Abstract
Background
To apply machine learning (ML) algorithms to perform multiclass diabetic retinopathy (DR) classification using both clinical data and optical coherence tomography angiography (OCTA).
Methods
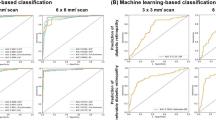
In this cross-sectional observational study, clinical data and OCTA parameters from 203 diabetic patients (203 eye) were used to establish the ML models, and those from 169 diabetic patients (169 eye) were used for independent external validation. The random forest, gradient boosting machine (GBM), deep learning and logistic regression algorithms were used to identify the presence of DR, referable DR (RDR) and vision-threatening DR (VTDR). Four different variable patterns based on clinical data and OCTA variables were examined. The algorithms’ performance were evaluated using receiver operating characteristic curves and the area under the curve (AUC) was used to assess predictive accuracy.
Results
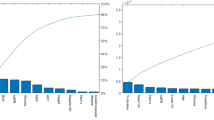
The random forest algorithm on OCTA+clinical data-based variables and OCTA+non-laboratory factor-based variables provided the higher AUC values for DR, RDR and VTDR. The GBM algorithm produced similar results, albeit with slightly lower AUC values. Leading predictors of DR status included vessel density, retinal thickness and GCC thickness, as well as the body mass index, waist-to-hip ratio and glucose-lowering treatment.
Conclusions
ML-based multiclass DR classification using OCTA and clinical data can provide reliable assistance for screening, referral, and management DR populations.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
269,00 € per year
only 14,94 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data used in the current study is available from the corresponding author upon request.
References
Teo ZL, Tham YC, Yu M, Chee ML, Rim TH, Cheung N, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128:1580–91.
Jaimie, Rupert RAB DA, Paul, Seth SB, Hugh RBT RF, Jost BJ, et al. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9:e144–60.
Flaxel CJ, Adelman RA, Bailey ST, Fawzi A, Lim JI, Vemulakonda GA, et al. Diabetic retinopathy preferred practice Pattern®. Ophthalmology. 2020;127:66–145.
Tan GS, Cheung N, Simó R, Cheung GC, Wong TY. Diabetic macular oedema. Lancet Diabetes Endocrinol. 2017;5:143–55.
Wong TY, Sun J, Kawasaki R, Ruamviboonsuk P, Gupta N, Lansingh VC, et al. Guidelines on diabetic eye care: the international council of ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology 2018;125:1608–22.
Wu JH, Liu TYA, Hsu WT, Ho JH, Lee CC. Performance and limitation of machine learning algorithms for diabetic retinopathy screening: meta-analysis. J Med Internet Res. 2021;23:e23863.
Gulshan V, Peng L, Coram M, Stumpe MC, Wu D, Narayanaswamy A, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. Jama. 2016;316:2402–10.
Gargeya R, Leng T. Automated identification of diabetic retinopathy using deep learning. Ophthalmology. 2017;124:962–69.
Abràmoff MD, Lou Y, Erginay A, Clarida W, Amelon R, Folk JC, et al. Improved automated detection of diabetic retinopathy on a publicly available dataset through integration of deep learning. Investig Ophthalmol Vis Sci. 2016;57:5200–06.
Li X, Xie J, Zhang L, Cui Y, Zhang G, Chen X, et al. Identifying microvascular and neural parameters related to the severity of diabetic retinopathy using optical coherence tomography angiography. Invest Ophthalmol Vis Sci. 2020;61:39.
Huang T, Li X, Xie J, Zhang L, Zhang G, Zhang A, et al. Long-term retinal neurovascular and choroidal changes after panretinal photocoagulation in diabetic retinopathy. Front Med. 2021;8:752538.
Hormel TT, Hwang TS, Bailey ST, Wilson DJ, Huang D, Jia Y. Artificial intelligence in OCT angiography. Prog Retin Eye Res. 2021;85:100965.
Sandhu HS, Elmogy M, Taher Sharafeldeen A, Elsharkawy M, El-Adawy N, Eltanboly A, et al. Automated diagnosis of diabetic retinopathy using clinical biomarkers, optical coherence tomography, and optical coherence tomography angiography. Am J Ophthalmol. 2020;216:201–06.
Sandhu HS, Eladawi N, Elmogy M, Keynton R, Helmy O, Schaal S, et al. Automated diabetic retinopathy detection using optical coherence tomography angiography: a pilot study. Br J Ophthalmol. 2018;102:1564–69.
Aslam TM, Hoyle DC, Puri V, Bento G. Differentiation of diabetic status using statistical and machine learning techniques on optical coherence tomography angiography images. Transl Vis Sci Technol. 2020;9:2.
Zang P, Hormel TT, Wang X, Tsuboi K, Huang D, Hwang TS, et al. A diabetic retinopathy classification framework based on deep-learning analysis of OCT angiography. Transl Vis Sci Technol. 2022;11:10.
Ryu G, Lee K, Park D, Kim I, Park SH, Sagong M. A deep learning algorithm for classifying diabetic retinopathy using optical coherence tomography angiography. Transl Vis Sci Technol. 2022;11:39.
Zang P, Gao L, Hormel TT, Wang J, You Q, Hwang TS, et al. DcardNet: diabetic retinopathy classification at multiple levels based on structural and angiographic optical coherence tomography. IEEE Trans Biomed Eng. 2021;68:1859–70.
Zhang G, Chen H, Chen W, Zhang M. Prevalence and risk factors for diabetic retinopathy in China: a multi-hospital-based cross-sectional study. Br J Ophthalmol. 2017;101:1591–95.
Song P, Yu J, Chan KY, Theodoratou E, Rudan I. Prevalence, risk factors and burden of diabetic retinopathy in China: a systematic review and meta-analysis. J Glob Health. 2018;8:010803.
Wan H, Cai Y, Wang Y, Fang S, Chen C, Chen Y, et al. The unique association between the level of peripheral blood monocytes and the prevalence of diabetic retinopathy: a cross-sectional study. J Transl Med. 2020;18:248.
Hasan M, Kotov A, Carcone A, Dong M, Naar S, Hartlieb KB. A study of the effectiveness of machine learning methods for classification of clinical interview fragments into a large number of categories. J Biomed Inf. 2016;62:21–31.
Oh E, Yoo TK, Park EC. Diabetic retinopathy risk prediction for fundus examination using sparse learning: a cross-sectional study. BMC Med Inf Decis Mak. 2013;13:106.
Blighe K, Gurudas S, Lee Y, Sivaprasad S. Diabetic retinopathy Environment-Wide Association Study (EWAS) in NHANES 2005-2008. J Clin Med. 2020;9:3643.
Ogunyemi OI, Gandhi M, Lee M, Teklehaimanot S, Daskivich LP, Hindman D, et al. Detecting diabetic retinopathy through machine learning on electronic health record data from an urban, safety net healthcare system. JAMIA Open. 2021;4:ooab066.
Cichosz SL, Johansen MD, Knudsen ST, Hansen TK, Hejlesen O. A classification model for predicting eye disease in newly diagnosed people with type 2 diabetes. Diabetes Res Clin Pract. 2015;108:210–5.
Tsao HY, Chan PY, Su EC. Predicting diabetic retinopathy and identifying interpretable biomedical features using machine learning algorithms. BMC Bioinforma. 2018;19:283.
Ogunyemi O, Kermah D. Machine learning approaches for detecting diabetic retinopathy from clinical and public health records. AMIA Annu Symp Proc. 2015;2015:983–90.
Yang C, Liu Q, Guo H, Zhang M, Zhang L, Zhang G, et al. Usefulness of machine learning for identification of referable diabetic retinopathy in a large-scale population-based study. Front Med. 2021;8:773881.
Ogunyemi OI, Gandhi M, Tayek C. Predictive models for diabetic retinopathy from non-image teleretinal screening data. AMIA Jt Summits Transl Sci Proc. 2019;2019:472–77.
Li HY, Dong L, Zhou WD, Wu HT, Zhang RH, Li YT, et al. Development and validation of medical record-based logistic regression and machine learning models to diagnose diabetic retinopathy. Graefes Arch Clin Exp Ophthalmol. 2023;261:681–89.
Li W, Song Y, Chen K, Ying J, Zheng Z, Qiao S, et al. Predictive model and risk analysis for diabetic retinopathy using machine learning: a retrospective cohort study in China. BMJ Open. 2021;11:e050989.
Hirano T, Kitahara J, Toriyama Y, Kasamatsu H, Murata T, Sadda S. Quantifying vascular density and morphology using different swept-source optical coherence tomography angiographic scan patterns in diabetic retinopathy. Br J Ophthalmol. 2019;103:216–21.
Su B, Zhu X, Yang K, Xiao Y, Li C, Shi K, et al. Age- and sex-related differences in the retinal capillary plexus in healthy Chinese adults. Eye Vis (Lond). 2022;9:38.
Monteiro-Henriques I, Rocha-Sousa A, Barbosa-Breda J. Optical coherence tomography angiography changes in cardiovascular systemic diseases and risk factors: a review. Acta Ophthalmol. 2022;100:e1–e15.
Katsimpris A, Karamaounas A, Sideri AM, Katsimpris J, Georgalas I, Petrou P. Optical coherence tomography angiography in Alzheimer’s disease: a systematic review and meta-analysis. Eye. 2022;36:1419–26.
Duan H, Xie J, Zhou Y, Zhang H, Liu Y, Tang C, et al. Characterization of the Retinal Microvasculature and FAZ Changes in Ischemic Stroke and Its Different Types. Transl Vis Sci Technol. 2022;11:21.
Subasi S, Kucuk KD, San S, Cefle A, Tokuc EO, Balci S, et al. Macular and peripapillary vessel density alterations in a large series of patients with systemic lupus erythematosus without ocular involvement. Graefes Arch Clin Exp Ophthalmol. 2022;260:3543–52.
Saini DC, Kochar A, Poonia R. Clinical correlation of diabetic retinopathy with nephropathy and neuropathy. Indian J Ophthalmol. 2021;69:3364–8. https://doi.org/10.4103/ijo.IJO_1237_21
WHO. The global burden of disease 2004 update. Geneva, Switzerland: World Health Organization; 2004.
Hu Y, Teng W, Liu L, Cheng K, Liu L, Hua R, et al. Prevalence and risk factors of diabetes and diabetic retinopathy in Liaoning province, China: a population-based cross-sectional study. PLoS One. 2015;10:e0121477.
Rajput D, Wang WJ, Chen CC. Evaluation of a decided sample size in machine learning applications. BMC Bioinforma. 2023;24:48.
Funding
This work was supported by the National Natural Science Foundation of China (grant numbers 82171072), the Guangdong Basic and Applied Basic Research Foundation (grant numbers 2021A1515010921, 2022A1515012073), the Guangzhou Science and Technology Program Project (grant numbers 202002030400); and the Sun Yat-sen Clinical Research Cultivating Program (grant numbers SYS-Q-202104).
Author information
Authors and Affiliations
Contributions
XL and XW collected and analysed the data, interpreted the results and wrote the manuscript. XS, QM, XL and GZ analysed and interpreted the data. LZ, YC, XL, YL and QM contributed to discussion and reviewed the manuscript. JL, JX, TH, ZC, ZL and XW collected the data. QM and YL designed this study, analysed the data, interpreted the results and revised the manuscript. All authors approved the final version of the manuscript. QM and YL are the guarantors of this work and had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, X., Wen, X., Shang, X. et al. Identification of diabetic retinopathy classification using machine learning algorithms on clinical data and optical coherence tomography angiography. Eye 38, 2813–2821 (2024). https://doi.org/10.1038/s41433-024-03173-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03173-3
This article is cited by
-
A novel deep learning approach for diabetic retinopathy classification using optical coherence tomography angiography
Multimedia Tools and Applications (2025)
-
Diabetic Retinopathy (DR) nomogram construction based on optical coherence tomography angiography parameters: a preliminary exploration of DR prediction
Graefe's Archive for Clinical and Experimental Ophthalmology (2025)
-
Sustaining Ophthalmic Practices for the Future: A High-Value Care Approach to Environmental Responsibility
Ophthalmology and Therapy (2025)