Abstract
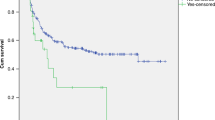
Transplant-associated thrombotic microangiopathy (TA-TMA) is an increasingly recognized complication in hematopoietic cell transplantation (HCT). Given the rarity of prospective pediatric studies on TA-TMA, this study aimed to evaluate the incidence, survival outcomes, and risk factors for predicting early the development of TA-TMA in a pediatric population following allogeneic HCT. We conducted a prospective analysis of 173 pediatric patients to evaluate the incidence, survival outcome, and risk factors of TA-TMA. The cumulative incidence of TA-TMA at one-year post-HCT was 4.7% (95% CI, 2.2–8.6%). Patients with TA-TMA showed significantly poorer 1-year overall survival (OS) rate, 50.0% ± 17.7% compared to 85.4% ± 2.8% in those without TA-TMA (p = 0.008). Additionally, the non-relapse mortality (NRM) rate was higher in the TA-TMA group at 12.5% (95% CI, 3.7–55.8%) versus 7.0% (95% CI, 2.8–10.1%) (p = 0.598). A urine protein/creatinine ratio ≥ 1 mg/mg on day 30 post-HCT was significantly associated with TA-TMA occurrence (adjusted HR, 9.5; [95% CI], 1.28–70.39; p = 0.028). This study showed the significantly unfavorable clinical outcomes associated with TA-TMA in pediatric patients and emphasized the importance of early identification of patients at risk. Further research is needed to explore additional strategies for early detection and intervention to improve outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Li A, Bhatraju PK, Chen J, Chung DW, Hilton T, Houck K, et al. Prognostic biomarkers for thrombotic microangiopathy after acute graft-versus-host disease: a nested case-control study. Transpl Cell Ther. 2021;27:308.e301–e308. https://doi.org/10.1016/j.jtct.2020.12.010.
Uderzo C, Bonanomi S, Busca A, Renoldi M, Ferrari P, Iacobelli M, et al. Risk factors and severe outcome in thrombotic microangiopathy after allogeneic hematopoietic stem cell transplantation. Transplantation. 2006;82:638–44. https://doi.org/10.1097/01.tp.0000230373.82376.46.
Jodele S, Fukuda T, Vinks A, Mizuno K, Laskin BL, Goebel J, et al. Eculizumab therapy in children with severe hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Biol Blood Marrow Transplant. 2014;20:518–25. https://doi.org/10.1016/j.bbmt.2013.12.565.
Jodele S, Davies SM, Lane A, Khoury J, Dandoy C, Goebel J, et al. Diagnostic and risk criteria for HSCT-associated thrombotic microangiopathy: a study in children and young adults. Blood. 2014;124:645–53. https://doi.org/10.1182/blood-2014-03-564997.
Jodele S, Dandoy CE, Myers KC, El-Bietar J, Nelson A, Wallace G, et al. New approaches in the diagnosis, pathophysiology, and treatment of pediatric hematopoietic stem cell transplantation-associated thrombotic microangiopathy. Transfus Apher Sci. 2016;54:181–90. https://doi.org/10.1016/j.transci.2016.04.007.
Jodele S, Sabulski A. Transplant-associated thrombotic microangiopathy: elucidating prevention strategies and identifying high-risk patients. Expert Rev Hematol. 2021;14:751–63. https://doi.org/10.1080/17474086.2021.1960816.
Jodele S, Laskin BL, Dandoy CE, Myers KC, El-Bietar J, Davies SM, et al. A new paradigm: diagnosis and management of HSCT-associated thrombotic microangiopathy as multi-system endothelial injury. Blood Rev. 2015;29:191–204. https://doi.org/10.1016/j.blre.2014.11.001.
Dvorak CC, Higham C, Shimano KA. Transplant-associated thrombotic microangiopathy in pediatric hematopoietic cell transplant recipients: a practical approach to diagnosis and management. Front Pediatr. 2019;7:133. https://doi.org/10.3389/fped.2019.00133.
Schoettler ML, Carreras E, Cho B, Dandoy CE, Ho VT, Jodele S, et al. Harmonizing definitions for diagnostic criteria and prognostic assessment of transplantation-associated thrombotic microangiopathy: a report on behalf of the european society for blood and marrow transplantation, american society for transplantation and cellular therapy, Asia-Pacific blood and marrow transplantation group, and center for international blood and marrow transplant research. Transpl Cell Ther. 2023;29:151–63. https://doi.org/10.1016/j.jtct.2022.11.015.
Young JA, Pallas CR, Knovich MA. Transplant-associated thrombotic microangiopathy: theoretical considerations and a practical approach to an unrefined diagnosis. Bone Marrow Transplant. 2021;56:1805–17. https://doi.org/10.1038/s41409-021-01283-0.
Ramgopal A, Sridar S, Dalal J, Kalpatthi R. Thrombotic microangiopathy: multi-institutional review of pediatric patients who underwent HSCT. J Pers Med. 2021;11:467. https://doi.org/10.3390/jpm11060467.
Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. https://doi.org/10.1186/cc5713.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120:c179–84. https://doi.org/10.1159/000339789.
Koh KN, Sunkara A, Kang G, Sooter A, Mulrooney DA, Triplett B, et al. Acute kidney injury in pediatric patients receiving allogeneic hematopoietic cell transplantation: incidence, risk factors, and outcomes. Biol Blood Marrow Transplant. 2018;24:758–64. https://doi.org/10.1016/j.bbmt.2017.11.021.
Stevens PE, Levin A.Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the kidney disease: improving global outcomes 2012 clinical practice guideline. Ann Intern Med. 2013;158:825–30. https://doi.org/10.7326/0003-4819-158-11-201306040-00007.
Lameire NH, Levin A, Kellum JA, Cheung M, Jadoul M, Winkelmayer WC, et al. Harmonizing acute and chronic kidney disease definition and classification: report of a kidney disease: improving global outcomes (KDIGO) consensus conference. Kidney Int. 2021;100:516–26. https://doi.org/10.1016/j.kint.2021.06.028.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995;15:825–8.
Lee SJ, Vogelsang G, Flowers ME. Chronic graft-versus-host disease. Biol Blood Marrow Transplant 2003;9:215–33. https://doi.org/10.1053/bbmt.2003.50026.
Akil A, Zhang Q, Mumaw CL, Raiker N, Yu J, de Mendizabal NV, et al. Biomarkers for diagnosis and prognosis of sinusoidal obstruction syndrome after hematopoietic cell transplantation. Biol Blood Marrow Transplant 2015;21:1739–45. https://doi.org/10.1016/j.bbmt.2015.07.004.
Bajwa RPS, Mahadeo KM, Taragin BH, Dvorak CC, McArthur J, Jeyapalan A, et al. Consensus report by pediatric acute lung injury and sepsis investigators and pediatric blood and marrow transplantation consortium joint working committees: supportive care guidelines for management of veno-occlusive disease in children and adolescents, Part 1: focus on investigations, prophylaxis, and specific treatment. Biol Blood Marrow Transplant 2017;23:1817–25. https://doi.org/10.1016/j.bbmt.2017.07.021.
Jones RJ, Lee KS, Beschorner WE, Vogel VG, Grochow LB, Braine HG, et al. Venoocclusive disease of the liver following bone marrow transplantation. Transplantation. 1987;44:778–83. https://doi.org/10.1097/00007890-198712000-00011.
McDonald GB, Sharma P, Matthews DE, Shulman HM, Thomas ED. Venocclusive disease of the liver after bone marrow transplantation: diagnosis, incidence, and predisposing factors. Hepatology. 1984;4:116–22. https://doi.org/10.1002/hep.1840040121.
Chemaly RF, Chou S, Einsele H, Griffiths P, Avery R, Razonable RR, et al. Definitions of resistant and refractory cytomegalovirus infection and disease in transplant recipients for use in clinical trials. Clin Infect Dis. 2019;68:1420–6. https://doi.org/10.1093/cid/ciy696.
Ljungman P, Boeckh M, Hirsch HH, Josephson F, Lundgren J, Nichols G, et al. Definitions of cytomegalovirus infection and disease in transplant patients for use in clinical trials. Clin Infect Dis. 2017;64:87–91. https://doi.org/10.1093/cid/ciw668.
Li SS, Zhang N, Jia M, Su M. Association between cytomegalovirus and epstein-barr virus co-reactivation and hematopoietic stem cell transplantation. Front Cell Infect Microbiol. 2022;12:818167. https://doi.org/10.3389/fcimb.2022.818167.
Donnelly JP, Chen SC, Kauffman CA, Steinbach WJ, Baddley JW, Verweij PE, et al. Revision and update of the consensus definitions of invasive fungal disease from the European organization for research and treatment of cancer and the mycoses study group education and research consortium. Clin Infect Dis. 2020;71:1367–76. https://doi.org/10.1093/cid/ciz1008.
Kousha M, Tadi R, Soubani AO. Pulmonary aspergillosis: a clinical review. Eur Respir Rev. 2011;20:156–74. https://doi.org/10.1183/09059180.00001011.
Kanj A, Abdallah N, Soubani AO. The spectrum of pulmonary aspergillosis. Respir Med. 2018;141:121–31. https://doi.org/10.1016/j.rmed.2018.06.029.
Law YM, Hoyer AW, Reller MD, Silberbach M. Accuracy of plasma B-type natriuretic peptide to diagnose significant cardiovascular disease in children: the Better Not Pout Children! Study. J Am Coll Cardiol. 2009;54:1467–75. https://doi.org/10.1016/j.jacc.2009.06.020.
Snowden JA, Hill GR, Hunt P, Carnoutsos S, Spearing RL, Espiner E, et al. Assessment of cardiotoxicity during haemopoietic stem cell transplantation with plasma brain natriuretic peptide. Bone Marrow Transplant. 2000;26:309–13. https://doi.org/10.1038/sj.bmt.1702507.
Rifai N Tietz textbook of clinical chemistry and molecular diagnostics, 6th edn Saunders: St. Louis, 2017.
Schoettler M, Lehmann LE, Margossian S, Lee M, Kean LS, Kao PC, et al. Risk factors for transplant-associated thrombotic microangiopathy and mortality in a pediatric cohort. Blood Adv. 2020;4:2536–47. https://doi.org/10.1182/bloodadvances.2019001242.
Cho BS, Yahng SA, Lee SE, Eom KS, Kim YJ, Kim HJ, et al. Validation of recently proposed consensus criteria for thrombotic microangiopathy after allogeneic hematopoietic stem-cell transplantation. Transplantation. 2010;90:918–26. https://doi.org/10.1097/TP.0b013e3181f24e8d.
Labrador J, Lopez-Corral L, Lopez-Godino O, Vazquez L, Cabrero-Calvo M, Perez-Lopez R, et al. Risk factors for thrombotic microangiopathy in allogeneic hematopoietic stem cell recipients receiving GVHD prophylaxis with tacrolimus plus MTX or sirolimus. Bone Marrow Transplant. 2014;49:684–90. https://doi.org/10.1038/bmt.2014.17.
Choi CM, Schmaier AH, Snell MR, Lazarus HM. Thrombotic microangiopathy in haematopoietic stem cell transplantation: diagnosis and treatment. Drugs. 2009;69:183–98. https://doi.org/10.2165/00003495-200969020-00004.
Bethge WA, Eyrich M, Mielke S, Meisel R, Niederwieser D, Schlegel PG, et al. Results of a multicenter phase I/II trial of TCRalphabeta and CD19-depleted haploidentical hematopoietic stem cell transplantation for adult and pediatric patients. Bone Marrow Transplant. 2022;57:423–30. https://doi.org/10.1038/s41409-021-01551-z.
Bertaina A, Zecca M, Buldini B, Sacchi N, Algeri M, Saglio F, et al. Unrelated donor vs HLA-haploidentical alpha/beta T-cell- and B-cell-depleted HSCT in children with acute leukemia. Blood. 2018;132:2594–607. https://doi.org/10.1182/blood-2018-07-861575.
Pagliuca S, Michonneau D, Sicre de Fontbrune F, Sutra del Galy A, Xhaard A, Robin M, et al. Allogeneic reactivity–mediated endothelial cell complications after HSCT: a plea for consensual definitions. Blood Adv. 2019;3:2424–35.
Gavriilaki E, Sakellari I, Anagnostopoulos A, Brodsky RA. Transplant-associated thrombotic microangiopathy: opening Pandora’s box. Bone Marrow Transplant. 2017;52:1355–60. https://doi.org/10.1038/bmt.2017.39.
Arai Y, Yamashita K, Mizugishi K, Watanabe T, Sakamoto S, Kitano T, et al. Serum neutrophil extracellular trap levels predict thrombotic microangiopathy after allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2013;19:1683–9. https://doi.org/10.1016/j.bbmt.2013.09.005.
Oran B, Donato M, Aleman A, Hosing C, Korbling M, Detry MA, et al. Transplant-associated microangiopathy in patients receiving tacrolimus following allogeneic stem cell transplantation: risk factors and response to treatment. Biol Blood Marrow Transplant. 2007;13:469–77. https://doi.org/10.1016/j.bbmt.2006.11.020.
Daly AS, Hasegawa WS, Lipton JH, Messner HA, Kiss TL. Transplantation-associated thrombotic microangiopathy is associated with transplantation from unrelated donors, acute graft-versus-host disease and venoocclusive disease of the liver. Transfus Apher Sci. 2002;27:3–12. https://doi.org/10.1016/S1473-0502(02)00020-4.
Dandoy CE, Davies SM, Hirsch R, Chima RS, Paff Z, Cash M, et al. Abnormal echocardiography 7 days after stem cell transplantation may be an early indicator of thrombotic microangiopathy. Biol Blood Marrow Transplant. 2015;21:113–8. https://doi.org/10.1016/j.bbmt.2014.09.028.
Liem DA, Cadeiras M, Setty SP. Insights and perspectives into clinical biomarker discovery in pediatric heart failure and congenital heart disease—a narrative review. Cardiovasc Diagn Ther. 2023;13:83–99. https://doi.org/10.21037/cdt-22-386.
Teixeira J, Guillaume M, Nellessen E, Chapelle JP. BNP and NT-proBNP: reference values and cutoff limits [In French]. Rev Med Liege. 2012;67:38–43.
Auerbach SR, Richmond ME, Lamour JM, Blume ED, Addonizio LJ, Shaddy RE, et al. BNP levels predict outcome in pediatric heart failure patients: post hoc analysis of the pediatric carvedilol trial. Circ Heart Fail. 2010;3:606–11. https://doi.org/10.1161/CIRCHEARTFAILURE.109.906875.
Mueller C, McDonald K, de Boer RA, Maisel A, Cleland JGF, Kozhuharov N, et al. Heart Failure Association of the European Society of Cardiology practical guidance on the use of natriuretic peptide concentrations. Eur J Heart Fail. 2019;21:715–31. https://doi.org/10.1002/ejhf.1494.
Schoettler M, Carreras E, Cho B, Dandoy C, Ho V, Jodele S, et al. Harmonizing definitions for diagnostic criteria and prognostic assessment of transplantation-associated thrombotic microangiopathy: a report on behalf of the European Society for Blood and Marrow Transplantation, American Society for Transplantation and Cellular Therapy, Asia-Pacific Blood and Marrow Transplantation Group, and Center for International Blood and Marrow Transplant Research. Transplant Cell Ther. 2023;29:151–63.
Acknowledgements
This study was supported by a grant 2022IF0007 from the Asan Institute for Life Sciences, and donated funds of Asan Medical Center, Seoul, Korea. The statistical analyses conducted in this study were advised by the Department of Medical Statistics at Asan Medical Center.
Author information
Authors and Affiliations
Contributions
KN Koh conceptualized, designed and supervised this study. SH Yoon analyzed and interpreted the patient data. SH Yoon prepared figures, performed statistical analysis, and wrote the manuscript. All authors read and approved the final manuscript; and SH Kang, Hyery Kim, ES Choi, HJ Im provided vital conceptual insights for study design, assisted with study subject accrual and data collection, and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the ethical standards of the Helsinki Declaration and were approved by the Asan Medical Center’s institutional review board (IRB No. 2018-0560). Written informed consent was obtained from all children and patients legal guardians prior to recruitment in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yoon, S.H., Kang, S.H., Kim, H. et al. Incidence, risk factors, and outcomes of transplant-associated thrombotic microangiopathy in pediatric patients after allogeneic hematopoietic cell transplantation: a single-institution prospective study. Bone Marrow Transplant 60, 447–457 (2025). https://doi.org/10.1038/s41409-024-02506-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-024-02506-w