Abstract
Study design
Narrative review.
Objectives
To discuss how electrophysiology may contribute to future clinical trials in spinal cord injury (SCI) in terms of: (1) improvement of SCI diagnosis, patient stratification and determination of exclusion criteria; (2) the assessment of adverse events; and (3) detection of therapeutic effects following an intervention.
Methods
An international expert panel for electrophysiological measures in SCI searched and discussed the literature focused on the topic.
Results
Electrophysiology represents a valid method to detect, track, and quantify readouts of nerve functions including signal conduction, e.g., evoked potentials testing long spinal tracts, and neural processing, e.g., reflex testing. Furthermore, electrophysiological measures can predict functional outcomes and thereby guide rehabilitation programs and therapeutic interventions for clinical studies.
Conclusion
Objective and quantitative measures of sensory, motor, and autonomic function based on electrophysiological techniques are promising tools to inform and improve future SCI trials. Complementing clinical outcome measures, electrophysiological recordings can improve the SCI diagnosis and patient stratification, as well as the detection of both beneficial and adverse events. Specifically composed electrophysiological measures can be used to characterize the topography and completeness of SCI and reveal neuronal integrity below the lesion, a prerequisite for the success of any interventional trial. Further validation of electrophysiological tools with regard to their validity, reliability, and sensitivity are needed in order to become routinely applied in clinical SCI trials.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF, et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord. 2007;45:206–21.
Lammertse D, Tuszynski MH, Steeves JD, Curt A, Fawcett JW, Rask C, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial design. Spinal Cord. 2007;45:232–42.
Tuszynski MH, Steeves JD, Fawcett JW, Lammertse D, Kalichman M, Rask C, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord. 2007;45:222–31.
Furlan JC, Fehlings MG, Tator CH, Davis AM. Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA standards. J Neurotrauma. 2008;25:1273–301.
Alexander MS, Anderson KD, Biering-Sorensen F, Blight AR, Brannon R, Bryce TN, et al. Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord. 2009;47:582–91.
Krassioukov A, Biering-Sorensen F, Donovan W, Kennelly M, Kirshblum S, Krogh K, et al. International standards to document remaining autonomic function after spinal cord injury. J Spinal Cord Med. 2012;35:201–10.
Tanadini LG, Steeves JD, Hothorn T, Abel R, Maier D, Schubert M, et al. Identifying homogeneous subgroups in neurological disorders: unbiased recursive partitioning in cervical complete spinal cord injury. Neurorehabilit Neural Repair. 2014;28:507–15.
Cadotte DW, Fehlings MG. Will imaging biomarkers transform spinal cord injury trials? Lancet Neurol. 2013;12:843–4.
Hupp M, Pavese C, Bachmann L, Koller R, Schubert M. Electrophysiological multimodal assessments improve outcome prediction in traumatic cervical spinal cord injury. J Neurotrauma. 2018;35:2916–23.
Spiess MR, Muller RM, Rupp R, Schuld C, Group E-SS, van Hedel HJ. Conversion in ASIA impairment scale during the first year after traumatic spinal cord injury. J Neurotrauma. 2009;26:2027–36.
Petersen JA, Spiess M, Curt A, Weidner N, Rupp R, Abel R, et al. Upper limb recovery in spinal cord injury: involvement of central and peripheral motor pathways. Neurorehabilit Neural Repair. 2017;31:432–41.
Spiess M, Schubert M, Kliesch U, group E-SS, Halder P. Evolution of tibial SSEP after traumatic spinal cord injury: baseline for clinical trials. Clin Neurophysiol. 2008;119:1051–61.
Wasner G, Lee BB, Engel S, McLachlan E. Residual spinothalamic tract pathways predict development of central pain after spinal cord injury. Brain. 2008;131:2387–400.
Finnerup NB, Gyldensted C, Fuglsang-Frederiksen A, Bach FW, Jensen TS. Sensory perception in complete spinal cord injury. Acta Neurol Scand. 2004;109:194–9.
Biering-Sorensen F, Alai S, Anderson K, Charlifue S, Chen Y, DeVivo M, et al. Common data elements for spinal cord injury clinical research: a National Institute for Neurological Disorders and Stroke project. Spinal Cord. 2015;53:265–77.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
McKay WB, Lim HK, Priebe MM, Stokic DS, Sherwood AM. Clinical neurophysiological assessment of residual motor control in post-spinal cord injury paralysis. Neurorehabilit Neural Repair. 2004;18:144–53.
Curt A, Dietz V. Neurographic assessment of intramedullary motoneurone lesions in cervical spinal cord injury: consequences for hand function. Spinal Cord. 1996;34:326–32.
Machida M, Yamada T, Ross M, Kimura J, Hitchon P. Effect of spinal cord ischemia on compound muscle action potentials and spinal evoked potentials following spinal cord stimulation in the dog. J Spinal Disord. 1990;3:345–52.
Oeda T, Kanda M, Onishi K, Kaji R, Akiguchi I. The value of F-waves in an early electrodiagnosis of the lower cervical cord infarction. Rinsho Shinkeigaku. 1996;36:587–9.
Van De Meent H, Hosman AJ, Hendriks J, Zwarts M, Schubert M. Severe degeneration of peripheral motor axons after spinal cord injury: a European multicenter study in 345 patients. Neurorehabilit Neural Repair. 2010;24:657–65.
Boland RA, Lin CS, Engel S, Kiernan MC. Adaptation of motor function after spinal cord injury: novel insights into spinal shock. Brain. 2011;134:495–505.
Lin CS, Macefield VG, Elam M, Wallin BG, Engel S, Kiernan MC. Axonal changes in spinal cord injured patients distal to the site of injury. Brain. 2007;130:985–94.
Parry GJ. Electrodiagnostic studies in the evaluation of peripheral nerve and brachial plexus injuries. Neurol Clin. 1992;10:921–34.
Curt A, Dietz V. Electrophysiological recordings in patients with spinal cord injury: significance for predicting outcome. Spinal Cord1999;37:157–65.
Petersen JA, Schubert M, Dietz V. The occurrence of the Babinski sign in complete spinal cord injury. J Neurol. 2010;257:38–43.
Petersen JA, Spiess M, Curt A, Dietz V, Schubert M. Spinal cord injury: one-year evolution of motor-evoked potentials and recovery of leg motor function in 255 patients. Neurorehabilit Neural Repair. 2012;26:939–48.
Little JW, Halar E. Temporal course of motor recovery after Brown-Sequard spinal cord injuries. Paraplegia. 1985;23:39–46.
Haefeli J, Kramer JL, Blum J, Curt A. Assessment of spinothalamic tract function beyond pinprick in spinal cord lesions: a contact heat evoked potential study. Neurorehabilit Neural Repair. 2014;28:494–503.
Yamada T. Neuroanatomic substrates of lower extremity somatosensory evoked potentials. J Clin Neurophysiol. 2000;17:269–79.
Ulrich A, Haefeli J, Blum J, Min K, Curt A. Improved diagnosis of spinal cord disorders with contact heat evoked potentials. Neurology. 2013;80:1393–9.
Ulrich A, Min K, Curt A. High sensitivity of contact-heat evoked potentials in “snake-eye” appearance myelopathy. Clin Neurophysiol. 2015;126:1994–2003.
Fisher KM, Zaaimi B, Baker SN. Reticular formation responses to magnetic brain stimulation of primary motor cortex. J Physiol. 2012;590:4045–60.
Matsugi A, Mori N, Uehara S, Kamata N, Oku K, Okada Y. et al. Effect of cerebellar transcranial magnetic stimulation on soleus Ia presynaptic and reciprocal inhibition. Neuroreport.2015;26:139–43.
Di Lazzaro V, Pilato F, Oliviero A, Saturno E, Dileone M, Tonali PA. Role of motor evoked potentials in diagnosis of cauda equina and lumbosacral cord lesions. Neurology. 2004;63:2266–71.
Schneider RC. The syndrome of acute anterior spinal cord injury. J Neurosurg. 1955;12:95–122.
Bromm B, Frieling A, Lankers J. Laser-evoked brain potentials in patients with dissociated loss of pain and temperature sensibility. Electroencephalogr Clin Neurophysiol. 1991;80:284–91.
Molliqaj G, Payer M, Schaller K, Tessitore E. Acute traumatic central cord syndrome: a comprehensive review. Neurochirurgie. 2014;60:5–11.
Lemon RN, Kirkwood PA, Maier MA, Nakajima K, Nathan P. Direct and indirect pathways for corticospinal control of upper limb motoneurons in the primate. Prog Brain Res. 2004;143:263–79.
Berger MJ, Hubli M, Krassioukov AV. Sympathetic skin responses and autonomic dysfunction in spinal cord injury. J Neurotrauma. 2014;31:1531–9.
Curt A, Weinhardt C, Dietz V. Significance of sympathetic skin response in the assessment of autonomic failure in patients with spinal cord injury. J Auton Nerv Syst 1996;61:175–80.
Kramer JK, Taylor P, Steeves JD, Curt A. Dermatomal somatosensory evoked potentials and electrical perception thresholds during recovery from cervical spinal cord injury. Neurorehabilit Neural Repair 2010;24:309–17.
Jutzeler CR, Rosner J, Rinert J, Kramer JL, Curt A. Normative data for the segmental acquisition of contact heat evoked potentials in cervical dermatomes. Sci Rep. 2016;6:34660.
van Hedel HJ, Kumru H, Rohrich F, Galen S. Changes in electrical perception threshold within the first 6 months after traumatic spinal cord injury: a multicenter responsiveness study. Neurorehabilit Neural Repair. 2012;26:497–506.
Ellaway PH, Kuppuswamy A, Balasubramaniam AV, Maksimovic R, Gall A, Craggs MD, et al. Development of quantitative and sensitive assessments of physiological and functional outcome during recovery from spinal cord injury: a clinical initiative. Brain Res Bull. 2011;84:343–57.
Shields CB, Ping Zhang Y, Shields LB, Burke DA, Glassman SD. Objective assessment of cervical spinal cord injury levels by transcranial magnetic motor-evoked potentials. Surg Neurol. 2006;66:475–83. discussion 483.
Cariga P, Catley M, Nowicky AV, Savic G, Ellaway PH, Davey NJ. Segmental recording of cortical motor evoked potentials from thoracic paravertebral myotomes in complete spinal cord injury. Spine. 2002;27:1438–43.
Ellaway PH, Anand P, Bergstrom EM, Catley M, Davey NJ, Frankel HL, et al. Towards improved clinical and physiological assessments of recovery in spinal cord injury: a clinical initiative. Spinal Cord. 2004;42:325–37.
Dimitrijevic MR. Residual motor functions in spinal cord injury. Adv Neurol. 1988;47:138–55.
Cariga P, Catley M, Mathias CJ, Savic G, Frankel HL, Ellaway PH. Organisation of the sympathetic skin response in spinal cord injury. J Neurol Neurosurg Psychiatry. 2002;72:356–60.
Claydon VE, Krassioukov AV. Orthostatic hypotension and autonomic pathways after spinal cord injury. J Neurotrauma. 2006;23:1713–25.
Kuhn F, Halder P, Spiess MR, Schubert M, Group E-SS. One-year evolution of ulnar somatosensory potentials after trauma in 365 tetraplegic patients: early prediction of potential upper limb function. J Neurotrauma. 2012;29:1829–37.
Wirth B, Van Hedel HJ, Curt A. Changes in corticospinal function and ankle motor control during recovery from incomplete spinal cord injury. J Neurotrauma. 2008;25:467–78.
Wirth B, van Hedel HJ, Curt A. Ankle dexterity is less impaired than muscle strength in incomplete spinal cord lesion. J Neurol. 2008;255:273–9.
Thomas SL, Gorassini MA. Increases in corticospinal tract function by treadmill training after incomplete spinal cord injury. J Neurophysiol. 2005;94:2844–55.
Kramer JL, Lammertse DP, Schubert M, Curt A, Steeves JD. Relationship between motor recovery and independence after sensorimotor-complete cervical spinal cord injury. Neurorehabilit Neural Repair. 2012;26:1064–71.
Slimp JC, Rubner DE, Snowden ML, Stolov WC. Dermatomal somatosensory evoked potentials: cervical, thoracic, and lumbosacral levels. Electroencephalogr Clin Neurophysiol. 1992;84:55–70.
Killeen T, Rosner J, Jutzeler CR, Hupp M, Heilbronner R, Curt A. Spontaneous resolution of an extensive posttraumatic syrinx. Neurology. 2016;87:1299–301.
Wirth B, van Hedel HJ, Curt A. Ankle paresis in incomplete spinal cord injury: relation to corticospinal conductivity and ambulatory capacity. J Clin Neurophysiol. 2008;25:210–7.
Firmin L, Field P, Maier MA, Kraskov A, Kirkwood PA, Nakajima K, et al. Axon diameters and conduction velocities in the macaque pyramidal tract. J Neurophysiol. 2014;112:1229–40.
Kohara N, Kimura J, Kaji R, Goto Y, Ishii J, Takiguchi M, et al. F-wave latency serves as the most reproducible measure in nerve conduction studies of diabetic polyneuropathy: multicentre analysis in healthy subjects and patients with diabetic polyneuropathy. Diabetologia. 2000;43:915–21.
Pinheiro DS, Manzano GM, Nobrega JA. Reproducibility in nerve conduction studies and F-wave analysis. Clin Neurophysiol. 2008;119:2070–3.
Pauri F, Boffa L, Cassetta E, Pasqualetti P, Rossini PM. Botulinum toxin type-A treatment in spastic paraparesis: a neurophysiological study. J Neurol Sci. 2000;181:89–97.
Hiersemenzel LP, Curt A, Dietz V. From spinal shock to spasticity: neuronal adaptations to a spinal cord injury. Neurology. 2000;54:1574–82.
(AAEM) AAoEM. The electrodiagnostic evaluation of patients with suspected cervical radiculopathy: literature review on the usefulness of needle electromyography. Muscle Nerve. 1999;22:S213–21.
Narayanaswami P, Geisbush T, Jones L, Weiss M, Mozaffar T, Gronseth G, et al. Critically re-evaluating a common technique: accuracy, reliability, and confirmation bias of EMG. Neurology. 2016;86:218–23.
Calder KM, Stashuk DW, McLean L. Motor unit potential morphology differences in individuals with non-specific arm pain and lateral epicondylitis. J Neuroeng Rehabil 2008;5:34.
Takehara I, Chu J, Li TC, Schwartz I. Reliability of quantitative motor unit action potential parameters. Muscle Nerve. 2004;30:111–3.
Palmieri RM, Hoffman MA, Ingersoll CD. Intersession reliability for H-reflex measurements arising from the soleus, peroneal, and tibialis anterior musculature. Int J Neurosci. 2002;112:841–50.
Hopkins JT, Ingersoll CD, Cordova ML, Edwards JE. Intrasession and intersession reliability of the soleus H-reflex in supine and standing positions. Electroencephalogr Clin Neurophysiol. 2000;40:89–94.
Hopkins JT, Wagie NC. Intrasession and intersession reliability of the quadriceps Hoffmann reflex. Electroencephalogr Clin Neurophysiol. 2003;43:85–9.
Phadke CP, Thompson FJ, Trimble MH, Behrman AL, Kukulka CG. Reliability of soleus H-reflexes in standing and walking post-incomplete spinal cord injury. Int J Neurosci. 2010;120:128–36.
Curt A, Dietz V. Traumatic cervical spinal cord injury: relation between somatosensory evoked potentials, neurological deficit, and hand function. Arch Phys Med Rehabil. 1996;77:48–53.
Curt A, Dietz V. Ambulatory capacity in spinal cord injury: significance of somatosensory evoked potentials and ASIA protocol in predicting outcome. Arch Phys Med Rehabil. 1997;78:39–43.
Jutzeler CR, Streijger F, Aguilar J, Shortt K, Manouchehri N, Okon E, et al. Sensorimotor plasticity after spinal cord injury: a longitudinal and translational study. Ann Clin Transl Neurol. 2019;6:68–82.
Kramer JL, Moss AJ, Taylor P, Curt A. Assessment of posterior spinal cord function with electrical perception threshold in spinal cord injury. J Neurotrauma. 2008;25:1019–26.
Savic G, Bergstrom EM, Frankel HL, Jamous MA, Ellaway PH, Davey NJ. Perceptual threshold to cutaneous electrical stimulation in patients with spinal cord injury. Spinal Cord. 2006;44:560–6.
Leong GW, Gorrie CA, Ng K, Rutkowski S, Waite PM. Electrical perceptual threshold testing: a validation study. J Spinal Cord Med. 2009;32:140–6.
Lagerburg V, Bakkers M, Bouwhuis A, Hoeijmakers JG, Smit AM, Van Den Berg SJ, et al. Contact heat evoked potentials: normal values and use in small-fiber neuropathy. Muscle Nerve. 2015;51:743–9.
Rosner J, Hubli M, Hostettler P, Scheuren PS, Rinert J, Kramer JLK, et al. Contact heat evoked potentials: Reliable acquisition from lower extremities. Clin Neurophysiol. 2018;129:584–91.
Kramer JL, Haefeli J, Curt A, Steeves JD. Increased baseline temperature improves the acquisition of contact heat evoked potentials after spinal cord injury. Clin Neurophysiol. 2012;123:582–9.
Jutzeler CR, Ulrich A, Huber B, Rosner J, Kramer JLK, Curt A. Improved diagnosis of cervical spondylotic myelopathy with contact heat evoked potentials. J Neurotrauma. 2017;34:2045–53.
Treede RD, Lankers J, Frieling A, Zangemeister WH, Kunze K, Bromm B. Cerebral potentials evoked by painful, laser stimuli in patients with syringomyelia. Brain. 1991;114:1595–607. (Pt 4)
Iannetti GD, Truini A, Galeotti F, Romaniello A, Manfredi M, Cruccu G. Usefulness of dorsal laser evoked potentials in patients with spinal cord damage: report of two cases. J Neurol Neurosurg Psychiatry. 2001;71:792–4.
Potter-Baker KA, Janini DP, Frost FS, Chabra P, Varnerin N, Cunningham DA, et al. Reliability of TMS metrics in patients with chronic incomplete spinal cord injury. Spinal Cord. 2016;54:980–90.
Pellegrini M, Zoghi M, Jaberzadeh S. The effect of transcranial magnetic stimulation test intensity on the amplitude, variability and reliability of motor evoked potentials. Brain Res. 2018;1700:190–8.
van Hedel HJ, Murer C, Dietz V, Curt A. The amplitude of lower leg motor evoked potentials is a reliable measure when controlled for torque and motor task. J Neurol. 2007;254:1089–98.
Hubli M, Krassioukov AV. How reliable are sympathetic skin responses in subjects with spinal cord injury? Clin Auton Res. 2015;25:117–24.
Dietz V, Curt A. Neurological aspects of spinal-cord repair: promises and challenges. Lancet Neurol. 2006;5:688–94.
Funding
Funding was provided by the American Spinal Injury Association (ASIA), Christopher and Dana Reeve Foundation (CDRF), Craig H. Neilsen Foundation (CHN), International Research Foundation for Paraplegia (IRP), Rick Hansen Institute (RHI), Spinal Cord Outcomes Partnership Endeavor (SCOPE), Spinal Research (SR), Wings for Life (WfL).
Author information
Authors and Affiliations
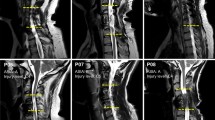
Contributions
MH was responsible for manuscript assembly, conducting the search, compiling the patient cases, creating the Table and writing the manuscript. MS was responsible for conducting research, compiling the patient cases and writing the manuscript. All remaining authors (JLKK, CRJ, JR, JCF, and KET) contributed individually by conducting the search and writing individual sections of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the data collection for patient examples provided in this manuscript. The local ethics board ‘Kantonale Ethikkommission Zürich, KEK’ (EK-04/2006, PB_2016-02051, clinicaltrial.gov number: NCT02138344) has approved this data collection.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hubli, M., Kramer, J.L.K., Jutzeler, C.R. et al. Application of electrophysiological measures in spinal cord injury clinical trials: a narrative review. Spinal Cord 57, 909–923 (2019). https://doi.org/10.1038/s41393-019-0331-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0331-z
This article is cited by
-
Research progress and prospects of benefit-risk assessment methods for umbilical cord mesenchymal stem cell transplantation in the clinical treatment of spinal cord injury
Stem Cell Research & Therapy (2024)
-
Functional electrical stimulation therapy for upper extremity rehabilitation following spinal cord injury: a pilot study
Spinal Cord Series and Cases (2023)
-
Integration of MRI and somatosensory evoked potentials facilitate diagnosis of spinal cord compression
Scientific Reports (2023)
-
Properties of the surface electromyogram following traumatic spinal cord injury: a scoping review
Journal of NeuroEngineering and Rehabilitation (2021)
-
Assessment of neuropathic pain after spinal cord injury using quantitative pain drawings
Spinal Cord (2021)