Abstract
Objective
Remote patient monitoring (RPM) facilitates early discharge of infants with inadequate oral feeding. We aim to determine the financial impact of discharge with RPM compared to continued hospitalization.
Study design
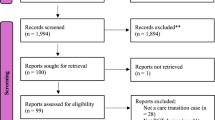
Patients discharged on RPM between May 2019 and June 2024 were eligible. Days of home nasogastric tube feeds and total physician time per episode were recorded. Direct cost estimates for each aspect of RPM and continued hospitalization were used to calculate cost savings of RPM use from a health care system perspective. One- and two-way sensitivity analyses were performed.
Results
One hundred eighty infants were included. RPM decreased the hospital stay by 9.2 days/patient (mean). An RPM episode cost $1,768.24 (mean), while hypothetical continued hospitalization cost $13,978.32 (mean); a difference of $12,210.08. Sensitivity analyses showed that inpatient hospital cost variations were the primary driver of savings.
Conclusion
RPM programs for neonates with inadequate oral feeding can reduce direct medical costs.
Clinical trial resgistration
None
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Harrison W, Goodman D. Epidemiologic trends in neonatal intensive care, 2007–2012. JAMA Pediatr. 2015;169:855–62.
Kim Y, Ganduglia-Cazaban C, Chan W, Lee M, Goodman DC. Trends in neonatal intensive care unit admissions by race/ethnicity in the United States, 2008-2018. Sci Rep. 2021;11:23795.
Outcomes IoMUCoUPBaAH. In: Behrman RE, Butler, AS, editor. Preterm Birth: Causes, Consequences, and Prevention. Washington (DC): National Academies Press (US); 2007. p. 398–429.
Phibbs CS, Schmitt SK, Cooper M, Gould JB, Lee HC, Profit J, et al. Birth hospitalization costs and days of care for mothers and Neonates in California, 2009-2011. J Pediatr. 2019;204:118–25.e14.
Ho T, Zupancic JAF, Pursley DM, Dukhovny D. Improving value in neonatal intensive care. Clin Perinatol. 2017;44:617–25.
Fisher C, Haag M, Douglas A, Kayhani A, Warren JB. Remote monitoring for neonates requiring continued nasogastric tube feeding: implementation, patient characteristics, and early outcomes. J Perinatol. 2023;43:1125–30.
Lagatta JM, Uhing M, Acharya K, Lavoie J, Rholl E, Malin K, et al. Actual and potential impact of a home nasogastric tube feeding program for infants whose neonatal intensive care unit discharge is affected by delayed oral feedings. J Pediatr. 2021;234:38–45.e2.
Lundberg B, Lindgren C, Palme-Kilander C, Ortenstrand A, Bonamy AK, Sarman I. Hospital-assisted home care after early discharge from a Swedish neonatal intensive care unit was safe and readmissions were rare. Acta Paediatr. 2016;105:895–901.
Mago-Shah DD, Malcolm WF, Greenberg RG, Goldstein RF. Discharging medically complex infants with supplemental nasogastric tube feeds: impact on neonatal intensive care unit length of stay and prevention of gastrostomy tubes. Am J Perinatol. 2021;38:e207–e14.
Schuler R, Ehrhardt H, Mihatsch WA. Safety and parental satisfaction with early discharge of preterm infants on nasogastric tube feeding and outpatient clinic follow-up. Front Pediatr. 2020;8:505.
van Kampen F, de Mol A, Korstanje J, Groof FM, van Meurs-Asseler L, Stas H, et al. Early discharge of premature infants < 37 weeks gestational age with nasogastric tube feeding: the new standard of care? Eur J Pediatr. 2019;178:497–503.
Vergales BD, Murray PD, Miller SE, Vergales JE. Safety and efficacy of a home nasogastric monitoring program for premature infants. J Neonatal Perinat Med. 2022;15:165–70.
White BR, Ermarth A, Thomas D, Arguinchona O, Presson AP, Ling CY. Creation of a standard model for tube feeding at neonatal intensive care unit discharge. JPEN J Parenter Enter Nutr. 2020;44:491–9.
Williams SL, Popowics NM, Tadesse DG, Poindexter BB, Merhar SL. Tube feeding outcomes of infants in a Level IV NICU. J Perinatol. 2019;39:1406–10.
Services CfMM. Physician Fee Schedule 2024 [Available from: https://www.cms.gov/medicare/payment/fee-schedules/physician.
Aveanna Healthcare, personal communication, 2023.
American Academy of Pediatrics Committee on F, Newborn. Hospital discharge of the high-risk neonate. Pediatrics. 2008;122:1119–26.
Edwards L, Cotten CM, Smith PB, Goldberg R, Saha S, Das A, et al. Inadequate oral feeding as a barrier to discharge in moderately preterm infants. J Perinatol. 2019;39:1219–28.
Meerlo-Habing ZE, Kosters-Boes EA, Klip H, Brand PL. Early discharge with tube feeding at home for preterm infants is associated with longer duration of breast feeding. Arch Dis Child Fetal Neonatal Ed. 2009;94:F294–7.
Bardach SH, Perry AN, Kapadia NS, Richards KE, Cogswell LK, Hartman TK. Redesigning care to support earlier discharge from a neonatal intensive care unit: a design thinking informed pilot. BMJ Open Qual. 2022;11:e001736.
Ermarth A, Ling CY. Partial enteral discharge programs for high-risk infants. Neoreviews. 2022;23:e13–e22.
Evanochko C, Jancs-Kelley S, Boyle R, Fox M, Molesky M, Byrne P. Facilitating early discharge from the NICU: the development of a home gavage program and neonatal outpatient clinic. Neonatal Netw. 1996;15:44.
Ortenstrand A, Waldenstrom U, Winbladh B. Early discharge of preterm infants needing limited special care, followed by domiciliary nursing care. Acta Paediatr. 1999;88:1024–30.
Lemelin A, Pare G, Bernard S, Godbout A. Demonstrated cost-effectiveness of a telehomecare program for gestational diabetes mellitus management. Diabetes Technol Ther. 2020;22:195–202.
Niu B, Mukhtarova N, Alagoz O, Hoppe K. Cost-effectiveness of telehealth with remote patient monitoring for postpartum hypertension. J Matern Fetal Neonatal Med. 2022;35:7555–61.
Peretz D, Arnaert A, Ponzoni NN. Determining the cost of implementing and operating a remote patient monitoring programme for the elderly with chronic conditions: a systematic review of economic evaluations. J Telemed Telecare. 2018;24:13–21.
Lanssens D, Vandenberk T, Smeets CJ, De Canniere H, Vonck S, Claessens J, et al. Prenatal remote monitoring of women with gestational hypertensive diseases: cost analysis. J Med Internet Res. 2018;20:e102.
Slotwiner D, Wilkoff B. Cost efficiency and reimbursement of remote monitoring: a US perspective. Europace. 2013;15:i54–i8.
Hagi-Pedersen MB, Dessau RB, Norlyk A, Stanchev H, Kronborg H. Comparison of video and in-hospital consultations during early in-home care for premature infants and their families: A randomised trial. J Telemed Telecare. 2022;28:24–36.
Holm KG, Clemensen J, Brodsgaard A, Smith AC, Maastrup R, Zachariassen G. Growth and breastfeeding of preterm infants receiving neonatal tele-homecare compared to hospital-based care. J Neonatal Perinat Med. 2019;12:277–84.
Gund A, Sjoqvist BA, Wigert H, Hentz E, Lindecrantz K, Bry K. A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med Inf Decis Mak. 2013;13:22.
Robinson C, Gund A, Sjoqvist BA, Bry K. Using telemedicine in the care of newborn infants after discharge from a neonatal intensive care unit reduced the need of hospital visits. Acta Paediatr. 2016;105:902–9.
Caruso CG, Warren JB, Carney PA. Parent experiences of a remote patient monitoring program enabling early discharge from the neonatal intensive care unit with nasogastric tube feeding. J Neonatal Perinat Med. 2023;16:301–9.
Quinn M, Banta-Wright S, Warren JB. Influences of a remote monitoring program of home nasogastric tube feeds on transition from NICU to home. Am J Perinatol. 2025;42:250–55.
King BC, Mowitz ME, Zupancic JAF. The financial burden on families of infants requiring neonatal intensive care. Semin Perinatol. 2021;45:151394.
Richardson D. Parents’ time is worth money. Pediatrics. 1983;71:466–7.
Acknowledgements
Thank you to the donors who made the creation of Growing @ Home a possibility and to the families for participating in our Growing @ Home studies.
Author information
Authors and Affiliations
Contributions
CRF conceptualized and designed the study, drafted the initial manuscript, and critically reviewed and revised the manuscript. DD conceptualized and designed the study, and critically reviewed and revised the manuscript. JBW conceptualized and designed the study, collected data, carried out the initial analyses, and critically reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was approved by the Institutional Review Board at Oregon Health & Science University (#19657). The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fisher, C.R., Dukhovny, D. & Warren, J.B. Effects of a remote patient monitoring program on cost of care for neonates with inadequate oral feeding. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02334-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-025-02334-w