Abstract
Objective
We hypothesized that outborn neonates in three rural states would have more frequent adverse short-term outcomes following therapeutic hypothermia (TH).
Study Design
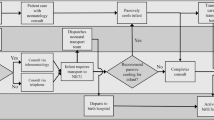
Multicenter retrospective study comparing outcomes for low (<500 births/year), medium (501–1500 births/year), and high (>1500 births/year) birth volume hospitals in Northern New England. Multivariable logistic regression assessed the combined outcome of death/severe gray matter injury on MRI, controlling for encephalopathy severity and time to initiation of TH.
Results
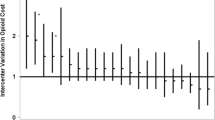
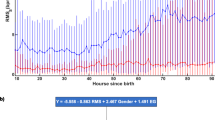
Death occurred for 35/531 neonates: 15/120 (12%) low, 7/193 (4%) medium, and 13/218 (6%) for high birth volume hospitals (p = 0.008). Severe gray matter injury occurred in 8%, 6% and 7% of low, medium, and high birth volume hospitals, respectively (p = 0.7). Odds of the combined outcome were 4.3-fold higher in low versus high volume hospitals (95% CI = 1.6, 12.1, p = 0.004).
Conclusion
Neonates born in low volume birth hospitals had significantly higher odds of death following treatment with TH.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed for the current study are available from the corresponding author on reasonable request.
References
Fairchild K, Sokora D, Scott J, Zanelli S. Therapeutic hypothermia on neonatal transport: 4-year experience in a single NICU. J Perinatol. 2010;30:324–9.
O’Reilly D, Labrecque M, O’Melia M, Bacic J, Hansen A, Soul JS. Passive cooling during transport of asphyxiated term newborns. J Perinatol. 2013;33:435–40.
Harbert MJA, Sey R, Arnell K, Rasmussen M. Identifying ways to fix outcome disparities among outborns needing therapeutic hypothermia. Am J Perinatol. 2021;38:e21–e5.
Simbruner G, Mittal RA, Rohlmann F, Muche R. neo.n EnTP. Systemic hypothermia after neonatal encephalopathy: outcomes of neo.nEURO.network RCT. Pediatrics. 2010;126:e771–8.
Eicher DJ, Wagner CL, Katikaneni LP, Hulsey TC, Bass WT, Kaufman DA, et al. Moderate hypothermia in neonatal encephalopathy: efficacy outcomes. Pediatr Neurol. 2005;32:11–7.
Natarajan G, Pappas A, Shankaran S, Laptook AR, Walsh M, McDonald SA, et al. Effect of inborn vs. outborn delivery on neurodevelopmental outcomes in infants with hypoxic-ischemic encephalopathy: secondary analyses of the NICHD whole-body cooling trial. Pediatr Res. 2012;72:414–9.
Thayyil S, Montaldo P, Krishnan V, Ivain P, Pant S, Lally PJ, et al. Whole-body hypothermia, cerebral magnetic resonance biomarkers, and outcomes in neonates with moderate or severe hypoxic-ischemic encephalopathy born at tertiary care centers vs other facilities: a nested study within a randomized clinical trial. JAMA Netw Open. 2023;6:e2312152.
Shipley L, Mistry A, Sharkey D. Outcomes of neonatal hypoxic-ischaemic encephalopathy in centres with and without active therapeutic hypothermia: a nationwide propensity score-matched analysis. Arch Dis Child Fetal Neonatal Ed. 2022;107:6–12.
Stetson RC, Brumbaugh JE, Weaver AL, Mara KC, Clark RH, Carey WA, et al. Association of outborn versus inborn birth status on the in-hospital outcomes of neonates treated with therapeutic hypothermia: a propensity score-weighted cohort study. Resuscitation. 2021;167:82–8.
Sabsabi B, Huet C, Rampakakis E, Beltempo M, Brown R, Lodygensky GA, et al. Asphyxiated neonates treated with hypothermia: birth place matters. Am J Perinatol. 2022;39:298–306.
Natarajan G, Mathur A, Zaniletti I, DiGeronimo R, Lee KS, Rao R, et al. Withdrawal of life-support in neonatal hypoxic-ischemic encephalopathy. Pediatr Neurol. 2019;91:20–6.
Wilkinson D. MRI and withdrawal of life support from newborn infants with hypoxic-ischemic encephalopathy. Pediatrics. 2010;126:e451–8.
Weeke LC, Groenendaal F, Mudigonda K, Blennow M, Lequin MH, Meiners LC, et al. A novel magnetic resonance imaging score predicts neurodevelopmental outcome after perinatal asphyxia and therapeutic hypothermia. J Pediatr. 2018;192:33–40.e2.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
NB Bayley Scales of Infant and Toddler Development. 3rd ed. San Antonio (TX): Harcourt Assessment; 2006.
Lisonkova S, Haslam MD, Dahlgren L, Chen I, Synnes AR, Lim KI. Maternal morbidity and perinatal outcomes among women in rural versus urban areas. CMAJ: Can Med Assoc J = J de l’Assoc Med Canadienne 2016;188:E456–E65.
Ely DM, Hoyert DL. Differences between rural and urban areas in mortality rates for the leading causes of infant death: United States, 2013-2015. NCHS Data Brief. 2018:1-8.
Ehrenthal DB, Kuo HD, Kirby RS. Infant mortality in rural and nonrural counties in the United States. Pediatrics. 2020;146:e20200464.
Weaver MR, Nandakumar V, Joffe J, Barber RM, Fullman N, Singh A, et al. VaRiation In Health Care Access And Quality Among US states and high-income countries with universal health insurance coverage. JAMA Netw Open. 2021;4:e2114730.
Mooney SE, Ogrinc G, Steadman W. Improving emergency caesarean delivery response times at a rural community hospital. Qual Saf Health Care 2007;16:60–6.
Jukkala AM, Henly SJ. Provider readiness for neonatal resuscitation in rural hospitals. J Obstet Gynecol Neonatal Nurs. 2009;38:443–52.
Zanno A, Melendi M, Cutler A, Stone B, Chipman M, Holmes J, et al. Simulation-based outreach program improves rural hospitals’ team confidence in neonatal resuscitation. Cureus. 2022;14:e28670.
Gunn AJ, Bennet L, Gunning MI, Gluckman PD, Gunn TR. Cerebral hypothermia is not neuroprotective when started after postischemic seizures in fetal sheep. Pediatr Res. 1999;46:274–80.
Gunn AJ, Gunn TR, de Haan HH, Williams CE, Gluckman PD. Dramatic neuronal rescue with prolonged selective head cooling after ischemia in fetal lambs. J Clin Invest. 1997;99:248–56.
Iwata O, Iwata S, Tamura M, Nakamura T, Sugiura M, Ogiso Y, et al. Early head cooling in newborn piglets is neuroprotective even in the absence of profound systemic hypothermia. Pediatrics Int: J Jpn Pediatr Soc 2003;45:522–9.
Thoresen M, Tooley J, Liu X, Jary S, Fleming P, Luyt K, et al. Time is brain: starting therapeutic hypothermia within three hours after birth improves motor outcome in asphyxiated newborns. Neonatology. 2013;104:228–33.
Laptook AR, Shankaran S, Tyson JE, Munoz B, Bell EF, Goldberg RN, et al. Effect of therapeutic hypothermia initiated after 6 h of age on death or disability among newborns with hypoxic-ischemic encephalopathy: a randomized clinical trial. JAMA. 2017;318:1550–60.
Guillot M, Philippe M, Miller E, Davila J, Barrowman NJ, Harrison MA, et al. Influence of timing of initiation of therapeutic hypothermia on brain MRI and neurodevelopment at 18 months in infants with HIE: a retrospective cohort study. BMJ Paediatr Open. 2019;3:e000442.
Wu YW, Comstock BA, Gonzalez FF, Mayock DE, Goodman AM, Maitre NL, et al. Trial of erythropoietin for hypoxic-ischemic encephalopathy in newborns. N Engl J Med. 2022;387:148–59.
Rao R, Comstock BA, Wu TW, Mietzsch U, Mayock DE, Gonzalez FF, et al. Time to reaching target cooling temperature and 2-year outcomes in infants with hypoxic-ischemic encephalopathy. J Pediatr. 2024;266:113853.
de Vries LS, Groenendaal F. Patterns of neonatal hypoxic-ischaemic brain injury. Neuroradiology. 2010;52:555–66.
Lemmon ME, Bonifacio SL, Shellhaas RA, Wusthoff CJ, Greenberg RG, Soul JS, et al. Characterization of death in infants with neonatal seizures. Pediatr Neurol. 2020;113:21–5.
Snowden JM, Tilden EL, Snyder J, Quigley B, Caughey AB, Cheng YW. Planned out-of-hospital birth and birth outcomes. N Engl J Med. 2015;373:2642–53.
Acknowledgements
We thank the individuals who contributed to data collection; Megan Berube, MD, Leah Fox, MD, Lauren McAllister, MD, and Sophi Aronson from MMC as well as Emily Fraser-Read. Delaney Davis, and Krysta Anderson from NLEMMC, Jessica Moya from Elliot Hospital, and Melanie Parziale, MD from The University of Vermont, Larner College of Medicine.
Funding
AKC, AC, and LMS were supported by grant 1P20GM139745-01 from the National Institutes of Health for the Center of Biomedical Research Excellence in Acute Care Research and Rural Disparities. AKC and the REDCap administrator were also supported by U54 GM115516 from the Northern New England Clinical and Translational Research network which funds the MaineHealth instance of REDCap.
Author information
Authors and Affiliations
Contributions
AKC contributions include study conceptualization and design, interpretation of findings, initial draft of the manuscript, and supervision and oversight of the research team. AC contributed to the study design, developed the analysis plan, and completed all analyses. JK, MR, MM, and AZ contributed to study design, data acquisition, and revising the manuscript. LMS contributed to data acquisition and revising the manuscript. DO’R contributed to study conceptualization and design, data acquisition, interpretation of findings, and revision of the manuscript. All authors approve the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Craig, A.K., Cutler, A., Kerecman, J. et al. Association of low hospital birth volume and adverse short-term outcomes for neonates treated with therapeutic hypothermia in rural states. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02352-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41372-025-02352-8