Abstract
Objective
The study aimed to evaluate the interocular symmetry of macular sublayer thickness among healthy children aged 6-12 years.
Methods
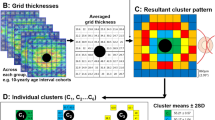
The Shiraz Pediatric Eye Study included 500 randomly selected children who underwent SD-OCT of the macula and optical biometry using the IOLMaster-500. Exclusion criteria involved ocular abnormalities or axial lengths outside the 21.5–26.5 mm range. Software recorded total retinal thickness and sublayer thickness within each ETDRS subfield.
Results
The study included 862 eyes from 431 healthy children, with 254 girls (59%). The anticipated variation in total retinal thickness between eyes was below 13 µm in the fovea and under 7 µm in the inner or outer ring for 95% of the population. For nerve fiber layer and inner plexiform layer, the expected variation ranged from 2 to 4 µm, and for the ganglion-cell layer, it ranged from 2.5 to 5 µm. Intraclass correlation coefficient (ICC) rankings for retinal topography were highest in the outer ring, followed by the inner ring and fovea. The highest ICC for individual layers was found in overall retinal thickness, followed by inner retinal layers, outer-nuclear layer, inner plexiform layer, and inner nuclear layer.
Conclusions
The study establishes a reliable reference range for interocular variances in macular sublayers, aiding clinical decision-making. The outer ring (3–6 mm) is most dependable for analysing most sublayers, while the inner ring is most suitable for examining the ganglion-cell layer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
269,00 € per year
only 14,94 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data used during this study are available from the corresponding author upon reasonable request.
References
Quellec G, Lee K, Dolejsi M, Garvin MK, Abramoff MD, Sonka M. Three-dimensional analysis of retinal layer texture: identification of fluid-filled regions in SD-OCT of the macula. IEEE Trans Med imaging. 2010;29:1321–30.
Yuksel Elgin C, Chen D, Al‐Aswad LAJC, Ophthalmology E. Ophthalmic imaging for the diagnosis and monitoring of glaucoma: a review. 2022;50:183–97.
Budenz DL. Symmetry between the right and left eyes of the normal retinal nerve fiber layer measured with optical coherence tomography (an AOS thesis). Trans Am Ophthalmol Soc. 2008;106:252.
Al-Haddad C, Antonios R, Tamim H. Interocular symmetry in retinal and optic nerve parameters in children as measured by spectral ___domain optical coherence tomography. Br J Ophthalmol. 2014;98:502–6.
Karadag AS, Bilgin B, Soylu MB. Comparison of optical coherence tomographic findings between Behcet disease patients with and without ocular involvement and healthy subjects. Arquivos Brasileiros De Oftalmologia. 2017;80:69–73.
Grover S, Murthy RK, Brar VS, Chalam KV. Comparison of retinal thickness in normal eyes using Stratus and Spectralis optical coherence tomography. Investig Ophthalmol Vis Sci. 2010;51:2644–7.
Dalgliesh JD, Tariq YM, Burlutsky G, Mitchell P. Symmetry of retinal parameters measured by spectral-___domain OCT in normal young adults. J Glaucoma. 2015;24:20–4.
Liu GY, Utset TO, Bernard JT. Retinal nerve fiber layer and macular thinning in systemic lupus erythematosus: an optical coherence tomography study comparing SLE and neuropsychiatric SLE. Lupus. 2015;24:1169–76.
Xia Z, Chen H, Zheng S. Thicknesses of macular inner retinal layers in children with anisometropic amblyopia. BioMed Res Int. 2020;2020:6853258.
Zakaria Eid M, Mahmoud Amin A, El-Sayed Mohamed M. Changes in macular thickness after part-time occlusion in children with amblyopia using optical coherence tomography (OCT). Al-Azhar Med J. 2020;49:117–24.
Giani A, Cigada M, Choudhry N, Deiro AP, Oldani M, Pellegrini M, et al. Reproducibility of retinal thickness measurements on normal and pathologic eyes by different optical coherence tomography instruments. Am J Ophthalmol. 2010;150:815–24.e811.
Seibold LK, Mandava N, Kahook MY. Comparison of retinal nerve fiber layer thickness in normal eyes using time-___domain and spectral-___domain optical coherence tomography. Am J Ophthalmol. 2010;150:807–14.e801.
Zhou M, Lu B, Zhao J, Wang Q, Zhang P, Sun XJPO. Interocular symmetry of macular ganglion cell complex thickness in young Chinese subjects. PLoS ONE. 2016;11:e0159583.
Altemir I, Oros D, Elía N, Polo V, Larrosa JM, Pueyo V. Retinal asymmetry in children measured with optical coherence tomography. Am J Ophthalmol. 2013;156:1238–43.e1231.
Leung CK, Ye C, Weinreb RN, Yu M, Lai G, Lam DSJO. Impact of age-related change of retinal nerve fiber layer and macular thicknesses on evaluation of glaucoma progression. Ophthalmology. 2013;120:2485–92.
Lee JY, Hwang YH, Lee SM, Kim YY. Age and retinal nerve fiber layer thickness measured by spectral ___domain optical coherence tomography. Korean J Ophthalmol. 2012;26:163–8.
Hirasawa K, Shoji N. Association between ganglion cell complex and axial length. Jpn J Ophthalmol. 2013;57:429–34.
Makhmutov V, Adler W, Matos PAW, Kopecky A, Nemcansky J, Rokohl AC, et al. Intraday repeatability of macular layers measurements in glaucomatous and non-glaucomatous patients using spectral-___domain optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2024;262:3287–94.
Author information
Authors and Affiliations
Contributions
Conception and design: AZ, RR, MRT, MRK, MSM, MHN; Acquisition and interpretation of data: ZS, HM, MK, EM, ZT; Data analysis: MHN; Drafting: All authors; Critical reviewing: AZ, RR, MRT, MRK, MSM, MHN; Final approval: All authors; Agreement to be accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zareei, A., Razeghinejad, R., Talebnejad, M.R. et al. Establishing normal interocular symmetry range for macular optical coherence tomography parameters in healthy children. Eye 39, 563–569 (2025). https://doi.org/10.1038/s41433-024-03591-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03591-3