Abstract
Background
The Royal College of Physicians (RCP) and Thyroid Eye Disease Amsterdam Declaration Implementation Group (TEAMeD-5) have the common goal of improving access to high quality care for thyroid eye disease (TED). The TEAMeD-5 programme recommends all patients with moderate-to-severe TED should have access to multidisciplinary clinics (MDT) with combined Ophthalmology and Endocrinology expertise.
Methods
The British Oculoplastic Surgery Society represents oculoplastic surgeons who usually lead TED care in the UK. A two-stage survey of the membership was conducted to ascertain current practice of existing resources.
Results
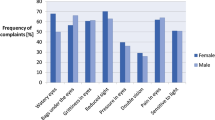
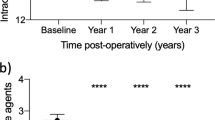
Seventy percent (45/65) of respondents in Survey 1 were aware of current RCP guidance, but only 49% (22/45) rated it as a good means of improving access to comprehensive TED service. Sixty percent (39/65) of respondents are working in a multidisciplinary TED clinic with co-___location of ophthalmologists and endocrinologists. Care for TED appears not to be provided in a multidisciplinary context in up to 31% (20/65). Thirty five (54%) of the respondents rated their relationship with endocrinology colleagues as good. Best practice guidelines recommend routine quality of life assessments but only 6/28 (21%) of respondents use this modality in current practice. Six percent (4/65) of areas appear not to be using intravenous steroids. In many areas (25%, 16/65), second-line immunosuppression is provided in a different trust and in 8% (5/65), it appears not to be used at all.
Conclusion
This survey is a ‘snapshot’ of current TED management in the UK and findings suggest scope for improvement. We recommend a framework for more robust collaboration across specialties and propose standards endorsed by multidisciplinary stakeholder societies.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Abraham-Nordling M, Byström K, Törring O, Lantz M, Berg G, Calissendorff J, et al. Incidence of hyperthyroidism in Sweden. Eur J Endocrinol. 2011;165:899–905.
Perros P, Hegedus L, Bartalena L, Marcocci C, Kahaly GJ, Baldeschi L, et al. Graves’ orbitopathy as a rare disease in Europe: a European Group on Graves’ Orbitopathy (EUGOGO) position statement. Orphanet J Rare Dis. 2017;12:72.
Ponto KA, Merkesdal S, Hommel G, Pitz S, Pfeiffer N, Kahaly GJ. Public health relevance of Graves’ orbitopathy. J Clin Endocrinol Metab. 2013;98:145–52.
Park JJ, Sullivan TJ, Mortimer RH, Wagenaar M, Perry-Keene DA. Assessing quality of life in Australian patients with Graves’ ophthalmopathy. Br J Ophthalmol. 2004;88:75–8. http://www.ncbi.nlm.nih.gov/pubmed/14693779.
Marcocci C, Altea MA, Leo M. Treatment options for Graves’ orbitopathy. Expert Opin Pharmacother. 2012;13:795–806.
Perros P, Wiersinga WM. The Amsterdam Declaration on Graves’ orbitopathy. Thyroid. 2010;20:245–6.
Perros P, Dayan CM, Dickinson AJ, Ezra D, Estcourt S, Foley P, et al. Management of patients with Graves’ orbitopathy: initial assessment, management outside specialised centres and referral pathways. Clin Med. 2015;15:173–8.
Bartalena L, Baldeschi L, Dickinson A, Eckstein A, Kendall-Taylor P, Marcocci C, et al. Consensus statement of the European Group on Graves’ orbitopathy (EUGOGO) on management of GO. Eur J Endocrinol. 2008;158:273–85.
Bartalena L, Baldeschi L, Boboridis K, Eckstein A, Kahaly GJ, Marcocci C, et al. The 2016 European Thyroid Association/European Group on Graves’ Orbitopathy Guidelines for the Management of Graves’ Orbitopathy. Eur Thyroid J. 2016;5:9–26.
Estcourt S, Hickey J, Perros P, Dayan C, Vaidya B. The patient experience of services for thyroid eye disease in the United Kingdom: results of a nationwide survey. Eur J Endocrinol. 2009;161:483–7.
Mellington FE, Dayan CM, Dickinson AJ, Hickey JL, MacEwen CJ, McLaren J, et al. Management of thyroid eye disease in the United Kingdom: a multi-centre thyroid eye disease audit. Orbit. 2017;36:159–69.
Perros P, Baldeschi L, Boboridis K, Dickinson AJ, Hullo A, Kahaly GJ, et al. A questionnaire survey on the management of Graves’ orbitopathy in Europe. Eur J Endocrinol. 2006;155:207–11.
Prummel MF, Bakker A, Wiersinga WM, Baldeschi L, Mourits MP, Kendall-Taylor P, et al. Multi-center study on the characteristics and treatment strategies of patients with Graves’ orbitopathy: the first European Group on Graves’ Orbitopathy experience. Eur J Endocrinol. 2003;148:491–5.
Perros P, Chandler T, Dayan CM, Dickinson AJ, Foley P, Hickey J, et al. Orbital decompression for Graves’ orbitopathy in England. Eye. 2012;26:434–7.
Draman MS, Mitchell A, Dayan C. TEAMeD-5: improving outcomes in thyoid eye disease | Society for Endocrinology. Endocrinologist. 2017;(125). https://www.endocrinology.org/endocrinologist/125-autumn17/features/teamed-5-improving-outcomes-in-thyoid-eye-disease/.
Benzimra JD, Quinn AG, Kersey T, McGrane D, Goss L, Vaidya B. Management of patients in a combined thyroid eye clinic in secondary care. Int Ophthalmol. 2014;34:1–6.
Avari C, Bravis V, Robinson S, Meeran K, Lee V. Sharing and caring? Perspectives of multidisciplinary working between endocrinologists and ophthalmologists in thyroid eye disease | Society for Endocrinology. Endocrinologist. 2018;(129). https://www.endocrinology.org/endocrinologist/129-autumn18/general-news/sharing-and-caring-perspectives-of-multidisciplinary-working-between-endocrinologists-and-ophthalmologists-in-thyroid-eye-disease/.
Ebner R, Devoto MH, Weil D, Bordaberry M, Mir C, Martinez H, et al. Treatment of thyroid associated ophthalmopathy with periocular injections of triamcinolone. Br J Ophthalmol. 2004;88:1380–6.
Young SM, Kim YD, Lang SS, Woo KI. Transconjunctival triamcinolone injection for upper lid retraction in thyroid eye disease-a new injection method. Ophthal Plast Reconstr Surg. 2018;34:587–93.
Rajendram R, Taylor PN, Wilson VJ, Harris N, Morris OC, Tomlinson M, et al. Combined immunosuppression and radiotherapy in thyroid eye disease (CIRTED): a multicentre, 2 × 2 factorial, double-blind, randomised controlled trial. Lancet Diabetes Endocrinol. 2018;6:299–309.
Kahaly GJ, Riedl M, Konig J, Pitz S, Ponto K, Diana T, et al. Mycophenolate plus methylprednisolone versus methylprednisolone alone in active, moderate-to-severe Graves’ orbitopathy (MINGO): a randomised, observer-masked, multicentre trial. Lancet Diabetes Endocrinol. 2018;6:287–98.
Baldeschi L, Wakelkamp IM, Lindeboom R, Prummel MF, Wiersinga WM. Early versus late orbital decompression in Graves’ orbitopathy: a retrospective study in 125 patients. Ophthalmology. 2006;113:874–8.
Mitchell AL, Goss L, Mathiopoulou L, Morris M, Vaidya B, Dickinson AJ, et al. Diagnosis of Graves’ orbitopathy (DiaGO): results of a pilot study to assess the utility of an office tool for practicing endocrinologists. J Clin Endocrinol Metab. 2015;100:E458–62.
Dolman PJ. Evaluating Graves’ orbitopathy. Best Pr Res Clin Endocrinol Metab. 2012;26:229–48.
Vannucchi G, Campi I, Covelli D, Dazzi D, Curro N, Simonetta S, et al. Graves’ orbitopathy activation after radioactive iodine therapy with and without steroid prophylaxis. J Clin Endocrinol Metab. 2009;94:3381–6.
Wickwar S, McBain HB, Ezra DG, Hirani SP, Rose GE, Newman SP. What are the psychosocial outcomes of treatment for thyroid eye disease? A systematic review. Thyroid. 2014;24:1407–18.
Estcourt S, Quinn AG, Vaidya B. Quality of life in thyroid eye disease: impact of quality of care. Eur J Endocrinol. 2011;164:649–55.
Wickwar S, McBain H, Ezra DG, Hirani SP, Rose GE, Newman SP. The psychosocial and clinical outcomes of orbital decompression surgery for thyroid eye disease and predictors of change in quality of life. Ophthalmology. 2015;122:2568–76.e1
The Royal College of Ophthalmologists. New Guidelines for Thyroid Eye Disease. 2015. https://www.rcophth.ac.uk/2015/07/new-guidelines-for-thyroid-eye-disease/.
Acknowledgements
The recommendations in this paper have been endorsed by TEAMeD, BOPSS, Royal College of Ophthalmologists, The Royal College of Physicians, Society for Endocrinology, British Thyroid Foundation and the British and Irish Orthoptic Society. The authors would like to thank the BOPSS Thyroid Audit Standards Group: Vikas Chadha, Lucy Clarke, Rebecca Ford, Anjana Haridas, Carole Jones (BOPSS president 2018), Faye Mellington, Rachna Murthy, Jonathan Norris, Cornelius Rene (BOPSS president 2016–2018), Sachin Salvi, Jimmy Uddin, Colin Vize (BOPSS secretary) and Stephen White and the BOPSS membership for completing the surveys. The authors also thank Janis Hickey (British Thyroid Foundation) and Lorna Pankethman (British and Irish Orthoptic Society) for their support and recommendations. The authors would like to thank TEDct for their generous donation that made it possible for this paper to be open access.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
Ben Williams is the Webmaster for BOPSS and is renumerated for providing IT support. None of the other authors or contributors have any conflict of interest to declare.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lee, V., Avari, P., Williams, B. et al. A survey of current practices by the British Oculoplastic Surgery Society (BOPSS) and recommendations for delivering a sustainable multidisciplinary approach to thyroid eye disease in the United Kingdom. Eye 34, 1662–1671 (2020). https://doi.org/10.1038/s41433-019-0664-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0664-z