Abstract
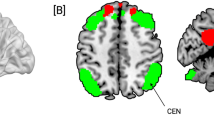
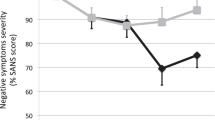
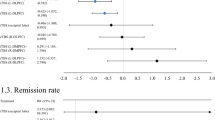
Abnormalities in the prefrontal cortex (PFC)-related network play an important role in the pathophysiology of major depressive disorder (MDD). Accumulating evidence indicated that fronto-striatal dysconnectivity is critical to MDD pathogenesis. Whether non-invasive brain stimulation, including 10-Hz repetitive transcranial magnetic stimulation (rTMS) and intermittent theta-burst stimulation (iTBS), may change cortico-striatal functional connectivity (FC) in MDD patients is unclear. Whether the change of cortico-striatal FC is associated with the antidepressant effects is also unknown. In total, 68 adult MDD subjects were randomly assigned to one of three groups: iTBS, 10-Hz rTMS, or sham group. Functional connectivity was analyzed using MRI and seed-based methods. Seeds included left and right dorsal caudate (DC), dorsal rostral putamen (DRP), and ventral rostral putamen (VRP). The results revealed that significant group-by-time interactions in FC were found in all the striatal seeds. Post-hoc analyses revealed significant increases in FC of the left DRP and VRP for both iTBS and rTMS treatments, particularly with the right frontal pole. Greater FC changes of the fronto-striatal networks correlated with the antidepressant effects. The effects of rTMS and iTBS on FCs of the intra-striatal network, default mode network, and other cortico-striatal networks were distinct. In conclusion, the first study demonstrated that iTBS and rTMS had common but unique effects on the cortico-striatal and intra-striatal networks. These results suggest that both treatments regulate brain reward systems and might be used to treat various striatum-related neuropsychiatric illnesses.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the first author, CTL, upon reasonable request.
References
Krishnan KR. Comorbidity and depression treatment. Biol Psychiatry. 2003;53:701–6.
Lépine J-P, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7:3–7.
DiBernardo A, Lin X, Zhang Q, Xiang J, Lu L, Jamieson C, et al. Humanistic outcomes in treatment resistant depression: a secondary analysis of the STAR*D study. BMC Psychiatry. 2018;18:352.
Kennard B, Silva S, Vitiello B, Curry J, Kratochvil C, Simons A, et al. Remission and residual symptoms after short-term treatment in the Treatment of Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. 2006;45:1404–11.
Rush AJ, Warden D, Wisniewski SR, Fava M, Trivedi MH, Gaynes BN, et al. STAR*D: revising conventional wisdom. CNS Drugs. 2009;23:627–47.
Dignam P. Treatment-resistant depression. Aust N Z J Psychiatry. 2009;43:87.
Little A. Treatment-resistant depression. Am Fam Physician. 2009;80:167–72.
Li CT, Bai YM, Tu PC, Lee YC, Huang YL, Chen TJ, et al. Major depressive disorder and stroke risks: a 9-year follow-up population-based, matched cohort study. PLoS ONE. 2012;7:e46818.
Price JL, Drevets WC. Neurocircuitry of mood disorders. Neuropsychopharmacology. 2010;35:192–216.
Li CT, Su TP, Wang SJ, Tu PC, Hsieh JC. Prefrontal glucose metabolism in medication-resistant major depression. Br J Psychiatry. 2015;206:316–23.
Zhao X, Wu S, Li X, Liu Z, Lu W, Lin K, et al. Common neural deficits across reward functions in major depression: a meta-analysis of fMRI studies. Psychol Med. 2024;23:1–13.
Paus T, Barrett J. Transcranial magnetic stimulation (TMS) of the human frontal cortex: implications for repetitive TMS treatment of depression. J Psychiatry Neurosci. 2004;29:268–79.
Food and Drug Administration US. Transcranial magnetic stimulation for treatment of major depressive disorder. Psychiatric News. 2008;43:1–25.
Berlim MT, van den Eynde F, Tovar-Perdomo S, Daskalakis ZJ. Response, remission and drop-out rates following high-frequency repetitive transcranial magnetic stimulation (rTMS) for treating major depression: a systematic review and meta-analysis of randomized, double-blind and sham-controlled trials. Psychol Med. 2014;44:225–39.
Liu B, Zhang Y, Zhang L, Li L. Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry. 2014;14:342.
Li CT, Chen MH, Juan CH, Huang HH, Chen LF, Hsieh JC, et al. Efficacy of prefrontal theta-burst stimulation in refractory depression: a randomized sham-controlled study. Brain. 2014;137:2088–98.
Li CT, Cheng CM, Chen MH, Juan CH, Tu PC, Bai YM, et al. Antidepressant efficacy of prolonged intermittent theta burst stimulation monotherapy for recurrent depression and comparison of methods for coil positioning: a randomized, double-blind, sham-controlled study. Biol Psychiatry. 2020;87:443–50.
Pogarell O, Koch W, Popperl G, Tatsch K, Jakob F, Mulert C, et al. Acute prefrontal rTMS increases striatal dopamine to a similar degree as D-amphetamine. Psychiatry Res. 2007;156:251–5.
Furman DJ, Hamilton JP, Gotlib IH. Frontostriatal functional connectivity in major depressive disorder. Biol Mood Anxiety Disord. 2011;1:11.
Kerestes R, Harrison BJ, Dandash O, Stephanou K, Whittle S, Pujol J, et al. Specific functional connectivity alterations of the dorsal striatum in young people with depression. Neuroimage Clin. 2015;7:266–72.
Avissar M, Powell F, Ilieva I, Respino M, Gunning FM, Liston C, et al. Functional connectivity of the left DLPFC to striatum predicts treatment response of depression to TMS. Brain Stimul. 2017;10:919–25.
Li CT, Cheng CM, Lin HC, Yeh SH, Jeng JS, Wu HT, et al. The longer, the better ? longer left-sided prolonged intermittent theta burst stimulation in patients with major depressive disorder: a randomized sham-controlled study. Asian J Psychiatr. 2023;87:103686.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6:278–96.
Hung CI, Weng LJ, Su YJ, Liu CY. Depression and somatic symptoms scale: a new scale with both depression and somatic symptoms emphasized. Psychiatry Clin Neurosci. 2006;60:700–8.
Dupont WD, Plummer WD Jr. Power and sample size calculations. A review and computer program. Control Clin Trials. 1990;11:116–28.
Huang YZ, Edwards MJ, Rounis E, Bhatia KP, Rothwell JC. Theta burst stimulation of the human motor cortex. Neuron. 2005;45:201–6.
O’Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62:1208–16.
George MS, Lisanby SH, Avery D, McDonald WM, Durkalski V, Pavlicova M, et al. Daily left prefrontal transcranial magnetic stimulation therapy for major depressive disorder: a sham-controlled randomized trial. Arch Gen Psychiatry. 2010;67:507–16.
Friston KJ, Williams S, Howard R, Frackowiak RS, Turner R. Movement-related effects in fMRI time-series. Magn Reson Med. 1996;35:346–55.
Di Martino A, Scheres A, Margulies DS, Kelly AM, Uddin LQ, Shehzad Z, et al. Functional connectivity of human striatum: a resting state FMRI study. Cereb Cortex. 2008;18:2735–47.
Vincent JL, Snyder AZ, Fox MD, Shannon BJ, Andrews JR, Raichle ME, et al. Coherent spontaneous activity identifies a hippocampal-parietal memory network. J Neurophysiol. 2006;96:3517–31.
Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput Biomed Res. 1996;29:162–73.
Gratton C, Sun H, Petersen SE Control networks and hubs. Psychophysiology. 2018;55. https://doi.org/10.1111/psyp.13032.
Zhong J, Xu J, Wang Z, Yang H, Li J, Yu H, et al. Changes in brain functional networks in remitted major depressive disorder: a six-month follow-up study. BMC Psychiatry. 2023;23:628.
Scheepens DS, van Waarde JA, Lok A, de Vries G, Denys D, van Wingen GA. The link between structural and functional brain abnormalities in depression: a systematic review of multimodal neuroimaging studies. Front Psychiatry. 2020;11:485.
Li CT, Wang SJ, Hirvonen J, Hsieh JC, Bai YM, Hong CJ, et al. Antidepressant mechanism of add-on repetitive transcranial magnetic stimulation in medication-resistant depression using cerebral glucose metabolism. J Affect Disord. 2010;127:219–29.
Roberts BM, Lopes EF, Cragg SJ. Axonal modulation of striatal dopamine release by local gamma-aminobutyric acid (GABA) signalling. Cells. 2021;10:709.
Rubi L, Fritschy JM. Increased GABAergic transmission in neuropeptide Y-expressing neurons in the dopamine-depleted murine striatum. J Neurophysiol. 2020;123:1496–503.
Li CT, Juan CH, Lin HC, Cheng CM, Wu HT, Yang BH, et al. Cortical excitatory and inhibitory correlates of the fronto-limbic circuit in major depression and differential effects of left frontal brain stimulation in a randomized sham-controlled trial. J Affect Disord. 2022;311:364–70.
Li CT, Huang YZ, Bai YM, Tsai SJ, Su TP, Cheng CM. Critical role of glutamatergic and GABAergic neurotransmission in the central mechanisms of theta-burst stimulation. Hum Brain Mapp. 2019;40:2001–9.
Kuroda Y, Motohashi N, Ito H, Ito S, Takano A, Nishikawa T, et al. Effects of repetitive transcranial magnetic stimulation on [11C]raclopride binding and cognitive function in patients with depression. J Affect Disord. 2006;95:35–42.
Shaikh UJ, Pellicano A, Schuppen A, Heinzel A, Winz OH, Herzog H, et al. Increasing striatal dopamine release through repeated bouts of theta burst transcranial magnetic stimulation of the left dorsolateral prefrontal cortex. A 18F-desmethoxyfallypride positron emission tomography study. Front Neurosci. 2023;17:1295151.
Strafella AP, Ko JH, Grant J, Fraraccio M, Monchi O. Corticostriatal functional interactions in Parkinson’s disease: a rTMS/[11C]raclopride PET study. Eur J Neurosci. 2005;22:2946–52.
Runia, Yucel DE N, Lok A, de Jong K, Denys D, van Wingen GA, et al. The neurobiology of treatment-resistant depression: a systematic review of neuroimaging studies. Neurosci Biobehav Rev. 2022;132:433–48.
Raichle ME. The brain’s default mode network. Annu Rev Neurosci. 2015;38:433–47.
Yan CG, Chen X, Li L, Castellanos FX, Bai TJ, Bo QJ, et al. Reduced default mode network functional connectivity in patients with recurrent major depressive disorder. Proc Natl Acad Sci USA. 2019;116:9078–83.
Sheline YI, Barch DM, Price JL, Rundle MM, Vaishnavi SN, Snyder AZ, et al. The default mode network and self-referential processes in depression. Proc Natl Acad Sci USA. 2009;106:1942–7.
Zhou HX, Chen X, Shen YQ, Li L, Chen NX, Zhu ZC, et al. Rumination and the default mode network: meta-analysis of brain imaging studies and implications for depression. Neuroimage. 2020;206:116287.
Sun J, Du Z, Ma Y, Guo C, Gao S, Luo Y, et al. Characterization of resting-state striatal differences in first-episode depression and recurrent depression. Brain Sci. 2022;12:1603.
Liston C, Chen AC, Zebley BD, Drysdale AT, Gordon R, Leuchter B, et al. Default mode network mechanisms of transcranial magnetic stimulation in depression. Biol Psychiatry. 2014;76:517–26.
Schiena G, Franco G, Boscutti A, Delvecchio G, Maggioni E, Brambilla P. Connectivity changes in major depressive disorder after rTMS: a review of functional and structural connectivity data. Epidemiol Psychiatr Sci. 2021;30. https://doi.org/10.1017/S2045796021000482.
Wu F, Lu Q, Kong Y, Zhang Z. A comprehensive overview of the role of visual cortex malfunction in depressive disorders: opportunities and challenges. Neurosci Bull. 2023;39:1426–38.
Lu F, Cui Q, Zou Y, Guo Y, Luo W, Yu Y, et al. Effects of rTMS intervention on functional neuroimaging activities in adolescents with major depressive disorder measured using resting-state fMRI. Bioengineering. 2023;10:1374.
Kirkovski M, Donaldson PH, Do M, Speranza BE, Albein-Urios N, Oberman LM, et al. A systematic review of the neurobiological effects of theta-burst stimulation (TBS) as measured using functional magnetic resonance imaging (fMRI). Brain Struct Funct. 2023;228:717–49.
Chung SW, Rogasch NC, Hoy KE, Sullivan CM, Cash RFH, Fitzgerald PB. Impact of different intensities of intermittent theta burst stimulation on the cortical properties during TMS-EEG and working memory performance. Hum Brain Mapp. 2018;39:783–802.
Zhang BBB, Kan RLD, Giron CG, Lin TTZ, Yau SY, Kranz GS. Dose-response relationship between iTBS and prefrontal activation during executive functioning: A fNIRS study. Front Psychiatry. 2022;13:1049130.
Liu PS, Song DH, Deng XP, Shang YQ, Ge Q, Wang Z, et al. The effects of intermittent theta burst stimulation (iTBS) on resting-state brain entropy (BEN). Neurotherapeutics. 2025;22:e00556.
Burke MJ, Romanella SM, Mencarelli L, Greben R, Fox MD, Kaptchuk TJ, et al. Placebo effects and neuromodulation for depression: a meta-analysis and evaluation of shared mechanisms. Mol Psychiatry. 2022;27:1658–66.
Liu Y, Paradis AL, Yahia-Cherif L, Tallon-Baudry C. Activity in the lateral occipital cortex between 200 and 300 ms distinguishes between physically identical seen and unseen stimuli. Front Hum Neurosci. 2012;6:211.
Cash RFH, Weigand A, Zalesky A, Siddiqi SH, Downar J, Fitzgerald PB, et al. Using brain imaging to improve spatial targeting of transcranial magnetic stimulation for depression. Biol Psychiatry. 2021;90:689–700.
Blumberger DM, Vila-Rodriguez F, Thorpe KE, Feffer K, Noda Y, Giacobbe P, et al. Effectiveness of theta burst versus high-frequency repetitive transcranial magnetic stimulation in patients with depression (THREE-D): a randomised non-inferiority trial. Lancet. 2018;391:1683–92.
Acknowledgements
We would like to thank all the patients who kindly participated in this study and all the research assistants, physicians, and staff who assisted with the study and imaging procedures. This study was sponsored by grants from Taipei Veterans General Hospital (V108D44-003-MY3-1; V111-B-019) [CTL], University System of Taiwan Joint Research Program (VGHUST111-G1-2-1), and the National Science and Technology (MOST108-2321-B-075-004-MY2; NSC 111-2314-B-075-085-MY3) [CTL]. This work was also supported by the Brain Research Center, National Yang Ming Chiao Tung University from The Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan. Neither of the aforementioned organizations had any role in the study design, data collection, analysis, interpretation of results, writing of the report, or ultimate decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
Drs CTL and PCT designed the study; Drs CTL, CMC, TPS, and YMB enrolled the candidate patients and helped with the clinical trial; Miss WCC and Dr PCT analyzed the neuroimaging data; Dr CTL performed the literature reviews; Drs CTL and PCT drafted the manuscript; all authors reviewed the final manuscript and agreed for the publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki and was approved by the Taipei Veterans General Hospital Institutional Review Board. The study was preregistered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR). Registration number: UMIN000044951. Informed consent was provided by all the participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, CT., Chang, WC., Cheng, CM. et al. Comparative effects of 10-Hz rTMS and iTBS on cortico-striatal connectivity in major depressive disorder: a sham-controlled study. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03091-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-025-03091-0