Abstract
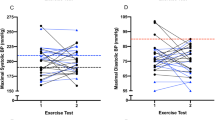
The American Heart Association recommends sex-specific thresholds for defining exaggerated systolic blood pressure response to exercise (ESBPR), primarily based on data from young healthy populations. However, their applicability and the sex differences in systolic blood pressure (SBP) response to exercise in real-world clinical settings remain unclear. We conducted a cross-sectional study of 44 418 adults (40.6% female) with a mean age of 49, who underwent treadmill exercise testing at Fuwai Hospital from 2016–2022. ESBPR was defined as peak SBP during exercise ≥ 210 mmHg for males and ≥ 190 mmHg for females. Multivariate regression models stratified by sex were used to explore whether sex modifies age-related patterns in SBP response to exercise. ESBPR was over five times more prevalent in females than males (10.1 vs. 1.9%, P < 0.001). While the mean, 90th, and 95th percentiles of peak SBP were at least 12 mmHg higher in males than females in younger age groups (18–44), the gap narrowed to less than 4 mmHg in older age groups (≥45). Stratified multivariate analysis revealed that age was a strong predictor of ESBPR in females but not in males. Using age ≥ 51 as a proxy for menopause, females older than 51 had significantly higher odds of ESBPR compared to younger females (adjusted OR: 1.904, 95% CI: 1.683–2.155, P < 0.001). Our findings reveal that females and males display distinct age-related patterns in SBP response to exercise. The lower threshold for females may disproportionately classify postmenopausal females as abnormal.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Public data is not applicable to this study. Study data are available from the corresponding author upon reasonable request.
References
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: a scientific statement from the American heart association. Circulation. 2013;128:873–934.
Singh JP, Larson MG, Manolio TA, O’Donnell CJ, Lauer M, Evans JC, et al. Blood pressure response during treadmill testing as a risk factor for new-onset hypertension. The Framingham heart study. Circulation. 1999;99:1831–6.
Ito K, Iwane M, Miyai N, Uchikawa Y, Mugitani K, Mohara O, et al. Exaggerated exercise blood pressure response in middle-aged men as a predictor of future blood pressure: a 10-year follow-up. Clin Exp Hypertens. 2016;38:696–700.
Kohl HW 3rd, Nichaman MZ, Frankowski RF, Blair SN. Maximal exercise hemodynamics and risk of mortality in apparently healthy men and women. Med Sci Sports Exerc. 1996;28:601–9.
Percuku L, Bajraktari G, Jashari H, Bytyci I, Ibrahimi P, Henein MY. Exaggerated systolic hypertensive response to exercise predicts cardiovascular events: a systematic review and meta-analysis. Pol Arch Intern Med. 2019;129:855–63.
Pelliccia A, Sharma S, Gati S, Back M, Borjesson M, Caselli S, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17–96.
Gary L, Feito Y, Fountaine C, Roy BA. American college of sports Medicine’s guidelines for exercise testing and prescription. Eleventh ed. Philadelphia: Wolters Kluwer; 2021.
Lauer MS, Levy D, Anderson KM, Plehn JF. Is there a relationship between exercise systolic blood pressure response and left ventricular mass? The Framingham Heart Study. Ann Intern Med. 1992;116:203–10.
Le VV, Mitiku T, Sungar G, Myers J, Froelicher V. The blood pressure response to dynamic exercise testing: a systematic review. Prog Cardiovasc Dis. 2008;51:135–60.
Daida H, Allison TG, Squires RW, Miller TD, Gau GT. Peak exercise blood pressure stratified by age and gender in apparently healthy subjects. Mayo Clin Proc. 1996;71:445–52.
Jiao J, Hao J, Hou L, Luo Z, Shan S, Ding Y, et al. Age at natural menopause and associated factors with early and late menopause among Chinese women in Zhejiang province: a cross-sectional study. PLoS ONE. 2024;19:e0307402.
Sabbahi A, Arena R, Kaminsky LA, Myers J, Phillips SA. Peak blood pressure responses during maximum cardiopulmonary exercise testing: reference standards from FRIEND (fitness registry and the importance of exercise: a national database). Hypertension. 2018;71:229–36.
Assaf Y, Barout A, Alhamid A, Al-Mouakeh A, Barillas-Lara MI, Fortin-Gamero S, et al. Peak systolic blood pressure during the exercise test: reference values by sex and age and association with mortality. Hypertension. 2021;77:1906–14.
El Khoudary SR, Aggarwal B, Beckie TM, Hodis HN, Johnson AE, Langer RD, et al. Menopause transition and cardiovascular disease risk: implications for timing of early prevention: a scientific statement from the American heart association. Circulation. 2020;142:e506–e532.
Stewart KJ, Sung J, Silber HA, Fleg JL, Kelemen MD, Turner KL, et al. Exaggerated exercise blood pressure is related to impaired endothelial vasodilator function. Am J Hypertens. 2004;17:314–20.
Shim CY, Ha JW, Park S, Choi EY, Choi D, Rim SJ, et al. Exaggerated blood pressure response to exercise is associated with augmented rise of angiotensin II during exercise. J Am Coll Cardiol. 2008;52:287–92.
Kim CH, Park Y, Chun MY, Kim YJ. Exercise-induced hypertension is associated with angiotensin II activity and total nitric oxide. Medicine. 2020;99:e20943.
Reslan OM, Khalil RA. Vascular effects of estrogenic menopausal hormone therapy. Rev Recent Clin Trials. 2012;7:47–70.
Saleh TM, Connell BJ. Role of oestrogen in the central regulation of autonomic function. Clin Exp Pharmacol Physiol. 2007;34:827–32.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines. Circulation. 2019;140:e563–e95.
Klonizakis M, Moss J, Gilbert S, Broom D, Foster J, Tew GA. Low-volume high-intensity interval training rapidly improves cardiopulmonary function in postmenopausal women. Menopause. 2014;21:1099–105.
Huynh E, Wiley E, Noguchi KS, Fang H, Beauchamp MK, MacDonald MJ, et al. The effects of aerobic exercise on cardiometabolic health in postmenopausal females: a systematic review and meta-analysis of randomized controlled trials. Womens Health. 2024;20:17455057241290889.
Manolio TA, Burke GL, Savage PJ, Sidney S, Gardin JM, Oberman A. Exercise blood pressure response and 5-year risk of elevated blood pressure in a cohort of young adults: the CARDIA study. Am J Hypertens. 1994;7:234–41.
Acknowledgements
The authors express our gratitude to all the participants who took part in the treadmill exercise tests in our study. The authors also greatly appreciate the dedicated staff of the Department of Cardiac Function Test Center, Fuwai Hospital for their expertise and commitment in conducting the treadmill exercise tests with precision and care.
Funding
This research was supported by the National High Level Hospital Clinical Research Funding (2022-GSP-GG-014).
Author information
Authors and Affiliations
Contributions
Shengming Li: Conceptualization, Formal analysis, Methodology, Writing—original draft. Tianjing Zhang: Formal analysis, Writing—original draft. Jia He: Data collection. Chen He: Data collection. Fang Liu: Formal analysis. Yan Yao: Conceptualization, Supervision. Xiaofei Li: Data collection, Writing—review and editing. Rutai Hui: Writing—review and editing. Xiaohan Fan: Conceptualization, Formal analysis, Data collection, Funding acquisition, Methodology, Project administration, Supervision, Writing—review and editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This cross-sectional study was approved by the Institutional Review Board of Fuwai Hospital, which granted a waiver of informed consent for research purposes, as the data were obtained from tests performed as part of routine clinical care rather than exclusively for research.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, S., Zhang, T., He, J. et al. Sex differences in systolic blood pressure response to exercise testing: a real-world clinical analysis. J Hum Hypertens (2025). https://doi.org/10.1038/s41371-025-01037-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41371-025-01037-1