Abstract
Purpose
To assess the physiological changes in the cornea over time in patients with irregular cornea fitted with Rose K2 XL gas-permeable scleral contact lenses.
Methods
Prospective study of 16 eyes of patients who did not tolerate gas-permeable corneal contact lenses and were fitted with Rose K2 XL scleral lenses. We assessed the central vault and the corneal thickness centrally and at peripheral regions (2 to 5 mm annulus). All these measures were obtained by anterior segment optical coherence tomography. The measurements were taken immediately after fitting the lenses and 1, 6 and 12 months later. Prior to the study and at 1 year, we performed an objective test for diagnosing limbal stem cell deficiency (Limbokit).
Results
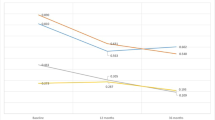
The mean vault was 201.7 ± 82.3 µm 20 min after fitting the contact lens; 189.4 ± 94.0 µm at 1 month; 165.1 ± 75.9 µm at 6 months and 142.1 ± 76.8 µm at 1 year, the values at 6 and 12 months being significantly different to baseline. After 1 year, the central corneal thickness had increased by 2.3% (IQR = 5.6), but the changes were only significant for the superior thickness. There is no limbal stem cell deficiency after 1 year of scleral contact lens use.
Conclusions
After use of Rose K2 XL scleral contact lenses, the corneal physiology of patients with an irregular cornea remains unchanged, as assessed by corneal thickness measurements and the Limbokit test. In all cases, however, the vault decreased over time.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Bennett EB. GP annual report 2016. Contact Lens Spectr. 2016;31:24–31.
Visser E-S, Van der Linden BJ, Otten HM, Van der Lelij A, Visser R. Medical applications and outcomes of bitangential scleral lenses. Optom Vis Sci. 2013;90:1078–85.
Romero-Jiménez M, Flores-Rodríguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013;36:146–50.
Lee JC, Chiu GB, Bach D, Babadeygy SR, Irvine J, Heur M. Functional and visual improvement with prosthetic replacement of the ocular surface ecosystem scleral lenses for irregular corneas. Cornea. 2013;32:1540–3.
Alipour F, Kheirkhah A, Jabarvand BM. Use of mini scleral contact lenses in moderate to severe dry eye. Cont Lens Anterior Eye. 2012;35:272–6.
Kalwerisky K, Davies B, Mihora L, Czyz CN, Foster JA, DeMartelaere S. Use of the Boston Ocular Surface Prosthesis in the management of severe periorbital thermal injuries: a case series of 10 patients. Ophthalmology. 2012;119:516–21.
Shah-Desai SD, Aslam Sa, Pullum K, Beaconsfield M, Rose GE. Scleral contact lens usage in patients with complex blepharoptosis. Ophthal Plast Reconstr Surg. 2011;27:95–8.
Severinsky B, Behrman S, Frucht-Pery J, Solomon A. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Contact Lens Anterior Eye. 2014;37:196–202.
Barnett M, Lien V, Li JY, Mannis MJ, Durbin-Johnson B. Use of scleral lenses and miniscleral lenses after penetrating keratoplasty. Eye Contact Lens Sci Clin Pr. 2016;42:185–9.
Kramer EG, Boshnick EL. Scleral lenses in the treatment of post-LASIK ectasia and superficial neovascularization of intrastromal corneal ring segments. Contact Lens Anterior Eye. 2015;38:298–303.
Schornack MM. Limbal stem cell disease: management with scleral lenses. Clin Exp Optom. 2011;94:592–4.
Tougeron-Brousseau B, Delcampe A, Gueudry J, Vera L. Doan S, Hoang-Xuan T et al. Vision-related function after scleral lens fitting in ocular complications of Stevens-Johnson syndrome and toxic epidermal necrolysis. Am J Ophthalmol. 2009;148:852–859.e2.
Deloss KS, Fatteh NH, Hood CT. Prosthetic replacement of the ocular surface ecosystem (PROSE) scleral device compared to keratoplasty for the treatment of corneal ectasia. Am J Ophthalmol. 2014;158:974–82.
Schornack MM. Scleral lenses. Eye Contact Lens Sci Clin Pr. 2015;41:3–11.
Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;35:266–71.
Compañ V, Oliveira C, Aguilella-Arzo M, Mollá S, Peixoto-de-Matos SC, Gónzalez-Méojome JM. Oxygen diffusion and edema with modern scleral rigid gas permeable contact lenses. Invest Ophthalmol Vis Sci. 2014;55:6421–9.
Giasson CJ, Morency J, Melillo M, Michaud L. Oxygen tension beneath scleral lenses of different clearances. Optom Vis Sci. 2017;94:466–75.
Soeters N, Visser ES, Imhof SM, Tahzib NG. Scleral lens influence on corneal curvature and pachymetry in keratoconus patients. Contact Lens Anterior Eye. 2015;38:294–7.
Vincent SJ, Alonso-caneiro D, Collins MJ, Beanland A, Lam L. Hypoxic corneal changes following eight hours of scleral contact lens wear. Optom Vis Sci. 2016;93:293–9.
Smith GT, Mireskandari K, Pullum KW. Corneal swelling with overnight wear of scleral contact lenses. Cornea 2004;23:29–34.
Kauffman MJ, Gilmartin Ca, Bennett ES, Bassi CJ. A comparison of the short-term settling of three scleral lens designs. Optom Vis Sci. 2014;91:1462–6.
Calonge M, Duebold Y, Sáez V, Enriquez de Salamanca A, García-Vázuqez C, Corrales RM. et al. Impression cytology of the ocular surface: a review. Exp Eye Res. 2004;78:457–72.
Rivas L, Oroza MA, Perez E, Murube del Castillo J. Topographical distribution of ocular surface cells by the use of impression cytology. Acta Ophthalmol. 1991;69:371–6.
Garcia I, Etxebarria J, Boto-de-Los-Bueis A, Díaz-Valle D, Rivas L, Martínez-Soroa I. et al. Comparative study of limbal stem cell deficiency diagnosis methods: detection of MUC5AC mRNA and goblet cells in corneal epithelium. Ophthalmology 2012;119:923–9.
García I, Etxebarria J, Merayo-Lloves J, Torras J, Boto-de-los-Bueis A, Díaz-Valle D et al. Novel molecular diagnostic system of limbal stem cell deficiency based on MUC5AC transcript detection in corneal epithelium by PCR-reverse dot blot. Investig Ophthalmol Vis Sci. 2013;54:5643–52.
Li Y, Tang M, Zhang X, Salaroli CH, Ramos JL, Huang D. Pachymetric mapping with Fourier-___domain optical coherence tomography. J Cataract Refract Surg. 2010;36:826–31.
Wang Q, Hua Y, Savini G, Chen H, Bao F, Lin S et al. Corneal power measurement obtained by fourier-___domain reproducibility, and comparison with scheimpflug and automated keratometry measurements. Cornea. 2015;34:1266–71.
Bayhan HA, Aslan Bayhan S, Can I. Comparison of central corneal thickness measurements with three new optical devices and a standard ultrasonic pachymeter. Int J Ophthalmol. 2014;7:302–8.
Wang C, Xia X, Tian B, Zhou S. Comparison of fourier-___domain and time-___domain optical coherence tomography in the measurement of thinnest corneal thickness in Keratoconus. J Ophthalmol 2015;2015:1–7.
de Luis Eguileor B, Etxebarria Ecenarro J, Santamaria Carro A, Feijoo Lera R. Irregular corneas. Eye Contact Lens Sci Clin Pr. 2016;0:1.
Alipour F, Jabarvand Behrouz M, Samet B. Mini-scleral lenses in the visual rehabilitation of patients after penetrating keratoplasty and deep lamellar anterior keratoplasty. Contact Lens Anterior Eye. 2015;38:54–8.
Kornberg DL, Dou E, Wang Y, St Clair R, Lee MN, Sood P et al. Clinical experience with PROSE fitting: significance of diagnosis and age. Eye Contact Lens. 2016;42:124–8.
Mishima S. Corneal thickness. Surv Ophthalmol 1968;13:57–96.
Mertz GW. Overnight swelling of the living human cornea. J Am Optom Assoc. 1980;51:211–4.
Harper CL, Boulton ME, Bennett D, Marcyniuk B, Jarvis-Evans JH, Tullo AB et al. Diurnal variations in human corneal thickness. Br J Opthalmol. 1996;80:1068–72.
McAlinden C, Khadka J, Pesudovs K. A comprehensive evaluation of the precision (repeatability and reproducibility) of the oculus pentacam HR. Investig Ophthalmol Vis Sci. 2011;52:7731–7.
Funding
This study was funded by a Jesús de Gangoiti Barrera grant with no links between the researchers who conducted the work and the companies that supplied the materials used.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
de Luis Eguileor, B., Acera, A., Santamaría Carro, A. et al. Changes in the corneal thickness and limbus after 1 year of scleral contact lens use. Eye 34, 1654–1661 (2020). https://doi.org/10.1038/s41433-019-0729-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0729-z