different measurement conditions on BP or the stability of the oscillometric pulse waveform from which BP is calculated. This study investigates the effect of six different measurement conditions (Quiet, Reading, Speaking, Deep Breathing, Moving, and Tapping) on BP readings in 30 healthy normotensive subjects. We hypothesize that non-standard conditions will result in significant deviations in BP measurements compared to the Quiet condition. Additionally, the quality and stability of the oscillometric waveform were assessed by evaluating the smoothness of the oscillometric pulse waveform characteristics during cuff deflation. Compared with the Quiet condition, all others resulted in significantly higher blood pressures, except for the respiratory condition, which resulted in significantly lower BPs. Average subject systolic BP (SBP) rose from 117.4 ± 6.0 mmHg for the Quiet condition to 129.7 ± 7.2 mmHg for the light finger tapping condition, P < 0.00001. Overall, changes for diastolic BP (DBP) were not significant. For the quality Noise indicator, all conditions in comparison with the Quiet condition were significantly noisier, increasing from 0.144 ± 0.024 to 1.055 ± 0.308 mmHg, P < 0.00001. Changes in SBP were significantly correlated to changes in quality Noise (r = 0.965, P < 0.001). This study confirms the importance of following international BP measurement guidelines, providing quantitative data showing significant changes in BP when guidelines are not followed. A method for assessing the quality of the measurement is also demonstrated, and shows that BP changes are significantly related to changes in the quality indicator.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding authors upon request.
References
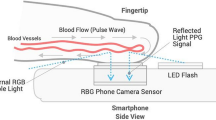
Shalom E, Hirshtal E, Slotki I, Shavit L, Yitzhaky Y, Engelberg S, et al. Systolic blood pressure measurement by detecting the photoplethysmographic pulses and electronic Korotkoff-sounds during cuff deflation. Physiol Meas. 2020;41:034001.
Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. Recommendations for blood pressure measurement in humans and experimental animals - Part 1: Blood pressure measurement in humans - A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716.
Palafox B, Goryakin Y, Stuckler D, Suhrcke M, Balabanova D, Alhabib KF, et al. Does greater individual social capital improve the management of hypertension? Cross-national analysis of 61 229 individuals in 21 countries. BMJ Glob Health. 2017;2:e000443.
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365:217–23.
Herakova N, Nwobodo NHN, Wang Y, Chen F, Zheng D. Effect of respiratory pattern on automated clinical blood pressure measurement: an observational study with normotensive subjects. Clin Hypertens. 2017;23:15.
Liu J, Hu SC, Xiao ZJ, Hu QH, Wang DM, Yang CW. A novel interpretable feature set optimization method in blood pressure estimation using photoplethysmography signals. Biomed Signal Process Control. 2023;86:105184.
Ding XR, Zhang YT, Tsang HK. Impact of heart disease and calibration interval on accuracy of pulse transit time-based blood pressure estimation. Physiol Meas. 2016;37:227–37.
Jones DW, Appel LJ, Sheps SG, Roccella EJ, Lenfant C. Measuring blood pressure accurately - New and persistent challenges. JAMA. 2003;289:1027–30.
Pa F, He PY, Che F, Zhan J, Wan H, Zhen DC. A novel deep learning based automatic auscultatory method to measure blood pressure. Int J Med Inform. 2019;128:71–78.
Liu CY, Griffiths C, Murray A, Zheng DC. Comparison of stethoscope bell and diaphragm, and of stethoscope tube length, for clinical blood pressure measurement. Blood Press Monit. 2016;21:178–83.
Celler BG, Le P, Basilakis J, Ambikairajah E. Improving the quality and accuracy of non-invasive blood pressure measurement by visual inspection and automated signal processing of the Korotkoff sounds. Physiol Meas. 2017;38:1006–22.
White WB, Berson AS, Robbins C, Jamieson MJ, Prisant LM, Roccella E, et al. National standard for measurement of resting and ambulatory blood pressures with automated sphygmomanometers. Hypertension. 1993;21:504–9.
Kessler R. The Minamata Convention on Mercury: a first step toward protecting future generations. Environ Health Perspect. 2013;121:A304–A9.
Yang FW, Chen F, Zhu MP, Chen AQ, Zheng DC. Significantly reduced blood pressure measurement variability for both normotensive and hypertensive subjects: effect of polynomial curve fitting of oscillometric pulses. Biomed Res Int. 2017;1:5201069.
Forouzanfar M, Dajani HR, Groza VZ, Bolic M, Rajan S, Batkin I. Oscillometric blood pressure estimation: past, present, and future. IEEE Rev Biomed Eng. 2015;8:44–63.
Liu C, Zheng D, Griffiths C, Murray A Oscillometric waveform difference between cuff inflation and deflation during blood pressure measurement. In 2014 Computing in Cardiology Conference. 2014; 849–52.
Fonseca-Reyes S, Fajardo-Flores I, Montes-Casillas M, Forsyth-MacQuarrie A. Differences and effects of medium and large adult cuffs on blood pressure readings in individuals with muscular arms. Blood Press Monit. 2009;14:166–71.
Lee S, Chang JH, Nam SW, Lim C, Rajan S, Dajani HR, et al. Oscillometric blood pressure estimation based on maximum amplitude algorithm employing gaussian mixture regression. IEEE Trans Instrum Meas. 2013;62:3387–9.
Liu J, Li YM, Li JQ, Zheng DC, Liu CY. Sources of automatic office blood pressure measurement error: a systematic review. Physiol Meas. 2022;43:09TR02.
Beevers G, Lip GYH, O’Brien E. ABC of hypertension - Blood pressure measurement Part II - Conventional sphygmomanometry: technique of auscultatory blood pressure measurement. BMJ-Br Med J. 2001;322:1043–7.
O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, et al. European Society of hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–48.
Zheng D, Liu C, Amoore J, Mieke S, Murray A. Need for re-validation of automated blood pressure devices for use in unstable conditions. Comput Cardiol Conf. 2015;2015:17–20.
Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in themeasurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens. 2017;35:421–41.
Familoni OB, Olunuga TO. Comparison of the effects of arm position and support on blood pressure in hypertensive and normotensive subjects: cardiovascular topic. Cardiovasc J South Afr. 2005;16:85–88.
Eşer İ, Khorshid L, Yapucu Güneş Ü, Demir Y. The effect of different body positions on blood pressure. J Clin Nurs. 2007;16:137–40.
Pinar R, Ataalkin S, Watson R. The effect of crossing legs on blood pressure in hypertensive patients. J Clin Nurs. 2010;19:1284–8.
Zheng D, Giovannini R, Murray A. Effect of respiration, talking and small body movements on blood pressure measurement. J Hum Hypertens. 2012;26:458–62.
Le Pailleur C, Montgermont P, Feder JM, Metzger JP, Vacheron A. Talking effect and “white coat” effect in hypertensive patients: physical effort or emotional content? Behav Med. 2001;26:149–57.
Laude D, Goldman M, Escourrou P, Elghozi JL. Effect of breathing pattern on blood pressure and heart rate oscillations in humans. Clin Exp Pharmacol Physiol. 1993;20:619–26.
Pan F, He PY, Chen F, Pu XB, Zhao QJ, Zheng DC. Deep learning-based automatic blood pressure measurement: evaluation of the effect of deep breathing, talking and arm movement. Ann Med. 2019;51:397–403.
Liu J, Murray A, Li J, Liu C Influence of finger movement on the stability of the oscillometric pulse waveform for blood pressure measurement. In 2021 Computing in Cardiology Conference. 2021; 48: 1–4.
Kurtz TW, Griffin KA, Bidani AK, Davisson RL, Hall JE. Recommendations for blood pressure measurement in humans and experimental animals - Part 2: Blood pressure measurement in experimental animals - A statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Hypertension. 2005;45:299–310.
Williams B, Poulter NR, Brown MJ, Davis M, McInnes GT, Potter JF, et al. Guidelines for management of hypertension: Report of the fourth working party of the British Hypertension Society, 2004 - BHSIV. J Hum Hypertens. 2004;18:139–85.
Zheng DC, Amoore JN, Mieke S, Murray A. How important is the recommended slow cuff pressure deflation rate for blood pressure measurement? Ann Biomed Eng. 2011;39:2584–91.
Yong PG, Geddes LA. The effect of cuff pressure deflation rate on accuracy in indirect measurement of blood pressure with the auscultatory method. J Clin Monit. 1987;3:155–9.
Cahan A, Ben-Dov IZ, Bursztyn M. Association of heart rate with blood pressure variability: implications for blood pressure measurement. Am J Hypertens. 2012;25:313–8.
Murray A, Zheng D. Newcastle University of Upon Tyne. Improved sphygmomanometer capable of displaying the quality of blood pressure readings. U S Pat Appl 2016;14/902:028.
Acknowledgements
We would like to thank all the volunteers who participated in this study.
Funding
This research was funded by the National Natural Science Foundation of China (62171123), the National Key Research and Development Program of China (2023YFC3603600), the Engineering and Physical Sciences Research Council (EPSRC) UK (EP/N025342/1, EP/I027270/1 and EP/F012764/1).
Author information
Authors and Affiliations
Contributions
CYL revised the paper and participated in the experiments. JL collected and analysed the data with the support of CYL and JQL. JQL provided the venue and guided the experiments. AM guided the experiments. CYL and AM designed the experiments and drafted the paper. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
None declared. The patent for the technique is cited in the paper, but as yet there is no commercial agreement.
Ethics Statement
The investigation conformed with the Declaration of Helsinki, and all subjects gave their written informed consent to participate in the study. Ethical approval was granted by the Independent Ethics Committee (IEC) for Clinical Research of Zhongda Hospital, affiliated with Southeast University, under approval number 2021ZDSYLL206-P01.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, C., Liu, J., Li, J. et al. Preventing troublesome variability in clinical blood pressure measurement. J Hum Hypertens 39, 72–77 (2025). https://doi.org/10.1038/s41371-024-00978-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-024-00978-3