Abstract
Objectives
To establish the norms of binocular and monocular acuity and interocular acuity differences for southern Chinese infants and compare these norms with the results for northern Chinese infants.
Methods
A prospective, comparative, and noninterventional study was conducted from January to August 2018. Teller Acuity Cards II were used to determine the binocular and monocular acuity of infants. The tolerance intervals and limits with a stated proportion and probability were used to evaluate the norms of binocular and monocular acuity and interocular acuity differences. An unpaired t-test was used to compare the obtained norms with the reported northern Chinese norms.
Results
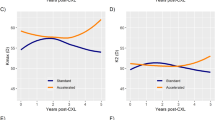
The tolerance intervals of binocular acuity (mean acuity of 3.73, 7.35, and 12.01 cpd, respectively, at 12, 24, and 36 months), monocular acuity (mean acuity of 2.88, 6.91, and 10.75 cpd, respectively, at 12, 24, and 36 months), and interocular acuity differences (mean difference of 0.92, 2.89, and 3.99 cpd, respectively, at 12, 24, and 36 months) were obtained, exhibiting an increasing trend with age. The binocular visual acuity norms of southern Chinese infants were significantly lower than those in northern China (4.37 vs. 6.9 cpd at 8 months and 7.35 vs. 26 cpd at 24 months) (P = 0.011).
Conclusions
Northern and southern Chinese infants exhibited distinct acuity norms and visual development patterns. The establishment of population-specific visual acuity norms is necessary for current populations of infants from different regions.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Roizen N, Kasza K, Karrison T, Mets M, Noble AG, Boyer K, et al. Impact of visual impairment on measures of cognitive function for children with congenital toxoplasmosis: implications for compensatory intervention strategies. Pediatrics. 2006;118:e379–390.
Brémond-Gignac D, Copin H, Lapillonne A, Milazzo S. Visual development in infants: physiological and pathological mechanisms. Curr Opin Ophthalmol. 2011;22:S1–8.
Dallaire R, Muckle G, Rouget F, Kadhel P, Bataille H, Guldner L, et al. Cognitive, visual, and motor development of 7-month-old Guadeloupean infants exposed to chlordecone. Environ Res. 2012;118:79–85.
Elyashiv SM, Shabtai EL, Belkin M. Correlation between visual acuity and cognitive functions. Br J Ophthalmol. 2014;98:129–32.
Jacobson SG, Mohindra I, Held R. Development of visual acuity in infants with congenital cataracts. Br J Ophthalmol. 1981;65:727–35.
Wiesel TN. Postnatal development of the visual cortex and the influence of environment. Nature. 1982;299:583–91.
Lewis TL, Maurer D, Brent HP. Effects on perceptual development of visual deprivation during infancy. Br J Ophthalmol. 1986;70:214–20.
Sener EC, Mocan MC, Gedik S, Ergin A, Sanaç AS. The reliability of grading the fixation preference test for the assessment of interocular visual acuity differences in patients with strabismus. J AAPOS. 2002;6:191–4.
Lewis TL, Maurer D. Effects of early pattern deprivation on visual development. Optom Vis Sci. 2009;86:640–6.
Livingstone IA, Lok AS, Tarbert C. New mobile technologies and visual acuity. Conf Proc IEEE Eng Med Biol Soc. 2014;2014:2189–92.
Mayer DL, Beiser AS, Warner AF, Pratt EM, Raye KN, Lang JM. Monocular acuity norms for the Teller Acuity Cards between ages one month and four years. Invest Ophthalmol Vis Sci. 1995;36:671–85.
Salomão SR, Ventura DF. Large sample population age norms for visual acuities obtained with Vistech-Teller Acuity Cards. Invest Ophthalmol Vis Sci. 1995;36:657–70.
Fantz RL. Pattern vision in young infants. Psychological Rec. 1958;8:43–47.
McDonald MA, Dobson V, Sebris SL, Baitch L, Varner D, Teller DY. The acuity card procedure: a rapid test of infant acuity. Invest Ophthalmol Vis Sci. 1985;26:1158–62.
Teller DY, McDonald MA, Preston K, Sebris SL, Dobson V. Assessment of visual acuity in infants and children: the acuity card procedure. Dev Med Child Neurol. 1986;28:779–89.
Brown AM, Yamamoto M. Visual acuity in newborn and preterm infants measured with grating acuity cards. Am J Ophthalmol. 1986;102:245–53.
McDonald M, Ankrum C, Preston K, Sebris SL, Dobson V. Monocular and binocular acuity estimation in 18- to 36-month-olds: acuity card results. Am J Optom Physiol Opt. 1986;63:181–6.
McDonald M, Sebris SL, Mohn G, Teller DY, Dobson V. Monocular acuity in normal infants: the acuity card procedure. Am J Optom Physiol Opt. 1986;63:127–34.
Van Hof-van Duin J, Mohn G. The development of visual acuity in normal fullterm and preterm infants. Vis Res. 1986;26:909–16.
Dobson V, Schwartz TL, Sandstrom DJ, Michel L. Binocular visual acuity of neonates: the acuity card procedure. Dev Med Child Neurol. 1987;29:199–206.
Kohl P, Samek M. Refractive error and preferential looking visual acuity in infants 12-24 months of age: year 2 of a longitudinal study. J Am Optom Assoc. 1988;59:686–90.
Courage ML, Adams RJ. Visual acuity assessment from birth to three years using the acuity card procedure: cross-sectional and longitudinal samples. Optom Vis Sci. 1990;67:713–8.
Clifford CE, Haynes BM, Dobson V. Are norms based on the original Teller Acuity Cards appropriate for use with the new Teller Acuity Cards II. J AAPOS. 2005;9:475–9.
National Bureau of Statistics of China. Birth rate, death rate, and natural growth rate of population. http://data.stats.gov.cn/.
Kujansuu E, Kivinen S, Tuimala R. Pregnancy and delivery at the age of forty and over. Int J Gynaecol Obstet. 1981;19:341–5.
Ellegren H. Characteristics, causes and evolutionary consequences of male-biased mutation. Proc Biol Sci. 2007;274:1–10.
Sartorius GA, Nieschlag E. Paternal age and reproduction. Hum Reprod Update. 2010;16:65–79.
Qiu Y, Li XQ, Yan XM. Evaluation of grating visual acuity development in normal infants. Zhonghua Yan Ke Za Zhi. 2011;47:995–1000.
Teller DY, Dobson V, Mayer DL. Teller Acuity Cards™ II Handbook. Revised Edition. (University of Washington, 2005).
Dixon WJ, Massey FJ. Introduction to statistical analysis. 2nd ed. New York: McGraw-Hill; 1957.
Gordon RA, Donzis PB. Refractive development of the human eye. Arch Ophthalmol. 1985;103:785–9.
Hussain RN, Shahid F, Woodruff G. Axial length in apparently normal pediatric eyes. Eur J Ophthalmol. 2014;24:120–3.
Birch EE. Infant interocular acuity differences and binocular vision. Vis Res. 1985;25:571–6.
Salomão SR, Ejzenbaum F, Berezovsky A, Sacai PY, Pereira JM. Age norms for monocular grating acuity measured by sweep-VEP in the first three years of age. Arq Bras Oftalmol. 2008;71:475–9.
Costa MF, de Cássia Rodrigues Matos França V, Barboni M, Ventura DF. Maturation of binocular, monocular grating acuity and of the visual interocular difference in the first 2 years of life. Clin EEG Neurosci. 2018;49:159–70.
Atkinson J, Braddick O, Pimm-Smith E. ‘Preferential looking’ for monocular and binocular acuity testing of infants. Br J Ophthalmol. 1982. 66:264–8.
Leone JF, Mitchell P, Kifley A, Rose KA, Sydney childhood eye Studies. Normative. visual acuity in infants and preschool-aged children in Sydney. Acta Ophthalmol. 2014;92:e521–9.
He M, Zeng J, Liu Y, Xu J, Pokharel GP, Ellwein LB. Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci. 2004;45:793–9.
He M, Zheng Y, Xiang F. Prevalence of myopia in urban and rural children in mainland China. Optom Vis Sci. 2009;86:40–44.
You QS, Xu L, Yang H, Wang YX, Jonas JB. Five-year incidence of visual impairment and blindness in adult Chinese the Beijing Eye Study. Ophthalmology. 2011;118:1069–75.
Wang L, Huang W, He M, Zheng Y, Huang S, Liu B, et al. Causes and five-year incidence of blindness and visual impairment in urban Southern China: the Liwan Eye Study. Invest Ophthalmol Vis Sci. 2013;54:4117–21.
Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD, Ellwein LB. Refractive error study in children: results from Shunyi District, China. Am J Ophthalmol. 2000;129:427–35.
Acknowledgements
The authors are grateful to all participants for supporting our study.
Funding
This study was funded by grants from the National Natural Science Foundation of China (91546101), the Guangdong Provincial Natural Science Foundation for Distinguished Young Scholars of China (2014A030306030), and the Outstanding Young Teacher Cultivation Projects in Guangdong Province (YQ2015006). The sponsors of the study played no role in the study protocol design; data collection, analysis, or interpretation; manuscript preparation; or the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Xiang, Y., Long, E., Liu, Z. et al. Study to establish visual acuity norms with Teller Acuity Cards II for infants from southern China. Eye 35, 2787–2792 (2021). https://doi.org/10.1038/s41433-020-01314-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01314-y