Abstract
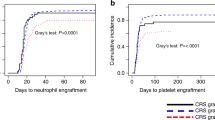
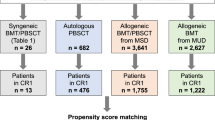
This study assessed 552 allogeneic hematopoietic cell transplantation (HCT) recipients with posttransplant cyclophosphamide (PTCy) to evaluate the incidence, characteristics, risk factors, and impact of early posttransplant cytokine release syndrome (CRS) on outcomes. The cohort included 36% matched sibling donors (MSD), 34% matched unrelated donors (MUD), 27% haploidentical donors, and 4% mismatched unrelated donors (MMUD). CRS was observed in 182 patients, with the highest incidence in haploidentical transplants (80%) compared to MMUD (32%), MUD (23%), and MSD (8%). Most CRS cases were mild, with 93% classified as grade 1 and 6% as grade 2, with only one severe case of grade 3. In haploidentical transplants, CRS was linked to a lower risk of severe chronic graft-versus-host disease (GVHD) and non-relapse mortality (NRM), leading to improved overall survival. In contrast, among HLA-matched recipients (MSD and MUD), there were no significant differences in outcomes between those with or without CRS. However, subgroup analysis revealed that CRS in patients with myeloid malignancies, including acute myeloid leukemia, myelodysplastic syndromes, and myeloproliferative neoplasms, was associated with a reduced relapse rate, improving survival outcomes. In conclusion, while CRS is typically mild and short-lived, it significantly impacts survival, particularly in haploidentical transplants and HLA-matched patients with myeloid malignancies.
Key points
-
CRS in haploidentical transplants is linked to lower severe chronic GVHD and NRM, improving survival outcomes.
-
In HLA-matched HSCT recipients with myeloid neoplasms, CRS reduces relapse rates, improving OS and DFS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The dataset supporting the conclusions of this article are available in the Hematology department of the Hospital Universitari i Politècnic La Fe, València, Spain: [email protected].
References
Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–95.
Lee DW, Santomasso BD, Locke FL, Ghobadi A, Turtle CJ, Brudno JN, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transpl. 2019;25:625–38.
Crombie JL, Graff T, Falchi L, Karimi YH, Bannerji R, Nastoupil L, et al. Consensus recommendations on the management of toxicity associated with CD3×CD20 bispecific antibody therapy. Blood. 2024;143:1565–75.
Imus PH, Blackford AL, Bettinotti M, Luznik L, Fuchs EJ, Huff CA. et al. Severe cytokine release syndrome after haploidentical peripheral blood stem cell transplantation. Biol Blood Marrow Transpl. 2019;25:2431–7. https://linkinghub.elsevier.com/retrieve/pii/S1083879119304999.
Abboud R, Wan F, Mariotti J, Arango M, Castagna L, Romee R. et al. Cytokine release syndrome after haploidentical hematopoietic cell transplantation: an international multicenter analysis. Bone Marrow Transpl. 2021;56:2763–70. https://www.nature.com/articles/s41409-021-01403-w.
Otoukesh S, Elmariah H, Yang D, Clark MC, Siraj M, Ali H. et al. Cytokine release syndrome following peripheral blood stem cell haploidentical hematopoietic cell transplantation with post-transplantation cyclophosphamide. Transpl Cell Ther. 2022;28:111.e1–111.e8. https://linkinghub.elsevier.com/retrieve/pii/S266663672101397X.
De Togni E, Wan F, Slade M, Plach K, Abboud R. The impact of tocilizumab treatment for cytokine release syndrome on the incidence of early blood stream infections after peripheral blood haploidentical hematopoietic cell transplantation. Leuk Lymphoma. 2022;63:2975–81. https://www.tandfonline.com/doi/full/10.1080/10428194.2022.2100367.
Shapiro RM, Kim HT, Ansuinelli M, Guleria I, Cutler CS, Koreth J. et al. Cytokine release syndrome in haploidentical stem cell transplant may impact T-cell recovery and relapse. Blood Adv. 2023;7:4080–8. https://ashpublications.org/bloodadvances/article/7/15/4080/495948/Cytokine-release-syndrome-in-haploidentical-stem.
McCurdy SR, Muth ST, Tsai HL, Symons HJ, Huff CA, Matsui WH. et al. Early Fever after Haploidentical Bone Marrow Transplantation Correlates with Class II HLA-Mismatching and Myeloablation but Not Outcomes. Biol Blood Marrow Transpl. 2018;24:2056–64. https://linkinghub.elsevier.com/retrieve/pii/S1083879118303161.
Solán L, Landete E, Bailén R, Dorado N, Oarbeascoa G, Anguita J, et al. Cytokine release syndrome after allogeneic stem cell transplantation with posttransplant cyclophosphamide. Hematol Oncol. 2020;38:597–603.
Rappazzo KC, Zahurak M, Bettinotti M, Ali SA, Ambinder AJ, Bolaños-Meade J, et al. Nonmyeloablative, HLA-Mismatched unrelated peripheral blood transplantation with high-dose post-transplantation cyclophosphamide. Transplant Cell Ther. 2021;27:909.e1–909.e6.
von dem Borne PA, Kemps-Mols BM, de Wreede LC, van Beek AA, Snijders TJF, van Lammeren D, et al. The degree of HLA matching determines the incidence of cytokine release syndrome and associated nonrelapse mortality in matched related and unrelated allogeneic stem cell transplantation with post-transplant cyclophosphamide. Leuk Lymphoma. 2024;65:1270–80.
Montoro J, Piñana JL, Hernández-Boluda JC, Hernani R, Lorenzo I, Pérez A, et al. Uniform graft-versus-host disease prophylaxis with posttransplant cyclophosphamide, sirolimus, and mycophenolate mofetil following hematopoietic stem cell transplantation from haploidentical, matched sibling and unrelated donors. Bone Marrow Transplant. 2020;55:2147–59.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33. https://doi.org/10.1016/j.bbmt.2009.07.004.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health consensus development project on criteria for clinical trials in Chronic Graft-versus-Host Disease: I. The 2014 Diagnosis and Staging Working Group Report. Biol Blood Marrow Transpl. 2015;21:389–401.e1.
Penack O, Marchetti M, Aljurf M, Arat M, Bonifazi F, Duarte RF, et al. Prophylaxis and management of graft-versus-host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2024;11:e147–59.
Sureda A, Carpenter PA, Bacigalupo A, Bhatt VR, de la Fuente J, Ho A, et al. Harmonizing definitions for hematopoietic recovery, graft rejection, graft failure, poor graft function, and donor chimerism in allogeneic hematopoietic cell transplantation: a report on behalf of the EBMT, ASTCT, CIBMTR, and APBMT. Bone Marrow Transpl. 2024;59:832–7.
Harris AC, Young R, Devine S, Hogan WJ, Ayuk F, Bunworasate U, et al. International, Multicenter Standardization of Acute Graft-versus-Host Disease Clinical Data Collection: A Report from the Mount Sinai Acute GVHD International Consortium. Biol Blood Marrow Transpl. 2016;22:4–10.
Mohty M, Malard F, Alaskar AS, Aljurf M, Arat M, Bader P, et al. Diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a refined classification from the European society for blood and marrow transplantation (EBMT). Bone Marrow Transpl. 2023;58:749–54.
McCurdy SR, Luznik L. Post-transplantation cyclophosphamide for chimerism-based tolerance. Bone Marrow Transpl. 2019;54:769–74.
Sanz J, Galimard JE, Labopin M, Afanasyev B, Angelucci E, Ciceri F, et al. Post-transplant cyclophosphamide after matched sibling, unrelated and haploidentical donor transplants in patients with acute myeloid leukemia: a comparative study of the ALWP EBMT. J Hematol Oncol. 2020;13:46.
Sanz J, Galimard JE, Labopin M, Afanasyev B, Sergeevich MI, Angelucci E, et al. Post-transplant cyclophosphamide containing regimens after matched sibling, matched unrelated and haploidentical donor transplants in patients with acute lymphoblastic leukemia in first complete remission, a comparative study of the ALWP of the EBMT. J Hematol Oncol. 2021;14:84.
Montoro J, Boumendil A, Finel H, Bramanti S, Castagna L, Blaise D, et al. Post-Transplantation Cyclophosphamide-Based Graft-versus-Host Disease Prophylaxis in HLA-Matched and Haploidentical Donor Transplantation for Patients with Hodgkin Lymphoma: A Comparative Study of the Lymphoma Working Party of the European Society for Blood and Marrow Transplantation. Transplant Cell Ther. 2024;30:210.e1–210.e14.
Author information
Authors and Affiliations
Contributions
RB, MAS and JS designed the study, performed statistical analysis, interpreted the results and wrote the original draft. JM, AB, MV, PC, PG, PA, IG, PS, MS, BL, AB, JE, DM, PLL, AL, PR, AP and JdlR critically reviewed the study design, maintained the database and reviewed and edited the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The hospital’s Institutional Review Board approved the protocol, and written informed consent was obtained from all patients in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benavente, R., Montoro, J., Balaguer-Roselló, A. et al. Cytokine release syndrome: implications for transplant outcomes in haploidentical and HLA-matched HSCT using PTCy. Bone Marrow Transplant (2025). https://doi.org/10.1038/s41409-025-02594-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41409-025-02594-2