Abstract
Introduction
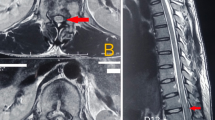
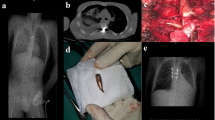
The incidence of preoperative neurological deficits in pediatric patients with complex deformities ranges from 15% to 23%. Furthermore, the likelihood of a postoperative neurological deficit can be considerably increased to 83.3% in the presence of a preoperative neurological deficit. Hence, the management of pediatric spinal deformities with neurological deficits is a challenge for every spine surgeon. Here, we describe four consecutive cases of pediatric spinal deformity with myelopathic cord, all of which were managed with decompressive surgery and stabilization without any attempts to correct the deformity. All the patients recovered well neurologically, without any progression of deformity.
Case presentation
The authors obtained the informed written consent from the patient and their parents for the print and electronic publication of the case. All four patients had clinical myelopathy with a progressive, worsening neurological deficit. The pathology was in the thoracic region in all the patients. Of the four cases, two were post-tubercular deformities, and two were congenital deformities. The treatment strategy for all patients was circumferential decompression of the spinal cord with posterior pedicle screw instrumentation. Although all patients had significant neurological deficits (Nurick grade 4 or 5) preoperatively, we used intraoperative neuromonitoring to prevent the worsening of the deficit during the procedure. None of the patients experienced intraoperative signal changes. All patients had significant neurological recovery (Nurick grade 0 to 2) and showed no worsening of deformity at their latest follow-up, up to 4 years. All showed good improvement in all domains of the SRS22r questionnaire.
Discussion
It is challenging for spine surgeons to manage complex spinal abnormalities in pediatric patients with myelopathic cords. Even a minimal manipulation of the cord during surgery might result in severe long-term morbidity. The primary objective in managing such patients should be neurological recovery rather than deformity correction—“First do no harm,” and if necessary, the deformity can be corrected at a later stage under neuromonitoring.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 print issues and online access
We are sorry, but there is no personal subscription option available for your country.
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Deidentified data are available from the corresponding authors upon reasonable request.
References
Cerpa M, Zuckerman SL, Lenke LG, Kelly MP, Yaszay B, Newton P, et al. Myelopathic patients undergoing severe pediatric spinal deformity surgery can improve neurologic function to that of non-myelopathic patients by 1-Year postoperative. Glob Spine J. 2023;13:1384–93.
Xie JM, Zhang Y, Wang YS, Bi N, Zhao Z, Li T, et al. The risk factors of neurologic deficits of one-stage posterior vertebral column resection for patients with severe and rigid spinal deformities. Eur Spine J. 2014;23:149–56.
Sielatycki JA, Cerpa M, Baum G, Pham M, Thuet E, Lehman RA, et al. A novel MRI-based classification of spinal cord shape and CSF presence at the curve apex to assess risk of intraoperative neuromonitoring data loss with thoracic spinal deformity correction. Spine Deform. 2020;8:655–61.
Patient Outcome Questionnaires | Scoliosis Research Society [Internet]. [cited 2024 Feb 4]. Available from: https://www.srs.org/Research/Patient-Outcome-Questionnaires.
Boachie-Adjei O, Yagi M, Nemani VM, Sacramento-Dominguez C, Akoto H, Cunningham ME, et al. Incidence and risk factors for major surgical complications in patients with complex spinal deformity: a report from an SRS GOP site. Spine Deform. 2015;3:57–64.
Boachie-Adjei O, Duah HO, Yankey KP, Lenke LG, Sponseller PD, Sucato DJ, et al. New neurologic deficit and recovery rates in the treatment of complex pediatric spine deformities exceeding 100 degrees or treated by vertebral column resection (VCR). Spine Deform. 2021;9:427–33.
Bivona LJ, France J, Daly-Seiler CS, Burton DC, Dolan LA, Seale JJ, et al. Spinal deformity surgery is accompanied by serious complications: report from the Morbidity and Mortality Database of the Scoliosis Research Society from 2013 to 2020. Spine Deform. 2022;10:1307–13.
Vitale MG, Skaggs DL, Pace GI, Wright ML, Matsumoto H, Anderson RCE, et al. Best practices in intraoperative neuromonitoring in spine deformity surgery: development of an intraoperative checklist to optimize response. Spine Deform. 2014;2:333–9.
Roberts SB, Tsirikos AI. Paediatric spinal deformity surgery: complications and their management. Healthcare. 2022;10:2519.
Cheh G, Lenke LG, Padberg AM, Kim YJ, Daubs MD, Kuhns C, et al. Loss of spinal cord monitoring signals in children during thoracic kyphosis correction with spinal osteotomy: why does it occur and what should you do? Spine. 2008;33:1093–9.
Wang Xbin, Lenke LG, Thuet E, Blanke K, Koester LA, Roth M. Deformity angular ratio describes the severity of spinal deformity and predicts the risk of neurologic deficit in posterior vertebral column resection surgery. Spine. 2016;41:1447.
Dubousset J, Herring JA, Shufflebarger H. The crankshaft phenomenon. J Pediatr Orthop. 1989;9:541–50.
Kioschos HC, Asher MA, Lark RG, Harner EJ. Overpowering the crankshaft mechanism: the effect of posterior spinal fusion with and without stiff transpedicular fixation on anterior spinal column growth in immature canines. Spine. 1996;21:1168–73.
Roberto RF, Lonstein JE, Winter RB, Denis F. Curve progression in Risser stage 0 or 1 patients after posterior spinal fusion for idiopathic scoliosis. J Pediatr Orthop. 1997;17:718–25.
Sanders JO, Herring JA, Browne RH. Posterior arthrodesis and instrumentation in the immature (Risser-grade-0) spine in idiopathic scoliosis. J Bone Joint Surg Am. 1995;77:39–45.
Hamill CL, Bridwell KH, Lenke LG, Chapman MP, Baldus C, Blanke K. Posterior arthrodesis in the skeletally immature patient. Assessing the risk for crankshaft: is an open triradiate cartilage the answer. Spine. 1997;22:1343–51.
Burton DC, Asher MA, Lai SM. Scoliosis correction maintenance in skeletally immature patients with idiopathic scoliosis: is anterior fusion really necessary? Spine. 2000;25:61.
Author information
Authors and Affiliations
Contributions
Rajat Mahajan: Treating surgeon, revising manuscript, supplying images. Ganesh Kumar: Collecting consent, writing and revising the manuscript, conducting the review. Correspondence and requests for materials should be addressed to Ganesh Kumar.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Ethics approval was waived by our institution’s Institutional Review Board. Consent to participate was obtained from the patients and their parents.
Consent for publication
Consent to publish was obtained from the patients and their parents.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mahajan, R., Kumar, G. Is deformity correction essential in a “Myelopathic Cord”? – A case series. Spinal Cord Ser Cases 10, 61 (2024). https://doi.org/10.1038/s41394-024-00676-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-024-00676-9