Abstract
Background
To evaluate the influence of age on the clinical characteristics of primary rhegmatogenous retinal detachments (RRD).
Methods
We conducted a retrospective review of a prospectively collected dataset. Data regarding adult patients (aged 16–100 years) who had undergone primary RRD repair, were extracted from two online databases. Baseline demographics, preoperative clinical characteristics and surgical management details were collected. Age-based groups (16–30, 30–39, 40–49, 50–59, 60–69, 70–79, ≥80) were compared using univariate analysis, with multivariate testing for interaction of age with sex, laterality and pseudophakia.
Results
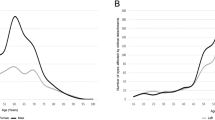
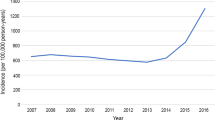
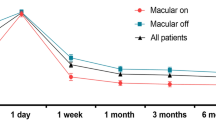
In total, 8,133 eyes were analysed, of which the majority (59%) were in the 50–69 age-range peaking at 60, with a male predominance (64%). Myopia was significantly more frequent in patients aged <50 years. The presence of posterior vitreous detachment increased up to 50 years, then remained >95%. Foveal involvement, grade C proliferative vitreoretinopathy, total RD and greater RD extent were more common and progressively increased after 60 years, with worsening visual acuity. Isolated superior RRDs became more prevalent with age reaching a plateau in the age-range 50–69, before reducing again; conversely, isolated inferior RRDs were commoner in those <30, with a minimum in the 70–79 age-range. The incidence of fellow-eye RRD decreased linearly with age.
Conclusions
Age appeared a key variable in RRD phenotype influencing a wide range of RRD characteristics. The higher incidence of myopia, PVD absent and bilateral RRD in patients <40 years and the significant phenotypical differences in the under 40 and over 50 age-groups highlight that there are several discrete forms of RRD.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
Data is freely available at https://outcomes.beavrs.org/ via ‘contact’ request and agreement to BEAVRS data access request guidelines
References
Qureshi MH, Steel DHW. Retinal detachment following cataract phacoemulsification-a review of the literature. Eye (Lond). 2020;34:616–31.
van Leeuwen R, Haarman AEG, van de Put MAJ, Klaver CCW, Los LI, Dutch Rhegmatogenous Retinal Detachment Study Group. Association of rhegmatogenous retinal detachment incidence with myopia prevalence in the Netherlands. JAMA Ophthalmol. 2021;139:85–92.
Nielsen BR, Alberti M, Bjerrum SS, la Cour M. The incidence of rhegmatogenous retinal detachment is increasing. Acta Ophthalmol. 2020;98:603–6.
Lewis H. Peripheral retinal degenerations and the risk of retinal detachment. Am J Ophthalmol. 2003;136:155–60.
Eye Disease Case-Control Study Group. Risk factors for idiopathic rhegmatogenous retinal detachment. Am J Epidemiol. 1993;137:749–57.
Chandra A, Banerjee P, Davis D, Charteris D. Ethnic variation in rhegmatogenous retinal detachments. Eye. 2015;29:803–7.
Mahroo OA, Dybowski R, Wong R, Williamson T. Characteristics of rhegmatogenous retinal detachment in pseudophakic and phakic eyes. Eye 2012;26:1114–21.
Ferrara M, Mehta A, Qureshi H, Avery P, Yorston D, Laidlaw DA, et al. Phenotype and outcomes of phakic versus pseudophakic primary rhegmatogenous retinal detachments: cataract or cataract surgery related? Am J Ophthalmol. 2020;222:318–27.
Mitry D, Charteris DG, Yorston D, Rehman Siddiqui MA, Campbell H, Murphy AL, et al. The epidemiology and socioeconomic associations of retinal detachment in Scotland: a two-year prospective population-based study. Invest Ophthalmol Vis Sci. 2010;51:4963–8.
Li X, Beijing Rhegmatogenous Retinal Detachment Study Group. Incidence and epidemiological characteristics of rhegmatogenous retinal detachment in Beijing, China. Ophthalmology. 2003;110:2413–7.
Li JQ, Welchowski T, Schmid M, Holz FG, Finger RP. Incidence of rhegmatogenous retinal detachment in Europe––a systematic review and meta-analysis. Ophthalmologica. 2019;242:81–6.
Van de Put MA, Hooymans JM, Los LI, Group DRRDS. The incidence of rhegmatogenous retinal detachment in The Netherlands. Ophthalmology. 2013;120:616–22.
Kim MS, Park SJ, Park KH, Woo SJ. Different mechanistic association of myopia with rhegmatogenous retinal detachment between young and elderly patients. BioMed Res Int. 2019;2019:5357241.
Sakamoto T, Kawano S, Kawasaki R, Hirakata A, Yamashita H, Yamamoto S, et al. Japan-Retinal Detachment Registry Report I: preoperative findings in eyes with primary retinal detachment. Jpn J Ophthalmol. 2020;64:1–12.
Patel SN, Starr MR, Obeid A, Ryan EH, Ryan C, Forbes NJ, et al. Characteristics and surgical outcomes of rhegmatogenous retinal detachment in older adults: a multicenter comparative cohort study. Retina. 2021;41:947–56.
Park SJ, Cho SC, Choi NK, Park KH, Woo SJ. Age, sex, and time-specific trends in surgical approaches for rhegmatogenous retinal detachment: a nationwide, population-based study using the National claim registry. Retina. 2017;37:2326–33.
Lieberman RM, Gow JA, Grillone LR. Development and implementation of a vitreous hemorrhage grading scale. Retin Physician. 2006;3:S1–S8.
Machemer R, Aaberg TM, Freeman HM, Irvine AR, Lean JS, Michels RM. An updated classification of retinal detachment with proliferative vitreoretinopathy. Am J Ophthalmol. 1991;112:159–65.
Lange C, Feltgen N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247:137–42.
Chen SN, Lian IeB, Wei YJ. Epidemiology and clinical characteristics of rhegmatogenous retinal detachment in Taiwan. Br J Ophthalmol. 2016;100:1216–20.
Park SJ, Choi NK, Park KH, Woo SJ. Five year nationwide incidence of rhegmatogenous retinal detachment requiring surgery in Korea. PLoS One. 2013;8:e80174.
Williams KM, Dogramaci M, Williamson TH. Retrospective study of rhegmatogenous retinal detachments secondary to round retinal holes. Eur J Ophthalmol. 2012;22:635–40.
Boutin TS, Charteris DG, Chandra A, Campbell S, Hayward C, Campbell A, et al. Insights into the genetic basis of retinal detachment. Hum Mol Genet. 2020;29:689–702.
Mitry D, Singh J, Yorston D, Siddiqui MA, Wright A, Fleck BW, et al. The predisposing pathology and clinical characteristics in the Scottish retinal detachment study. Ophthalmology. 2011;118:1429–34.
Aylward GW, Cooling RJ, Leaver PK. Trauma-induced retinal detachment associated with giant retinal tears. Retina. 1993;13:136–41.
Mehdizadeh M, Afarid M, Hagigi MS. Risk factors for giant retinal tears. J Ophthalmic Vis Res. 2010;5:246–9.
Kwong TQ, Shunmugam M, Williamson TH. Characteristics of rhegmatogenous retinal detachments secondary to retinal dialyses. Can J Ophthalmol. 2014;49:196–9.
Kinyoun JL, W H Knobloch WH. Idiopathic retinal dialysis. Retina. 1984;4:9–14.
Abdolrahimzadeh S, Piraino DC, Scavella V, Abdolrahimzadeh B, Crucian F, Gharbiya M, et al. Spectral ___domain optical coherence tomography and B-scan ultrasonography in the evaluation of retinal tears in acute, incomplete posterior vitreous detachment. BMC Ophthalmol. 2016;16:60.
Shunmugam M, Shah AN, Hysi PG, Williamson TH. The pattern and distribution of retinal breaks in eyes with rhegmatogenous retinal detachment. Am J Ophthalmol. 2014;157:221–226.
Chen C, Huang S, Sun L, Li S, Huang L, Wang Z, et al. Analysis of etiologic factors in pediatric rhegmatogenous retinal detachment with genetic testing. Am J Ophthalmol. 2020;218:330–6.
Acknowledgements
BEAVRS and Euretina VR Retinal Detachment outcomes group: Atiq Babar, Hull and East Yorkshire Eye Hospital, Hull, UK; Kamaljit Singh Balaggan, Wolverhampton and Midland Counties Eye Infirmary, New Cross Hospital, Wolverhampton, UK; Anthony G Casswell, Brighton and Sussex University Hospitals NHS Trust, Brighton, UK; Aman Chandra, Mid & South Essex NHS Foundation Trust, Southend, UK, Anglia Ruskin University, Cambridge, UK; Stephen Charles, Manchester Royal Eye Hospital, Manchester, UK; Timothy Cochrane, Maidstone and Tunbridge Wells NHS Trust, Tunbridge Wells, UK; Niels Crama, Radboudumc, Nijmegen, The Netherlands; Sandro Di Simplicio Cherubini, Newcastle Eye Centre, Royal Victoria Infirmary, Newcastle upon Tyne, UK; Abdallah A Ellabban, Hull University Teaching Hospitals, Hull, UK; John Ellis, Ninewells Hospital, Dundee, UK; Peter van Etten, Retina Operation Center Utrecht, Utrecht, The Netherlands; Marta S. Figueroa, Ramon y Cajal University Hospital, Madrid, Spain, Alcala de Henares University, Madrid, Spain; Craig Goldsmith, James Paget University Hospitals NHS Trust, Great Yarmouth UK; Roxane J Hillier, Newcastle Eye Centre, Royal Victoria Infirmary, Newcastle upon Tyne, UK; Edward Hughes, University Hospitals Sussex, Brighton, UK; Tsveta Ivanova, Manchester Royal Eye Hospital, Manchester, UK; Assad Jalil, Manchester Royal Eye Hospital, Manchester, UK; Huw Jenkins, Hywel Dda University Health Board, Carmarthenshire, UK; Ashraf Khan, Princess Alexandra Eye Pavilion, Edinburgh, UK; D Alistair Laidlaw, Guy’s and St. Thomas’ NHS Foundation Trust, London, UK; Yannick Le Mer, Hopital Fondation A. de Rothschild, Paris, France; Angelina Meireles, Centro Hospitalar Universitário do Porto, Porto, Spain; Andrew HC Morris, Royal Bournemouth Hospital, Bournemouth, UK; Richard Newsom, University of Portsmouth, Portsmouth, UK; Vasileios T Papastavrou, Cumberland Infirmary, Carlisle, UK; Jonathan C Park, Musgrove Park Hospital, Taunton, UK; Yashin D Ramkissoon, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK; Diego Sanchez-Chicharro, Martin University Hospital, Martin, Slovakia; Richard Sheard, Derwent Eye Specialists, Hobart, Tasmania; Jonathan Smith, Sunderland Eye Infirmary, Sunderland, UK; Kurt Spiteri Cornish, Sheffield Teaching hospitals NHS Trust, Sheffield, UK; David HW Steel, Sunderland Eye Infirmary, Sunderland, UK; Vaughan Tanner, King Edward VII Hospital, Windsor, UK; Deepak Vayalambrone, East Suffolk and North Essex NHS Foundation Trust, Essex, UK; Tom H Williamson, Guy’s and St. Thomas’ NHS Foundation Trust, London, UK; Stephen Winder, Royal Hallamshire Hospital, Sheffield; David Yorston, Gartnavel Hospital, Glasgow, UK. No funding has been received for this work.
Author information
Authors and Affiliations
Consortia
Contributions
DHWS contributed to the design of the study, interpretation of the data, the correction of the draft, and the final revision. PA analysed the data. DY, THW, DAL and MF contributed to the interpretation of the data. MF, AS, MAZ wrote the first draft and created the tables and the figures. All authors provided feedback on the draft, revised the final version, read and approved the final manuscript. All authors agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferrara, M., Al-Zubaidy, M., Song, A. et al. The effect of age on phenotype of primary rhegmatogenous retinal detachment. Eye 37, 1114–1122 (2023). https://doi.org/10.1038/s41433-022-02061-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-022-02061-y
This article is cited by
-
The rising tide of rhegmatogenous retinal detachment in Germany: a nationwide analysis of the incidence, from 2005 to 2021
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)
-
The effect of sex and laterality on the phenotype of primary rhegmatogenous retinal detachment
Eye (2023)