Abstract
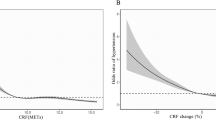
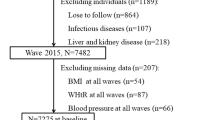
This study investigated the association between fat-to-muscle ratio (FMR) and hypertension. A total of 1592 participants aged ≥ 40 years were included. Participants were divided into four groups by quartiles of FMR. Odds ratio (OR) and 95% confidence interval (CI) was calculated using logistic regression models. Restricted cubic spline was applied to examine the correlation of FMR and hypertension. Of 1592 participants, 943 (59.2%) participants had hypertension. Hypertension risk rose with FMR quartiles. Compared to FMR quartile 1, ORs were 1.496 (95% CI: 1.115–2.006), 2.445 (95% CI: 1.840–3.249), and 5.415 (95% CI: 3.993–7.344) for quartiles 2, 3, and 4, respectively (P for trend < 0.001). Adjusted OR in quartile 4 was 3.015 (95% CI: 2.083–4.365). Restricted cubic spline showed a linear relationship between FMR and hypertension. Adding FMR improved hypertension risk model performance (P = 0.006). Subgroup analysis revealed FMR interactions with sex (P = 0.010) and BMI (P < 0.016), with a higher hypertension risk in females and non-obese individuals. Additionally, versus FMR quartile 1, hypertensive individuals in quartiles 2 (OR: 1.370, 95% CI: 0.900–2.085), 3 (OR: 2.055, 95% CI: 1.374–3.073) and 4 (OR: 3.102, 95% CI: 2.055–4.682) exhibited a significantly elevated risk of atherosclerotic cardiovascular disease (ASCVD). In summary, Elevated FMR independently correlated with hypertension risk, especially in women, or even in non-obese individuals. FMR is a valuable tool for identifying populations with higher hypertension risk and assessing ASCVD risk in hypertensive individuals. Body composition warrants consideration in future hypertension risk studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The original data of this study are available from Dryad Digital Repository (https://datadryad.org).
References
Mills KT, Stefanescu A, He J. The global epidemiology of hypertension. Nat Rev Nephrol. 2020;16:223–37.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390:2549–58.
Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021;18:785–802.
The Lancet Neurology. The global challenge of hypertension. Lancet Neurol. 2023;22:1087.
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–50.
Reisin E, Jack AV. Obesity and hypertension: mechanisms, cardio-renal consequences, and therapeutic approaches. Med Clin North Am. 2009;93:733–51.
Zeng Q, Sun L, Zeng Q. Trajectories of mid-life to elderly adulthood BMI and incident hypertension: the China Health and Nutrition Survey. BMJ Open. 2021;11:e047920.
Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, et al. Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Clin Nutr. 2022;41:990–1000.
Park SH, Park JH, Song PS, Kim DK, Kim KH, Seol SH, et al. Sarcopenic obesity as an independent risk factor of hypertension. J Am Soc Hypertens. 2013;7:420–5.
Ramirez-Velez R, Carrillo HA, Correa-Bautista JE, Schmidt-RioValle J, Gonzalez-Jimenez E, Correa-Rodriguez M, et al. Fat-to-Muscle ratio: a new anthropometric indicator as a screening tool for metabolic syndrome in young Colombian people. Nutrients. 2018;10:1027.
Liu D, Zhong J, Ruan Y, Zhang Z, Sun J, Chen H. The association between fat-to-muscle ratio and metabolic disorders in type 2 diabetes. Diabetol Metab Syndr. 2021;13:129.
Eun Y, Lee SN, Song SW, Kim HN, Kim SH, Lee YA, et al. Fat-to-muscle ratio: a new indicator for coronary artery disease in healthy adults. Int J Med Sci. 2021;18:3738–43.
Gortan Cappellari G, Guillet C, Poggiogalle E, Ballesteros Pomar MD, Batsis JA, Boirie Y, et al. Sarcopenic obesity research perspectives outlined by the sarcopenic obesity global leadership initiative (SOGLI) - proceedings from the SOGLI consortium meeting in rome November 2022. Clin Nutr. 2023;42:687–99.
Yan F, Nie G, Zhou N, Zhang M, Peng W. Association of fat-to-muscle ratio with non-alcoholic fatty liver disease: a single-centre retrospective study. BMJ Open. 2023;13:e072489.
Fang Q, Zhu G, Huang J, Pan S, Fang M, Li Q, et al. Current status of sarcopenia in the disabled elderly of chinese communities in Shanghai: based on the updated EWGSOP consensus for sarcopenia. Front Med. 2020;7:552415.
Zeng P, Wu S, Han Y, Liu J, Zhang Y, Zhang E, et al. Differences in body composition and physical functions associated with sarcopenia in chinese elderly: reference values and prevalence. Arch Gerontol Geriatr. 2015;60:118–23.
Sun Q, Cui J, Liu W, Li J, Hong M, Qian S. The prognostic value of sarcopenia in acute myeloid leukemia patients and the development and validation of a novel nomogram for predicting survival. Front Oncol. 2022;12:828939.
Zhu J, Zhang Y, Wu Y, Xiang Y, Tong X, Yu Y, et al. Obesity and dyslipidemia in chinese adults: A Cross-Sectional Study in Shanghai, China. Nutrients. 2022;14:2321.
Andrus B, Lacaille D. 2013 ACC/AHA guideline on the assessment of cardiovascular risk. J Am Coll Cardiol. 2014;63:2886.
Ittermann T, Werner N, Lieb W, Merz B, Nothlings U, Kluttig A, et al. Changes in fat mass and fat-free-mass are associated with incident hypertension in four population-based studies from Germany. Int J Cardiol. 2019;274:372–7.
Sato F, Maeda N, Yamada T, Namazui H, Fukuda S, Natsukawa T, et al. Association of epicardial, visceral, and subcutaneous fat with cardiometabolic diseases. Circ J. 2018;82:502–8.
Goto K, Yokokawa H, Fukuda H, Saita M, Hamada C, Hisaoka T, et al. An association between subcutaneous fat mass accumulation and hypertension. J Gen Fam Med. 2021;22:209–17.
Takase M, Nakamura T, Tsuchiya N, Kogure M, Itabashi F, Narita A, et al. Association between the combined fat mass and fat-free mass index and hypertension: The Tohoku Medical Megabank Community-based Cohort Study. Clin Exp Hypertens. 2021;43:610–21.
Lee SB, Cho AR, Kwon YJ, Jung DH. Body fat change and 8-year incidence of hypertension: Korean Genome and Epidemiology Study. J Clin Hypertens. 2019;21:1849–57.
Jurdana M, Ziberna L. Sarcopenic obesity and hypertension in elderly patients: a narrative review of pathophysiology and management strategies. Ann Ist Super Sanita. 2023;59:231–9.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Butcher JT, Mintz JD, Larion S, Qiu S, Ruan L, Fulton DJ, et al. Increased muscle mass protects against hypertension and renal injury in obesity. J Am Heart Assoc. 2018;7:e009358.
Gao LW, Huang YW, Cheng H, Wang X, Dong HB, Xiao P, et al. Prevalence of hypertension and its associations with body composition across chinese and american children and adolescents. World J Pediatr. 2024;20:392–403.
Chen YY, Fang WH, Wang CC, Kao TW, Yang HF, Wu CJ, et al. Fat-to-muscle ratio is a useful index for cardiometabolic risks: a population-based observational study. PLoS One. 2019;14:e0214994.
Park SK, Ryoo JH, Oh CM, Choi JM, Chung PW, Jung JY. Body fat percentage, obesity, and their relation to the incidental risk of hypertension. J Clin Hypertens. 2019;21:1496–504.
Yan F, Nie G, Zhou N, Zhang M, Peng W. Combining fat-to-muscle ratio and alanine aminotransferase/aspartate aminotransferase ratio in the prediction of cardiometabolic risk: A Cross-Sectional Study. Diabetes Metab Syndr Obes. 2023;16:795–806.
Jayant SS, Gupta R, Rastogi A, Agrawal K, Sachdeva N, Ram S, et al. Abdominal obesity and incident cardio-metabolic disorders in Asian-Indians: A 10-years prospective cohort study. Diabetes Metab Syndr. 2022;16:102418.
Marra M, Sammarco R, De Lorenzo A, Iellamo F, Siervo M, Pietrobelli A, et al. Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-Ray absorptiometry (DXA): a critical overview. Contrast Media Mol Imaging. 2019;2019:3548284.
Acknowledgements
The authors appreciate Yan F, Peng W et al. for sharing the data for secondary analysis.
Author information
Authors and Affiliations
Contributions
LX and ZC were responsible for manuscript writing and data analysis. YC conceived and supervised the study. DG and YC contributed to literature search and methodology. HS performed the manuscript review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The original study, the source of our research data, involved human participants and was approved by the Institutional Review Board of Tongji Medical College, Huazhong University of Science and Technology. The protocol of this study was approved by the Ethics Committee of Cancer Hospital of Shantou University Medical College. No informed consent was required because the study was conducted retrospectively and anonymized.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Z., Guo, D., Xiao, L. et al. Association of fat-to-muscle ratio with hypertension: a cross-sectional study in China. J Hum Hypertens 39, 301–307 (2025). https://doi.org/10.1038/s41371-025-00992-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-025-00992-z