Abstract
Background
To compare conventional internal limiting membrane (ILM) peeling versus inverted flap technique in small idiopathic macular hole.
Methods
Retrospective, multicentre cohort study including consecutive eyes with a ≤250 μm idiopathic macular hole treated with primary vitrectomy. The primary outcome was best-corrected visual acuity (BCVA) change and macular hole closure rate. Closure patterns on optical coherence tomography (OCT) and rates of external limiting membrane (ELM) and ellipsoid zone (EZ) recovery were considered as secondary outcomes.
Results
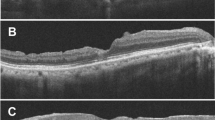
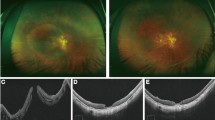
A total of 389 and 250 eyes were included in the conventional ILM peeling group and in the inverted flap group, respectively. Hole closure rate was comparable between the two groups (98.5% in the ILM peeling group and 97.6% in the inverted flap group). Mean BCVA was comparable between the two groups at baseline (p = 0.331). At 12 months, mean BCVA was 0.14 ± 0.19 logMAR in the conventional ILM peeling group and 0.17 ± 0.18 logMAR in the inverted flap group (p = 0.08). At 12 months, 73% of eyes had a U-shape closure morphology in the conventional ILM peeling group versus 55% in the inverted flap group. At 12 months, ELM recovery rate was 96% and 86% in the conventional ILM peeling group and in the inverted flap group, respectively (p < 0.001); EZ recovery rate was 78% and 69%, respectively (p = 0.04).
Conclusions
The inverted flap technique provides no advantages in terms of visual outcome and closure rate in small idiopathic macular hole surgery. Additionally, this technique seems to impair postoperative restoration of external retinal layers compared with conventional peeling.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
269,00 € per year
only 14,94 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets analysed during the current study are available from the corresponding author on reasonable request.
References
Park DW, Sipperley JO, Sneed SR, Dugel PU, Jacobsen J. Macular hole surgery with internal-limiting membrane peeling and intravitreous air. Ophthalmology. 1999;106:1392–8.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Shen Y, Lin X, Zhang L, Wu M. Comparative efficacy evaluation of inverted internal limiting membrane flap technique and internal limiting membrane peeling in large macular holes: a systematic review and meta-analysis. BMC Ophthalmol. 2020;20:14.
Rizzo S, Tartaro R, Barca F, Caporossi T, Bacherini D, Giansanti F. Internal limiting membrane peeling versus inverted flap technique for treatment of full-thickness macular holes: a comparative study in a large series of patients. Retina. 2018;38:S73–S78.
Ch’ng SW, Patton N, Ahmed M, Ivanova T, Baumann C, Charles S, et al. The Manchester large macular hole study: is it time to reclassify large macular holes? Am J Ophthalmol. 2018;195:36–42.
Yamashita T, Sakamoto T, Terasaki H, Iwasaki M, Ogushi Y, Okamoto F, et al. Best surgical technique and outcomes for large macular holes: retrospective multicentre study in Japan. Acta Ophthalmol. 2018;96:e904–e910.
Li P, Li L, Wu J. Inverted internal limiting membrane flap versus internal limiting membrane peeling for <400 μm macular hole: a meta-analysis and systematic review. Ophthalmic Res. 2023; 66. https://pubmed.ncbi.nlm.nih.gov/37931613/.
Baumann C, Dervenis N, Kirchmair K, Lohmann CP, Kaye SB, Sandinha MT. Functional and morphological outcomes of the inverted internal limiting membrane flap technique in small-sized and medium-sized macular holes. Retina. 2021;41:2073–8. https://pubmed.ncbi.nlm.nih.gov/33758135/.
Chou H-D, Liu L, Wang C-T, Chen K-J, Wu W-C, Hwang Y-S, et al. Single-layer inverted internal limiting membrane flap versus conventional peel for small- or medium-sized full-thickness macular holes. Am J Ophthalmol. 2022;235:111–9. https://doi.org/10.1016/j.ajo.2021.08.016.
Ventre L, Fallico M, Longo A, Parisi G, Russo A, Bonfiglio V, et al. Conventional internal limiting membrane peeling versus inverted flap for small-to-medium idiopathic macular hole: a randomized trial. Retina. 2022;42. https://pubmed.ncbi.nlm.nih.gov/36084331/.
Fallico M, Jackson TL, Chronopoulos A, Hattenbach LO, Longo A, Bonfiglio V, et al. Factors predicting normal visual acuity following anatomically successful macular hole surgery. Acta Ophthalmol. 2021;99:e324–e329.
Iuliano L, Corbelli E, Bandello F, Codenotti M. Inverted internal limiting membrane flap for small-sized (<250 µm) full-thickness macular hole: anatomical and functional outcome. Retina. 2023;43:547–54. https://pubmed.ncbi.nlm.nih.gov/36728896/.
Duker JS, Kaiser PK, Binder S, De Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology. 2013;120:2611–9. https://pubmed.ncbi.nlm.nih.gov/24053995/.
Parisi G, Fallico M, Maugeri A, Barchitta M, Agodi A, Russo A, et al. Primary vitrectomy for degenerative and tractional lamellar macular holes: a systematic review and meta-analysis. PLoS ONE. 2021;16. https://pubmed.ncbi.nlm.nih.gov/33667237/.
Michalewska Z, Michalewski J, Cisiecki S, Adelman R, Nawrocki J. Correlation between foveal structure and visual outcome following macular hole surgery: a spectral optical coherence tomography study. Graefe’s Arch Clin Exp Ophthalmol. 2008;246:823–30.
Haller JA, Stalmans P, Benz MS, Gandorfer A, Pakola SJ, Girach A, et al. Efficacy of intravitreal ocriplasmin for treatment of vitreomacular adhesion: subgroup analyses from two randomized trials. Ophthalmology. 2015;122:117–22. https://pubmed.ncbi.nlm.nih.gov/25240630/.
Chan CK, Mein CE, Glassman AR, Beaulieu WT, Calhoun CT, Jaffe GJ, et al. Pneumatic vitreolysis with perfluoropropane for vitreomacular traction with and without macular hole: DRCR retina network protocols AG and AH. Ophthalmology. 2021;128:1592–603. https://pubmed.ncbi.nlm.nih.gov/33989683/
Chan CK, Crosson JN, Mein CE, Daher N. Pneumatic vitreolysis for relief of vitreomacular traction. Retina. 2017;37:1820–31. https://pubmed.ncbi.nlm.nih.gov/28099316/.
Morescalchi F, Costagliola C, Gambicorti E, Duse S, Romano MR, Semeraro F. Controversies over the role of internal limiting membrane peeling during vitrectomy in macular hole surgery. Surv Ophthalmol. 2017;62:58–69. https://pubmed.ncbi.nlm.nih.gov/27491476/.
Tadayoni R, Gaudric A, Haouchine B, Massin P. Relationship between macular hole size and the potential benefit of internal limiting membrane peeling. Br J Ophthalmol. 2006;90:1239–41. https://pubmed.ncbi.nlm.nih.gov/16809385/.
Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, et al. Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Investig Ophthalmol Vis Sci. 2011;52:1586–92. https://pubmed.ncbi.nlm.nih.gov/21051731/.
Neubauer J, Gelisken F, Ozturk T, Bartz-Schmidt KU, Dimopoulos S. The time course of spontaneous closure of idiopathic full-thickness macular holes. Graefe’s Arch Clin Exp Ophthalmol. 2024. https://pubmed.ncbi.nlm.nih.gov/38587655/.
Gu C, Qiu Q. Inverted internal limiting membrane flap technique for large macular holes: a systematic review and single-arm meta-analysis. Graefe’s Arch Clin Exp Ophthalmol. 2018;256:1041–9.
Yamada K, Oishi A, Kusano M, Kinoshita H, Tsuiki E, Kitaoka T. Effect of inverted internal limiting membrane flap technique on small-medium size macular holes. Sci Rep. 2022;12. https://pubmed.ncbi.nlm.nih.gov/35031664/.
Park JH, Lee SM, Park SW, Lee JE, Byon IS. Comparative analysis of large macular hole surgery using an internal limiting membrane insertion versus inverted flap technique. Br J Ophthalmol. 2019;103:245–50.
Iwasaki M, Miyamoto H, Imaizumi H. Effects of inverted internal limiting membrane technique and insertion technique on outer retinal restoration associated with glial proliferation in large macular holes. Graefe’s Arch Clin Exp Ophthalmol. 2020;258:1841–9.
Ventre L, Fallico M, Longo A, Parisi G, Russo A, Bonfiglio V, et al. Reply. Retina 2023;43:E27. https://pubmed.ncbi.nlm.nih.gov/36796036/.
Acknowledgements
We are grateful to Dott. A. Bridgewood of the Scientific Bureau of the University of Catania for language editing.
Author information
Authors and Affiliations
Consortia
Contributions
Each author made substantial contributions to the realisation of the work. MR was a major contributor in the conception and design of the research; MF and PC in the acquisition and interpretation of the data and in writing the manuscript; FR, FG and LC in the analysis of data; PM, GP and EB in revising the manuscript. SMALL Study Group had a key role in the acquisition of the data and in revising the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fallico, M., Caselgrandi, P., Marolo, P. et al. Vitrectomy in Small idiopathic MAcuLar hoLe (SMALL) study: conventional internal limiting membrane peeling versus inverted flap. Eye 38, 3334–3340 (2024). https://doi.org/10.1038/s41433-024-03301-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03301-z