Abstract
Backgroud
This study aimed to explore the associations of lysophosphatidylcholines (LPCs) with insulin resistance (IR) and abdominal obesity among children and adolescents.
Methods
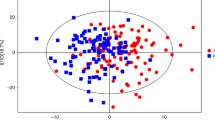
A cross-sectional study was conducted on 612 young individuals, aged 7 to 18 years in Tianjin City, China. LC-MS metabolomic analysis was used to measure LPCs levels. The Homeostasis Model Assessment was used to estimate IR. Waist circumference measurements were used to assess abdominal obesity. Logistic regression models were employed to explore the relationships between LPCs and IR and abdominal obesity. Mediation analyses were performed to analyze whether LPCs affected IR through abdominal obesity.
Results
Compared to their counterparts, five specific LPCs were significantly different in youth with IR. The levels of LPC 24:0 and 26:0 were significantly associated with IR after adjustment. Both decreased levels of LPC 24:0 and 26:0 associated with the increased risks of IR (OR: 0.64, 95%CI: 0.38–0.95; OR: 0.66, 95%CI: 0.40–1.00), and the ORs for abdominal obesity were 0.68 (95%CI: 0.38–1.00) and 0.51 (95%CI: 0.28–0.90), respectively. Mediation analysis indicated that abdominal obesity mediated the association between LPC 26:0 and IR, with a total effect (c) of −0.109 (P < 0.05), a direct effect (c’) of −0.055 (P > 0.05), and an indirect effect through obesity (a × b) path with “a” of −0.125 (P < 0.05) and “b” of 0.426 (P < 0.05).
Conclusion
Overall findings suggest that decreased levels of LPC 24:0 and 26:0 were associated with increased risks of IR and abdominal obesity. Importantly, addressing abdominal obesity may mediate the impact of IR driven by LPC 26:0.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
269,00 € per year
only 19,21 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in underweight and obesity from 1990 to 2022: a pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet 403, 1027–1050 (2024).
Popkin, B. M., Adair, L. S. & Ng, S. W. Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 70, 3–21 (2012).
Jackson-Leach, R. & Lobstein, T. Estimated burden of pediatric obesity and co-morbidities in Europe. Part 1. The increase in the prevalence of child obesity in Europe is itself increasing. Int. J. Pediatr. Obes. 1, 26–32 (2006).
Janssen, I. et al. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes. Rev. 6, 123–132, (2005).
Newman, T. B. et al. Childhood Seizures after phototherapy. Pediatrics 142, e20180648 (2018).
Lee, S., Bacha, F. & Arslanian, S. A. Waist circumference, blood pressure, and lipid components of the metabolic syndrome. J. Pediatr. 149, 809–816 (2006).
Zhang, C. et al. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation 117, 1658–1667 (2008).
Weihrauch-Blüher, S., Schwarz, P. & Klusmann, J. H. Childhood obesity: increased risk for cardiometabolic disease and cancer in adulthood. Metabolism 92, 147–152 (2019).
Birgbauer, E. & Chun, J. New developments in the biological functions of lysophospholipids. Cell Mol. Life Sci. 63, 2695–2701 (2006).
Fukushima, N. et al. Lysophospholipid receptors. Annu Rev. Pharm. Toxicol. 41, 507–534 (2001).
Xu, Y. Sphingosylphosphorylcholine and lysophosphatidylcholine: G protein-coupled receptors and receptor-mediated signal transduction. Biochim. Biophys. Acta 1582, 81–88 (2002).
Suvitaival, T. et al. Lipidome as a predictive tool in progression to type 2 diabetes in Finnish men. Metabolism 78, 1–12 (2018).
Wang-Sattler, R. et al. Novel biomarkers for pre-diabetes identified by metabolomics. Mol. Syst. Biol. 8, 615 (2012).
Lee, Y. K. et al. Lysophosphatidylcholine, oxidized low-density lipoprotein and cardiovascular disease in Korean hemodialysis patients: analysis at 5 years of follow-up. J. Korean Med. Sci. 28, 268–273 (2013).
Fernandez, C. et al. Plasma lipid composition and risk of developing cardiovascular disease. PLoS ONE 8, e71846 (2013).
Carrascosa, J. M. et al. Obesity and psoriasis: inflammatory nature of obesity, relationship between psoriasis and obesity, and therapeutic implications. Actas Dermosifiliogr. 105, 31–44 (2014).
Esser, N. et al. Inflammation as a link between obesity, metabolic syndrome and type 2 diabetes. Diabetes Res. Clin. Pract. 105, 141–150 (2014).
Howard, B. V. Insulin resistance and lipid metabolism. Am. J. Cardiol. 84, 28J–32J (1999).
Tonks, K. T. et al. Skeletal muscle and plasma lipidomic signatures of insulin resistance and overweight/obesity in humans. Obesity 24, 908–916 (2016).
Rai, S. & Bhatnagar, S. Novel Lipidomic Biomarkers in Hyperlipidemia and cardiovascular diseases: an integrative biology analysis. OMICS 21, 132–142 (2017).
Bao, L. et al. Lysophosphatidylcholine (17:0) Improves HFD-Induced hyperglycemia & insulin resistance: a mechanistic mice model study. Diabetes Metab. Syndr. Obes. 15, 3511–3517 (2022).
Liu, P. et al. The mechanisms of lysophosphatidylcholine in the development of diseases. Life Sci. 247, 117443 (2020).
Bellot, P. E. N. R. et al. Are Phosphatidylcholine and Lysophosphatidylcholine Body Levels Potentially Reliable Biomarkers in Obesity? A Review of Human Studies. Mol. Nutr. Food Res. 67, e2200568 (2023).
Puri, P. et al. The plasma lipidomic signature of nonalcoholic steatohepatitis. Hepatology 50, 1827–1838 (2009).
Ma, G. S. et al. Waist circumference reference values for screening cardiovascular risk factors in Chinese children and adolescents. Biomed. Environ. Sci. 23, 21–31 (2010).
Yan, X. X. & Ying, Y. W. The diagnostic significance of homeostasis model assessment of insulin resistance in metabolic syndrome among subjects with different glucose tolerance. Chin. J. Diabetes 3, 31–35 (2004).
Szukiewicz, D. Molecular mechanisms for the vicious cycle between insulin resistance and the inflammatory response in obesity. Int. J. Mol. Sci. 24, 9818 (2023).
Barazzoni, R. et al. Insulin resistance in obesity: an overview of fundamental alterations. Eat. Weight Disord. 23, 149–157 (2018).
Schmitz, G. & Ruebsaamen, K. Metabolism and atherogenic disease association of lysophosphatidylcholine. Atherosclerosis 208, 10–18 (2010).
Barber, M. N. et al. Plasma lysophosphatidylcholine levels are reduced in obesity and type 2 diabetes. PLoS ONE 7, e41456 (2012).
Yea, K. et al. Lysophosphatidylcholine activates adipocyte glucose uptake and lowers blood glucose levels in murine models of diabetes. J. Biol. Chem. 284, 33833–33840 (2009).
Drzazga, A. et al. Lysophosphatidylcholine containing anisic acid is able to stimulate insulin secretion targeting G protein coupled receptors. Nutrients 12, 1173 (2020).
Graessler, J. et al. Top-down lipidomics reveals ether lipid deficiency in blood plasma of hypertensive patients. PLoS ONE 4, e6261 (2009).
Floegel, A. et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes 62, 639–648 (2013).
Razquin, C. et al. Plasma lipidomic profiling and risk of type 2 Diabetes in the PREDIMED Trial. Diab. Care 41, 2617–2624 (2018).
Prada, M. et al. Association of the odd-chain fatty acid content in lipid groups with type 2 diabetes risk: A targeted analysis of lipidomics data in the EPIC-Potsdam cohort. Clin. Nutr. 40, 4988–4999 (2021).
Wang, Y. et al. Lipidomic profile revealed the association of plasma lysophosphatidylcholines with adolescent obesity. Biomed. Res. Int. 2019, 1382418 (2019).
Kim, J. Y. et al. Metabolic profiling of plasma in overweight/obese and lean men using ultra performance liquid chromatography and Q-TOF mass spectrometry (UPLC-Q-TOF MS). J. Proteome Res. 9, 4368–4375 (2010).
Sharma, S. et al. Circulatory levels of lysophosphatidylcholine species in obese adolescents: findings from cross-sectional and prospective lipidomics analyses. Nutr. Metab. Cardiovasc. Dis. 34, 1807–1816 (2024).
Heimerl, S. et al. Alterations of plasma lysophosphatidylcholine species in obesity and weight loss. PLoS ONE 9, e111348 (2014).
Wei, M. et al. Waist circumference as the best predictor of noninsulin dependent diabetes mellitus (NIDDM) compared to body mass index, waist/hip ratio and other anthropometric measurements in Mexican Americans-a 7-year prospective study. Obes. Res. 5, 16–23 (1997).
Kivimäki, M. et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2, e277–e285 (2017).
Global BMI Mortality Collaboration. et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet 388, 776–786 (2016).
Molani Gol, R. & Rafraf, M. Association between abdominal obesity and pulmonary function in apparently healthy adults: A systematic review. Obes. Res. Clin. Pract. 15, 415–424 (2021).
Zingarelli, B. et al. Peroxisome proliferator-activated receptor {delta} regulates inflammation via NF-{kappa}B signaling in polymicrobial sepsis. Am. J. Pathol. 177, 1834–1847 (2010).
Piqueras, L. et al. Activation of PPARbeta/delta inhibits leukocyte recruitment, cell adhesion molecule expression, and chemokine release. J. Leukoc. Biol. 86, 115–122 (2008).
Takahashi, H. et al. Metabolomics reveal 1-palmitoyl lysophosphatidylcholine production by peroxisome proliferator-activated receptor α. J. Lipid Res. 56, 254–265 (2015).
Cariou, B. et al. Dual peroxisome proliferator-activated receptor α/δ agonist GFT505 improves hepatic and peripheral insulin sensitivity in abdominally obese subjects. Diabetes Care 36, 2923–2930 (2013).
Demerath, E. W. et al. Do changes in body mass index percentile reflect changes in body composition in children? Data from the Fels Longitudinal Study. Pediatrics 117, e487–e495 (2006).
McCarthy, H. D., Ellis, S. M. & Cole, T. J. Central overweight and obesity in British youth aged 11-16 years: cross sectional surveys of waist circumference. BMJ 326, 624 (2003).
Acknowledgements
The authors thank all the physicians, nurses and research staff at the Tianjin Medical University General Hospital who participated in the study and extended their support for data collection. This research was supported by the National Key Research and Development Program of China (2021YFA1301202), General hospital Clinical research project (22ZYYLCCG03), Tianjin Key Medical Discipline (Specialty) Construction Project (TJWJ2022XK008, TJYXZDXK-068C), Tianjin Science and Technology Plan Project (22KPHDRC00120), and National Natural Science Foundation of China (Grant No: 82200932, 82273676, 32400963 & 92357305).
Author information
Authors and Affiliations
Contributions
J.L., S.M., and X.Z. substantially contributed to the conception and design of the work. X.-Y.Z., Z.F., X.L., X.H., and Z.-H.Z. substantially contributed to acquisition of the data. X.-Y.Z., J.L., and H.L. analyzed the data and drafted the article. C.-Y.L., T.A., Y.W., and X.K. revised the article critically for important intellectual content. All authors edited the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The studies involving human participants were reviewed and approved by Tianjin Medical University General Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, X., Liu, H., Li, C. et al. Abdominal obesity in youth: the associations of plasma Lysophophatidylcholine concentrations with insulin resistance. Pediatr Res (2024). https://doi.org/10.1038/s41390-024-03652-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-024-03652-z