Abstract
Objective
To evaluate visual acuity (VA) and factors influencing VA using new multimodal imaging-based classification of central serous chorioretinopathy (CSCR).
Methods
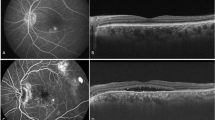
Retrospective, observational and cross-sectional study on 229 naïve eyes diagnosed as CSCR with available baseline data and multimodal imaging. Each case was classified into (i) simple/complex/atypical; (ii) primary/recurrent/resolved; (iii) persistent or not; (iv) outer retinal atrophy(ORA) present/absent; (v) foveal involvement present/absent; and (vi) macular neovascularization(MNV) present/absent. Best corrected visual acuity (BCVA) was correlated to the classification as well as every parameter of the classification.
Results
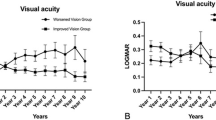
Median BCVA was 0.18 logMAR [95% Confidence Interval (CI)0.16–0.18] with median duration of complaints of one month (95% CI,6.14–13.0 months). Age of the patient (r = −0.24, p = 0.002) and duration of the disease (r = −0.32, p < 0.001) correlated significantly with BCVA. Logistic regression model showed that older age [odds ratio (OR) = 0.96, p = 0.05], female gender (OR = 2.45, p = 0.046), presence of ORA(OR = 0.34, p = 0.012),and foveal involvement(OR = 0.18, p = 0.007) were statistically significantly associated with poorer BCVA. Eyes classified as complex, persistent CSCR, with ORA or foveal involvement demonstrated lower BCVA compared to those with simple, non-persistent CSCR, without ORA or without foveal involvement (p < 0.05). Eyes with complex CSCR (p < 0.001), atypical CSCR(p = 0.025), persistent subretinal fluid (SRF) (p = 0.001) and those with ORA (p < 0.001) demonstrated a trend towards severe visual loss. Prevalence of persistent SRF, recurrent episodes and ORA was significantly higher among eyes with complex CSCR (p < 0.001) while there was no difference in prevalence of resolved cases (p = 0.07), foveal involvement (p = 0.28) and MNV (p = 0.45) between simple and complex cases.
Conclusion
There is a strong correlation between VA and foveal involvement and ORA using the new classification. Thus, the objective parameters of the classification can be incorporated in establishing the treatment guidelines for CSCR.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
08 November 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41433-021-01837-y
References
Kaye R, Chandra S, Sheth J, Boon CJF, Sivaprasad S, Lotery A. Central serous chorioretinopathy: An update on risk factors, pathophysiology and imaging modalities. Prog Retin Eye Res. 2020:100865.
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, et al. Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res. 2015;48:82–118.
Singh SR, Matet A, van Dijk EHC, Daruich A, Fauser S, Yzer S, et al. Discrepancy in current central serous chorioretinopathy classification. Br J Ophthalmol. 2019;103:737–42.
van Rijssen TJ, van Dijk EHC, Yzer S, Ohno-Matsui K, Keunen JEE, Schlingemann RO, et al. Central serous chorioretinopathy: towards an evidence-based treatment guideline. Prog Retin Eye Res. 2019;73:100770.
Chhablani J, Cohen FB. Multimodal imaging-based central serous chorioretinopathy classification. Ophthalmol Retin. 2020;4:1043–6.
Loo RH, Scott IU, Flynn HW Jr, Gass JD, Murray TG, Lewis ML, et al. Factors associated with reduced visual acuity during long-term follow-up of patients with idiopathic central serous chorioretinopathy. Retina 2002;22:19–24.
Aggio FB, Roisman L, Melo GB, Lavinsky D, Cardillo JA, Farah ME. Clinical factors related to visual outcome in central serous chorioretinopathy. Retina 2010;30:1128–34.
Mrejen S, Balaratnasingam C, Kaden TR, Bottini A, Dansingani K, Bhavsar KV, et al. Long-term visual outcomes and causes of vision loss in chronic central serous chorioretinopathy. Ophthalmology 2019;126:576–88.
Suwal B, Khadka D, Shrestha A, Shrestha S, Shrestha N, Khatri B. Baseline predictive factors of visual outcome and persistence of subretinal fluid based on morphologic changes in spectral ___domain optical coherence tomography in patients with idiopathic central serous chorioretinopathy. Clin Ophthalmol. 2019;13:2439–44.
Singh SR, Iovino C, Zur D, Masarwa D, Iglicki M, Gujar R, et al. Central serous chorioretinopathy imaging biomarkers. Br J Ophthalmol. 2020.
Matsumoto H, Sato T, Kishi S. Outer nuclear layer thickness at the fovea determines visual outcomes in resolved central serous chorioretinopathy. Am J Ophthalmol. 2009;148:105–10.e1.
Imamura Y, Fujiwara T, Spaide RF. Fundus autofluorescence and visual acuity in central serous chorioretinopathy. Ophthalmology 2011;118:700–5.
Mohabati D, van Rijssen TJ, van Dijk EH, Luyten GP, Missotten TO, Hoyng CB, et al. Clinical characteristics and long-term visual outcome of severe phenotypes of chronic central serous chorioretinopathy. Clin Ophthalmol. 2018;12:1061–70.
Nicholson BP, Ali Idris AM, Bakri SJ. Central Serous Chorioretinopathy: Clinical Characteristics Associated with Visual Outcomes. Semin Ophthalmol. 2018;33:804–7.
Spaide RF, Campeas L, Haas A, Yannuzzi LA, Fisher YL, Guyer DR, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology 1996;103:2070–9. discussion 9-80
Piccolino FC, de la Longrais RR, Ravera G, Eandi CM, Ventre L, Abdollahi A, et al. The foveal photoreceptor layer and visual acuity loss in central serous chorioretinopathy. Am J Ophthalmol. 2005;139:87–99.
Yalcinbayir O, Gelisken O, Akova-Budak B, Ozkaya G, Gorkem Cevik S, Yucel AA. Correlation of spectral ___domain optical coherence tomography findings and visual acuity in central serous chorioretinopathy. Retina 2014;34:705–12.
Gilbert CM, Owens SL, Smith PD, Fine SL. Long-term follow-up of central serous chorioretinopathy. Br J Ophthalmol. 1984;68:815–20.
Yannuzzi LA, Shakin JL, Fisher YL, Altomonte MA. Peripheral retinal detachments and retinal pigment epithelial atrophic tracts secondary to central serous pigment epitheliopathy. Ophthalmology 1984;91:1554–72.
Han J, Cho NS, Kim K, Kim ES, Kim DG, Kim JM, et al. Fundus autofluorescence patterns in central serous chorioretinopathy. Retina 2020;40:1387–94.
Borrelli E, Battista M, Sacconi R, Gelormini F, Querques L, Grosso D, et al. OCT risk factors for 3-year development of macular complications in eyes with “resolved” chronic central serous chorioretinopathy. Am J Ophthalmol. 2021;223:129–39.
Siedlecki J, Fischer C, Schworm B, Kreutzer TC, Luft N, Kortuem KU, et al. Impact of sub-retinal fluid on the long-term incidence of macular atrophy in neovascular age-related macular degeneration under treat & extend anti-vascular endothelial growth factor inhibitors. Sci Rep. 2020;10:8036.
Gianniou C, Dirani A, Jang L, Mantel I. Refractory intraretinal or subretinal fluid in neovascular age-related macular degeneration treated with intravitreal ranizubimab: functional and structural outcome. Retina 2015;35:1195–201.
Govindahari V, Singh SR, Rajesh B, Gallego-Pinazo R, Marco RD, Nair DV, et al. Multicolor imaging in central serous chorioretinopathy - a quantitative and qualitative comparison with fundus autofluorescence. Sci Rep. 2019;9:11728.
Bousquet E, Bonnin S, Mrejen S, Krivosic V, Tadayoni R, Gaudric A. Optical coherence tomography angiography of flat irregular pigment epithelium detachment in chronic central serous chorioretinopathy. Retina 2018;38:629–38.
Bonini Filho MA, de Carlo TE, Ferrara D, Adhi M, Baumal CR, Witkin AJ, et al. Association of choroidal neovascularization and central serous chorioretinopathy with optical coherence tomography angiography. JAMA Ophthalmol. 2015;133:899–906.
Quaranta-El Maftouhi M, El Maftouhi A, Eandi CM. Chronic central serous chorioretinopathy imaged by optical coherence tomographic angiography. Am J Ophthalmol. 2015;160:581–7.e1.
Dansingani KK, Balaratnasingam C, Klufas MA, Sarraf D, Freund KB. Optical coherence tomography angiography of shallow irregular pigment epithelial detachments in pachychoroid spectrum disease. Am J Ophthalmol. 2015;160:1243–54.e2.
Arora S, Kulikov AN, Maltsev DS. Implementation of the new multimodal imaging-based classification of central serous chorioretinopathy. Eur J Ophthalmol. 2021:11206721211013651.
Funding
No grants/ support was received for this study.
Author information
Authors and Affiliations
Contributions
SA contributed to concept and design of the work, analysis and interpretation of the data, writing the draft, revising it and finally approving it. DM contributed to acquisition of the data, analysis and interpretation of the data, writing the draft and approving it. NS contributed to acquisition of the data and its analysis, revising the draft and approving it. DP contributed to acquisition of the data and its analysis, revising the draft and approving it. CI contributed to acquisition of the data and its analysis and approving the final draft. TA contributed in analysis and interpretation of the data, writing the draft and approving it. AK helped in acquisition of the data and approving the final draft. FT was responsible for acquisition of the data and approving the final draft. RV contributed to acquisition of the data and approving the final draft. NR contributed to acquisition of the data and approving the final draft. RP contributed to acquisition of the data and approving the final draft. SS contributed to acquisition of the data and approving the final draft. EP contributed to acquisition of the data and approving the final draft. JC designed and conceptualized the study, was responsible for acquisition of the data, analysis and interpretation of the data, writing the manuscript, revising it and finally approving it. Supplementary information is available at Eye’s website.
Corresponding author
Ethics declarations
Financial disclosures
Dr Jay Chhablani is a consultant for Allergan, OD-OS, Novartis and Biogen. The remaining authors have no proprietary or financial interest in any aspect of this report. No grants/ support was received for this study.
Competing interests
Dr Jay Chhablani is a consultant for Allergan, OD-OS, Novartis and Biogen. The remaining authors have no proprietary or financial interest in any aspect of this report. There is no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The name of the author Ramesh Venkatesh was corrected.
Rights and permissions
About this article
Cite this article
Arora, S., Maltsev, D.S., Sahoo, N.K. et al. Visual acuity correlates with multimodal imaging-based categories of central serous chorioretinopathy. Eye 36, 517–523 (2022). https://doi.org/10.1038/s41433-021-01788-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01788-4
This article is cited by
-
Three-dimensional choroidal characteristics in different subtypes of central serous chorioretinopathy using swept-source optical coherence tomography angiography
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)
-
Gender differences in central serous chorioretinopathy based on the new multimodal imaging classification
Eye (2024)
-
Randomized controlled trials in central serous chorioretinopathy: A review
Eye (2023)
-
Early versus delayed photodynamic therapy for chronic central serous chorioretinopathy
International Ophthalmology (2023)
-
577 nm subthreshold micropulse laser treatment for acute central serous chorioretinopathy: a comparative study
BMC Ophthalmology (2022)