Abstract
Background and aims
Accumulating evidence supports the effectiveness of moderate-intensity aerobic training on metabolic health, with limited studies investigating change in resting substrate oxidation. The aim of this study was to explore whether 10 weeks of walking-based aerobic training would alter substrate oxidation in postmenopausal women with obesity.
Methods and results
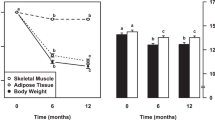
Twenty-four postmenopausal women with obesity who were assigned into the control (n = 12) or exercise groups (n = 12) undertook a 10-week aerobic training program (3 d·week−1) that involved walking exercises at 50–70% of heart rate reserve on a treadmill, with exercise volume increased from 25 to 40 min·day−1. Resting metabolic rate (RMR) and body composition were measured pre- and post-training. Whole-body substrate oxidation was calculated using respiratory data collected during RMR measurement via indirect calorimetry. No significant change was noted (p > 0.05) in resting fat oxidation and carbohydrate oxidation in the exercise group. Resting respiratory exchange ratio and RMR did not alter in response to the training program (p > 0.05).
Conclusion
Our results show that a 10-week of moderate-intensity aerobic training does not modify substrate oxidation in postmenopausal women with obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18:715–23.
Sarma S, Sockalingam S, Dash S. Obesity as a multisystem disease: trends in obesity rates and obesity-related complications. Diabetes Obes Metab. 2021;23:3–16.
Di Angelantonio E, Bhupathiraju ShN, Wormser D, Gao P, Kaptoge S, de Gonzalez AB, et al. Body-mass index and all-cause mortality: individual-participant-data meta-analysis of 239 prospective studies in four continents. Lancet. 2016;388:776–86.
Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018;6:944–53.
Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, Anis AH. The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health. 2009;9:88.
Pi-Sunyer X. The medical risks of obesity. Postgrad Med. 2009;121:21–33.
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism. 2019;92:6–10.
Sipilä S, Törmäkangas T, Sillanpää E, Aukee P, Kujala UM, Kovanen V, et al. Muscle and bone mass in middle-aged women: role of menopausal status and physical activity. J Cachexia Sarcopenia Muscle. 2020;11:698–709.
Fritzen AM, Lundsgaard AM, Kiens B. Tuning fatty acid oxidation in skeletal muscle with dietary fat and exercise. Nat Rev Endocrinol. 2020;16:683–96.
Kelley DE, Mandarino LJ. Fuel selection in human skeletal muscle in insulin resistance: a reexamination. Diabetes. 2000;49:677–83.
Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of obesity among adults and youth: United States, 2015–2016. NCHS Data Brief. 2017;288:1–8.
Melanson KJ, Saltzman E, Russell RR, Roberts SB. Fat oxidation in response to four graded energy challenges in younger and older women. Am J Clin Nutr. 1997;66:860–6.
Nagy TR, Goran MI, Weinsier RL, Toth MJ, Schutz Y, Poehlman ET. Determinants of basal fat oxidation in healthy Caucasians. J Appl Physiol. 1996;80:1743–8.
Zurlo F, Lillioja S, Esposito-Del Puente A, Nyomba BL, Raz I, Saad MF, et al. Low ratio of fat to carbohydrate oxidation as predictor of weight gain: study of 24-h RQ. Am J Physiol. 1990;259:E650–7.
Goodpaster BH, Wolf D. Skeletal muscle lipid accumulation in obesity, insulin resistance, and type 2 diabetes. Pediatr Diabetes. 2004;5:219–26.
Houmard JA. Intramuscular lipid oxidation and obesity. Am J Physiol Regul Integr Comp Physiol. 2008;294:R1111–6.
Goodpaster BH, Theriault R, Watkins SC, Kelley DE. Intramuscular lipid content is increased in obesity and decreased by weight loss. Metabolism 2000;49:467–72.
Perdomo G, Commerford SR, Richard AM, Adams SH, Corkey BE, O’Doherty RM, et al. Increased beta-oxidation in muscle cells enhances insulin-stimulated glucose metabolism and protects against fatty acid-induced insulin resistance despite intramyocellular lipid accumulation. J Biol Chem. 2004;279:27177–86.
Tan A, Thomas RL, Campbell MD, Prior SL, Bracken RM, Churm R. Effects of exercise training on metabolic syndrome risk factors in post-menopausal women—a systematic review and meta-analysis of randomised controlled trials. Clin Nutr. 2023;42:337–51.
Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2:1143–211.
Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25:1–72.
Atakan MM, Kosar SN, Guzel Y, Tin HT, Yan X. The role of exercise, diet, and cytokines in preventing obesity and improving adipose tissue. Nutrients. 2021;13:1459.
Astorino TA, Schubert MM. Changes in fat oxidation in response to various regimes of high-intensity interval training (HIIT). Eur J Appl Physiol. 2018;118:51–63.
Perdomo G, Commerford SR, Richard A-MT, Adams SH, Corkey BE, O’Doherty RM, et al. Increased β-oxidation in muscle cells enhances insulin-stimulated glucose metabolism and protects against fatty acid-induced insulin resistance despite intramyocellular lipid accumulation. J Biol Chem. 2004;279:27177–86.
Dupuit M, Rance M, Morel C, Bouillon P, Pereira B, Bonnet A, et al. Moderate-intensity continuous training or high-intensity interval training with or without resistance training for altering body composition in postmenopausal women. Med Sci Sports Exerc. 2020;52:736–45.
Froehle AW, Hopkins SR, Natarajan L, Schoeninger MJ. Moderate to high levels of exercise are associated with higher resting energy expenditure in community-dwelling postmenopausal women. Appl Physiol Nutr Metab. 2013;38:1147–53.
Zarins ZA, Wallis GA, Faghihnia N, Johnson ML, Fattor JA, Horning MA, et al. Effects of endurance training on cardiorespiratory fitness and substrate partitioning in postmenopausal women. Metabolism. 2009;58:1338–46.
Ortmeyer HK, Goldberg AP, Ryan AS. Exercise with weight loss improves adipose tissue and skeletal muscle markers of fatty acid metabolism in postmenopausal women. Obesity. 2017;25:1246–53.
Lee IM, Buchner DM. The importance of walking to public health. Med Sci Sports Exerc. 2008;40:S512–8.
Rhodes RE, Martin AD, Taunton JE, Rhodes EC, Donnelly M, Elliot J. Factors associated with exercise adherence among older adults. An individual perspective. Sports Med. 1999;28:397–411.
Yamazaki S, Ichimura S, Iwamoto J, Takeda T, Toyama Y. Effect of walking exercise on bone metabolism in postmenopausal women with osteopenia/osteoporosis. J Bone Min Metab. 2004;22:500–8.
Morris JN, Hardman AE. Walking to health. Sports Med. 1997;23:306–32.
Ratjen I, Morze J, Enderle J, Both M, Borggrefe J, Müller H-P, et al. Adherence to a plant-based diet in relation to adipose tissue volumes and liver fat content. Am J Clin Nutr. 2020;112:354–63.
Lanzi S, Codecasa F, Cornacchia M, Maestrini S, Capodaglio P, Brunani A, et al. Short-term HIIT and Fat max training increase aerobic and metabolic fitness in men with class II and III obesity. Obesity 2015;23:1987–94.
Støa EM, Meling S, Nyhus LK, Glenn S, Mangerud KM, Helgerud J, et al. High-intensity aerobic interval training improves aerobic fitness and HbA1c among persons diagnosed with type 2 diabetes. Eur J Appl Physiol. 2017;117:455–67.
Whyte LJ, Gill JM, Cathcart AJ. Effect of 2 weeks of sprint interval training on health-related outcomes in sedentary overweight/obese men. Metabolism. 2010;59:1421–8.
Jabbour G, Mauriege P, Joanisse D, Iancu HD. Effect of supramaximal exercise training on metabolic outcomes in obese adults. J Sports Sci. 2017;35:1975–81.
Dishman RK, Buckworth J. Increasing physical activity: a quantitative synthesis. Med Sci Sports Exerc. 1996;28:706–19.
Ekkekakis P, Parfitt G, Petruzzello SJ. The pleasure and displeasure people feel when they exercise at different intensities: decennial update and progress towards a tripartite rationale for exercise intensity prescription. Sports Med. 2011;41:641–71.
Hardcastle SJ, Ray H, Beale L, Hagger MS. Why sprint interval training is inappropriate for a largely sedentary population. Front Psychol. 2014; 5,121376.
Biddle SJ, Batterham AM. High-intensity interval exercise training for public health: a big HIT or shall we HIT it on the head? Int J Behav Nutr Phys Act. 2015;12:1–8.
Atakan MM, Li Y, Koşar Ş N, Turnagöl HH, Yan X. Evidence-based effects of high-intensity interval training on exercise capacity and health: a review with historical perspective. Int J Environ Res Public Health. 2021;18,7201.
Asikainen T-M, Kukkonen-Harjula K, Miilunpalo S. Exercise for health for early postmenopausal women. Sports Med. 2004;34:753–78.
Carroll JF, Pollock ML, Graves JE, Leggett SH, Spitler DL, Lowenthal DT. Incidence of injury during moderate-and high-intensity walking training in the elderly. J Gerontol. 1992;47:M61–M6.
Cononie CC, Graves JE, Pollock ML, Phillips MI, Sumners C, Hagberg JM. Effect of exercise training on blood pressure in 70-to 79-year-old men and women. Med Sci Sports Exerc. 1991;23:505–11.
Hootman JM, Macera CA, Ainsworth BE, Martin M, Addy CL, Blair SN. Association among physical activity level, cardiorespiratory fitness, and risk of musculoskeletal injury. Am J Epidemiol. 2001;154:251–8.
Pollock ML, Carroll JF, Graves JE, Leggett SH, Braith RW, Limacher M, et al. Injuries and adherence to walk/jog and resistance training programs in the elderly. Med Sci Sports Exerc. 1991;23:1194–200.
Fields KB, Sykes JC, Walker KM, Jackson JC. Prevention of running injuries. Curr Sports Med Rep. 2010;9:176–82.
Hootman JM, Macera CA, Ainsworth BE, Addy CL, Martin M, Blair SN. Epidemiology of musculoskeletal injuries among sedentary and physically active adults. Med Sci Sports Exerc. 2002;34:838–44.
Romani WA, Gallicchio L, Flaws JA. The association between physical activity and hot flash severity, frequency, and duration in mid‐life women. Am J Hum Biol. 2009;21:127–9.
Lee I-M, Skerrett PJ. Physical activity and all-cause mortality: what is the dose-response relation? Med Sci Sports Exerc. 2001;33:S459–S71.
Manson JE, Greenland P, LaCroix AZ, Stefanick ML, Mouton CP, Oberman A, et al. Walking compared with vigorous exercise for the prevention of cardiovascular events in women. N Engl J Med. 2002;347:716–25.
Church TS, Earnest CP, Skinner JS, Blair SN. Effects of different doses of physical activity on cardiorespiratory fitness among sedentary, overweight or obese postmenopausal women with elevated blood pressure: a randomized controlled trial. JAMA. 2007;297:2081–91.
Asikainen T, Miilunpalo S, Oja P, Rinne M, Pasanen M, Uusi-Rasi K, et al. Randomised, controlled walking trials in postmenopausal women: the minimum dose to improve aerobic fitness? Br J Sports Med. 2002;36:189–94.
Asikainen TM, Miilunpalo S, Kukkonen‐Harjula K, Nenonen A, Pasanen M, Rinne M, et al. Walking trials in postmenopausal women: effect of low doses of exercise and exercise fractionization on coronary risk factors. Scand J Med Sci Sports. 2003;13:284–92.
Martyn-St James M, Carroll S. Meta-analysis of walking for preservation of bone mineral density in postmenopausal women. Bone. 2008;43:521–31.
Guzel Y, Atakan MM, Areta JL, Turnagol HH, Kosar SN. Ten weeks of low-volume walking training improve cardiometabolic health and body composition in sedentary postmenopausal women with obesity without affecting markers of bone metabolism. Res Sports Med. 2022:1–13.
Compher C, Frankenfield D, Keim N, Roth-Yousey L. Group EAW. Best practice methods to apply to measurement of resting metabolic rate in adults: a systematic review. J Am Diet Assoc. 2006;106:881–903.
Weir JB. New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol. 1949;109:1–9.
Frayn KN. Calculation of substrate oxidation rates in vivo from gaseous exchange. J Appl Physiol Respir Environ Exerc Physiol. 1983;55:628–34.
Karvonen MJ. The effects of training on heart rate: a longitudinal study. Ann Med Exp Biol Fenn. 1957;35:307–15.
Schubert MM, Clarke HE, Seay RF, Spain KK. Impact of 4 weeks of interval training on resting metabolic rate, fitness, and health-related outcomes. Appl Physiol Nutr Metab. 2017;42:1073–81.
Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–60.
Hopkins WG. A scale of magnitudes for effect statistics. A new view of statistics. 2002;502:411. www.sportsci.org/resource/stats/effectmag.html.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57:289–300.
Calles-Escandón J, Goran MI, O’Connell M, Nair KS, Danforth JrE. Exercise increases fat oxidation at rest unrelated to changes in energy balance or lipolysis. Am J Physiol Endocrinol Metab. 1996;270:E1009–E14.
Morio B, Montaurier C, Ritz P, Fellmann N, Coudert J, Beaufrere B, et al. Time-course effects of endurance training on fat oxidation in sedentary elderly people. Int J Obes. 1999;23:706–14.
Poehlman ET, Gardner AW, Arciero PJ, Goran MI, Calles-Escandon J. Effects of endurance training on total fat oxidation in elderly persons. J Appl Physiol. 1994;76:2281–7.
Buemann B, Astrup A, Christensen N. Three months aerobic training fails to affect 24-hour energy expenditure in weight-stable, post-obese women. Int J Obes Relat Metab Disord. 1992;16:809–16.
Potteiger JA, Kirk EP, Jacobsen DJ, Donnelly JE. Changes in resting metabolic rate and substrate oxidation after 16 months of exercise training in overweight adults. Int J Sport Nutr Exerc Metab. 2008;18:79–95.
Toth M, Poehlman E. Resting metabolic rate and cardiovascular disease risk in resistance-and aerobic-trained middle-aged women. Int J Obes Relat Metab Disord. 1995;19:691–8.
van Aggel-Leijssen DP, Saris WH, Hul GB, Van Baak MA. Long-term effects of low-intensity exercise training on fat metabolism in weight-reduced obese men. Metab Clin Exp. 2002;51:1003–10.
Sial S, Coggan AR, Hickner RC, Klein S. Training-induced alterations in fat and carbohydrate metabolism during exercise in elderly subjects. Am J Physiol Endocrinol Metab. 1998;274:E785–E90.
Martins C, Kazakova I, Ludviksen M, Mehus I, Wisloff U, Kulseng B, et al. High-intensity interval training and isocaloric moderate-intensity continuous training result in similar improvements in body composition and fitness in obese individuals. Int J Sport Nutr Exerc Metab. 2016;26:197–204.
Amaro-Gahete FJ, De-la OA, Jurado-Fasoli L, Sanchez-Delgado G, Ruiz JR, Castillo MJ. Metabolic rate in sedentary adults, following different exercise training interventions: the FIT-AGEING randomized controlled trial. Clin Nutr. 2020;39:3230–40.
Hirsch KR, Greenwalt CE, Cabre HE, Gould LM, Brewer GJ, Blue MNM, et al. Metabolic effects of high-intensity interval training and essential amino acids. Eur J Appl Physiol. 2021;121:3297–311.
Guadalupe-Grau A, Fernández-Elías VE, Ortega JF, Dela F, Helge JW, Mora-Rodriguez R. Effects of 6-month aerobic interval training on skeletal muscle metabolism in middle-aged metabolic syndrome patients. Scand J Med Sci Sports. 2018;28:585–95.
Goodpaster BH, Sparks LM. Metabolic flexibility in health and disease. Cell Metab. 2017;25:1027–36.
Bishop DJ, Botella J, Genders AJ, Lee MJ, Saner NJ, Kuang J, et al. High-intensity exercise and mitochondrial biogenesis: current controversies and future research directions. Physiology 2019;34:56–70.
Atakan MM, Guzel Y, Shrestha N, Kosar SN, Grgic J, Astorino TA, et al. Effects of high-intensity interval training (HIIT) and sprint interval training (SIT) on fat oxidation during exercise: a systematic review and meta-analysis. Br J Sports Med. 2022;56:988–96.
Bunt JC. Metabolic actions of estradiol: significance for acute and chronic exercise responses. Med Sci Sports Exerc. 1990;22:286–90.
D’Eon TM, Sharoff C, Chipkin SR, Grow D, Ruby BC, Braun B. Regulation of exercise carbohydrate metabolism by estrogen and progesterone in women. Am J Physiol Endocrinol Metab. 2002;283:E1046–55.
Isacco L, Duché P, Boisseau N. Influence of hormonal status on substrate utilization at rest and during exercise in the female population. Sports Med. 2012;42:327–42.
Tarnopolsky MA. Gender differences in substrate metabolism during endurance exercise. Can J Appl Physiol. 2000;25:312–27.
Santa-Clara H, Szymanski L, Ordille T, Fernhall B. Effects of exercise training on resting metabolic rate in postmenopausal African American and Caucasian women. Metabolism. 2006;55:1358–64.
Wilmore JH, Stanforth PR, Hudspeth LA, Gagnon J, Daw EW, Leon AS, et al. Alterations in resting metabolic rate as a consequence of 20 wk of endurance training: the HERITAGE Family study. Am J Clin Nutr. 1998;68:66–71.
Jennings A, Alberga A, Sigal R, Jay O, BoulE N, Kenny G. The effect of exercise training on resting metabolic rate in type 2 diabetes mellitus. Med Sci Sports Exerc. 2009;41:1558.
Tremblay A, Fontaine E, Poehlman E, Mitchell D, Perron L, Bouchard C. The effect of exercise-training on resting metabolic rate in lean and moderately obese individuals. Int J Obes. 1986;10:511–7.
Stefanska A, Bergmann K, Sypniewska G. Metabolic syndrome and menopause: pathophysiology, clinical and diagnostic significance. In: Makowski GS, editor. Advances in clinical chemistry. 72: Elsevier; 2015. p. 1–75.
Byrne HK, Wilmore JH. The effects of a 20-week exercise training program on resting metabolic rate in previously sedentary, moderately obese women. Int J Sport Nutr Exerc Metab. 2001;11:15–31.
Hunter GR, Byrne NM, Gower BA, Sirikul B, Hills AP. Increased resting energy expenditure after 40 min of aerobic but not resistance exercise. Obesity. 2006;14:2018–25.
Müller MJ, Enderle J, Bosy-Westphal A. Changes in energy expenditure with weight gain and weight loss in humans. Curr Obes Rep. 2016;5:413–23.
Thorp AA, Schlaich MP. Relevance of sympathetic nervous system activation in obesity and metabolic syndrome. J Diabetes Res. 2015, 341583.
Gentile CL, Orr JS, Davy BM, Davy KP. Modest weight gain is associated with sympathetic neural activation in nonobese humans. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1834–R8.
Cleeman JI. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Dalleck LC, Allen BA, Hanson BA, Borresen EC, Erickson ME, De Lap SL. Dose-response relationship between moderate-intensity exercise duration and coronary heart disease risk factors in postmenopausal women. J Women’s Health. 2009;18:105–13.
Wooten JS, Phillips MD, Mitchell JB, Patrizi R, Pleasant RN, Hein RM, et al. Resistance exercise and lipoproteins in postmenopausal women. Int J Sports Med. 2011;32:7–13.
Acknowledgements
The authors would like to thank Beytepe Gün Hospital for their contributions and support. We acknowledge the Hacettepe University Scientific Research Projects Coordination Unit for funding this study (Project ID: THD-2016-7280).
Funding
This study was funded by a grant from the Hacettepe University Scientific Research Projects Coordination Unit (Project ID: THD-2016-7280).
Author information
Authors and Affiliations
Contributions
YG, MMA, HHT, and ŞNK designed the study. YG and MMA collected and analyzed the data, and wrote the manuscript; HHT contributed to the interpretation of the results, constructing the methods, and reviewing the data analyses; ŞNK contributed to the development of the study idea, data collection, data analysis, and manuscript preparation. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Hacettepe University Non-Interventional Clinical Research Ethics Board (GO: 15/197-33) and written informed consent was obtained from the participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Güzel, Y., Atakan, M.M., Turnagöl, H.H. et al. Effects of 10 weeks of walking-based exercise training on resting substrate oxidation in postmenopausal women with obesity. Eur J Clin Nutr 79, 311–319 (2025). https://doi.org/10.1038/s41430-024-01546-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-024-01546-1