Abstract
Background
Little research has been conducted on the relationship between statin use and the survival of head and neck cancer patients. This study assessed whether statin use after head and neck cancer diagnosis is associated with overall survival among patients in the U.S. military health system (MHS) that provides universal health care to its beneficiaries.
Methods
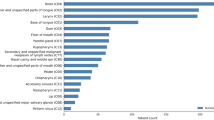
The study included 1842 patients with head and neck squamous cell carcinoma (HNSCC) from MHS. Statin use was extracted from the pharmacy database of the Military Health System Data Repository (MDR). Time-dependent multivariate Cox proportional hazards models were used to assess the relationship between post-diagnosis statin use and overall survival with the adjustment for potential confounders.
Results
Compared to non-users, increased post-diagnosis cumulative use of statins (per one-year of use) conferred a significant improved survival with adjusted hazard ratio (HR) of 0.70 (95% Confidence Interval, CI = 0.55 to 0.90). When analysis was stratified by status of statin use prior to HNSCC diagnosis, the HRs were 0.31 (95% CI = 0.15–0.65) and 0.81 (95% CI = 0.59–1.11) for post-diagnosis users who also used it before HNSCC diagnosis and those who only used it after the diagnosis, respectively.
Conclusion
Prolonged statin use was associated with improved survival among HNSCC patients in MHS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
269,00 € per year
only 11,21 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The dataset generated during and/or analyzed during the current study is not publicly available following DoD MHS regulations.
References
American Cancer Society, Cancer Facts and Figures 2022: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2022/2022-cancer-facts-and-figures.pdf. Accessed 14 Nov 2022.
American Cancer Society, Survival Rates for Oral Cavity and Oropharyngeal Cancer: https://www.cancer.org/cancer/oral-cavity-and-oropharyngeal-cancer/detection-diagnosis-staging/survival-rates.html. Accessed 14 Nov 2022.
Gauthaman K, Fong CY, Bongso A. Statins, stem cells, and cancer. J Cell Biochem. 2009;106:975–83.
Chan KK, Oza AM, Siu LL. The statins as anticancer agents. Clin Cancer Res. 2003;9:10–19.
Demierre MF, Higgins PD, Gruber SB, Hawk E, Lippman SM. Statins and cancer prevention. Nat Rev Cancer. 2005;5:930–42.
Mei Z, Liang M, Li L, Zhang Y, Wang Q, Yang W. Effects of statins on cancer mortality and progression: a systematic review and meta-analysis of 95 cohorts including 1,111,407 individuals. Int J Cancer. 2017;140:1068–81.
Cardwell CR, Hicks BM, Hughes C, Murray LJ. Statin use after diagnosis of breast cancer and survival: a population-based cohort study. Epidemiology. 2015;26:68–78.
Leiter A, Bickell NA, LeRoith D, Nayak A, Feldman SM, Friedman NB. Statin use and breast cancer prognosis in black and white women. Horm Cancer. 2018;9:55–61.
Marcella SW, David A, Ohman-Strickland PA, Carson J, Rhoads GG. Statin use and fatal prostate cancer: a matched case-control study. Cancer. 2012;118:4046–52.
Borgquist S, Broberg P, Tojjar J, Olsson H. Statin use and breast cancer survival - a Swedish nationwide study. BMC Cancer. 2019;19:54.
Gray RT, Coleman HG, Hughes C, Murray LJ, Cardwell CR. Statin use and survival in colorectal cancer: Results from a population-based cohort study and an updated systematic review and meta-analysis. Cancer Epidemiol. 2016;45:71–81.
Getz KR, Bellile E, Zarins KR, Rullman C, Chinn SB, Taylor JMG. Statin use and head and neck squamous cell carcinoma outcomes. Int J Cancer. 2020;10:2440–8.
Gupta A, Stokes W, Eguchi M, Hararah M, Amini A, Mueller A. Statin use associated with improved overall and cancer specific survival in patients with head and neck cancer. Oral Oncol. 2019;90:54–66.
Lebo NL, Griffiths R, Hall S, Dimitroulakos J, Johnson-Obaseki S. Effect of statin use on oncologic outcomes in head and neck squamous cell carcinoma. Head Neck. 2018;40:1697–706.
Suissa S. Immortal time bias in observational studies of drug effects. Pharmacoepidemiol Drug Saf. 2007;16:241–9.
Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008;167:492–9.
Essien UR, Dusetzina SB, Gellad WF. A policy prescription for reducing health disparities-achieving pharmacoequity. JAMA. 2021;326:1793–4.
Walker GV, Grant SR, Guadagnolo BA, Hoffman KE, Smith BD, Koshy M. Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol. 2014;32:3118–25.
TRICARE Rates and Reimbursement: https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/TRICARE-Health-Plan/Rates-and-Reimbursement. Accessed 20 Dec 2022.
Evaluation of the TRICARE Program: Fiscal Year 2021 Report to Congress: https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program. Accessed 21 Dec 2022.
Lin J, Gill A, Zahm SH, Carter CA, Shriver CD, Nations JA, et al. Metformin use and survival after non-small cell lung cancer: a cohort study in the US Military health system. Int J Cancer. 2017;141:254–63.
Eaglehouse YL, Park AB, Georg MW, Brown DW, Lin J, Shao S, et al. Consolidation of cancer registry and administrative claims data on cancer diagnosis and treatment in the US Military Health System. JCO Clin Cancer Inf. 2020;4:906–17.
Defense Health Agency: Military Health System Data Repository, https://www.health.mil/Military-Health-Topics/Technology/Support-Areas/MDR-M2-ICD-Functional-References-and-Specification-Documents. Accessed 14 Dec 2022.
International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3). World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf. Accessed 13 Apr 2021.
Hashim D, Genden E, Posner M, Hashibe M, Boffetta P. Head and neck cancer prevention: from primary prevention to impact of clinicians on reducing burden. Ann Oncol. 2019;30:744–56.
Commission on Cancer, Facility Oncology Registry Data Standards Revised for 2016, American College of Surgeons: https://www.facs.org/quality-programs/cancer-programs/national-cancer-database/ncdb-call-for-data/fordsmanual/ Accessed 17 Feb 2023.
Commission on Cancer, Cancer Program Standards 2012: Ensuring Patient-Centered Care., American College of Surgeons: https://apos-society.org/wp-content/uploads/2016/06/CoCStandards.pdf. Accessed 17 Feb 2023.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83.
Mody MD, Rocco JW, Yom SS, Haddad RI, Saba NF. Head and neck cancer. Lancet. 2021;398:2289–99.
Chow LQM. Head and Neck Cancer. N Engl J Med. 2020;382:60–72.
American Joint Committee on Cancer. AJCC cancer staging manual. 6th ed. In: Greene FL, Page DL, Flemming ID, et al. editors. Chicago, IL: Springer; 2002.
Alkhatib HH, Maroun CA, Amin N, Zhu G, Guller M, Herberg ME, et al. Tumor histological grade and immunotherapy response in patients with recurrent or metastatic head and neck squamous cell carcinoma. JAMA Otolaryngol Head Neck Surg. 2022;148:540–6.
Nielsen SF, Nordestgaard BG, Bojesen SE. Statin use and reduced cancer-related mortality. N Engl J Med. 2012;367:1792–802.
Nguyen T, Khan A, Liu Y, El-Serag HB, Thrift AP. The association between statin use after diagnosis and mortality risk in patients with esophageal cancer: a retrospective cohort study of United States Veterans. Am J Gastroenterol. 2018;113:1310.
Shibata MA, Ito Y, Morimoto J, Otsuki Y. Lovastatin inhibits tumor growth and lung metastasis in mouse mammary carcinoma model: a p53-independent mitochondrial-mediated apoptotic mechanism. Carcinogenesis. 2004;25:1887–98.
Cafforio P, Dammacco F, Gernone A, Silvestris F. Statins activate the mitochondrial pathway of apoptosis in human lymphoblasts and myeloma cells. Carcinogenesis. 2005;26:883–91.
Crick DC, Andres DA, Danesi R, Macchia M, Waechter CJ. Geranylgeraniol overcomes the block of cell proliferation by lovastatin in C6 glioma cells. J Neurochem. 1998;70:2397–405.
Dimitroulakos J, Marhin WH, Tokunaga J, Irish J, Gullane P, Penn LZ, et al. Microarray and biochemical analysis of lovastatin-induced apoptosis of squamous cell carcinomas. Neoplasia. 2002;4:337–46.
Rettig EM, D’Souza G. Epidemiology of head and neck cancer. Surg Oncol Clin N. Am. 2015;24:379–96.
Stein E, Lenze NR, Yarbrough WG, Hayes DN, Mazul A, Sheth S. Systematic review and meta-analysis of racial survival disparities among oropharyngeal cancer cases by HPV status. Head Neck. 2020;42:2985–3001.
Acknowledgements
The authors thank Joint Pathology Center for providing the Central Cancer Registry (CCR) data and the Defense Health Agency for providing the MHS Data Repository (MDR) data.
Funding
This project was supported by Murtha Cancer Center Research Program via Uniformed Services University of the Health Sciences under the auspices of the Henry M. Jackson Foundation for the Advancement of Military Medicine.
Author information
Authors and Affiliations
Contributions
Conception: Lin, Zhu; Data Curation: Lin, Zhu, Shriver; Formal Analysis: Lin; Funding Acquisition: Shriver; Methodology: Lin, Zhu, Orestes, Shriver; Investigation: Lin, Zhu, Orestes, Shriver; Writing –original draft: Lin; Writing-review and editing: Lin, Orestes, Zhu, Shriver
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The MilCanEpi database and its utilization were approved by the Institutional Review Board of the Uniformed Services University of the Health Sciences, and Defense Health Agency (DHA). The study was performed in accordance with the Declaration of Helsinki. The study used deidentified data stored in the MilCanEpi database. Obtaining informed consent does not apply.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J., Orestes, M.I., Shriver, C.D. et al. Post-diagnosis statin use and survival among head and neck cancer patients: a cohort study in a universal health care system. Br J Cancer 132, 259–265 (2025). https://doi.org/10.1038/s41416-024-02925-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-024-02925-y
This article is cited by
-
The role of lipids and lipids lowering drugs in human papillomavirus (HPV) and HPV-associated cancers
Infectious Agents and Cancer (2025)