Abstract
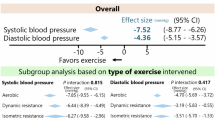
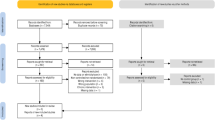
Although hypertension is a major cause of cardiovascular disease, the control of blood pressure (BP) is insufficient worldwide. Exercise is an effective treatment for reducing BP, but the differences in the blood pressure lowering effects of exercise according to the underlying pathophysiological condition, the type of exercise, and the geographic region are not fully understood. An umbrella review with a meta-analysis of 435 randomized controlled trials that investigated the BP-lowering effects of exercise was performed using Ovid MEDLINE and the Cochrane Library, covering the period from inception to August 1, 2023. A random effects model meta-analysis was performed to estimate the effect size across multiple studies. Exercise significantly reduced systolic BP in healthy subjects (−3.51 mmHg, 95% confidence interval: −3.90, −3.11; p < 0.001) and in those with lifestyle-related diseases including hypertension (−5.48 mmHg, −6.51, −4.45; p < 0.001), but not in those with cardiovascular diseases (−1.16 mmHg, −4.08, 1.76; p = 0.44). According to the type of exercise, all types significantly reduced systolic BP in healthy subjects and in those with lifestyle-related diseases, but not in those with cardiovascular diseases. According to the region, in Oceania, there were no reductions in systolic BP. In Asia, systolic BP was reduced in patients with cardiovascular diseases. In conclusion, any type of exercise reduced BP in healthy subjects and in those with lifestyle-related diseases, but not in those with cardiovascular diseases, and the region affected the effect of exercise. When using exercise to reduce hypertension, it is important to consider the patient’s pathophysiological condition and the region.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kario K, Okura A, Hoshide S, Mogi M. The WHO Global report 2023 on hypertension warning the emerging hypertension burden in globe and its treatment strategy. Hypertens Res. 2024;47:1099–102.
Umemura S, Arima H, Arima S, Asayama K, Dohi Y, Hirooka Y, et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens Res. 2019;42:1235–481.
Messerli FH, Williams B, Ritz E. Essential hypertension. Lancet. 2007;370:591–603.
World Health Organization. Global report on hypertension: the race against a silent killer. Geneva, Switzerland: World Health Organization; 2023, p. 1–276.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997;336:1117–24.
He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48:861–9.
Norman D, Loredo JS, Nelesen RA, Ancoli-Israel S, Mills PJ, Ziegler MG, et al. Effects of continuous positive airway pressure versus supplemental oxygen on 24-hour ambulatory blood pressure. Hypertension. 2006;47:840–5.
Edwards JJ, Coleman DA, Ritti-Dias RM, Farah BQ, Stensel DJ, Lucas SJE, et al. Isometric Exercise Training and Arterial Hypertension: An Updated Review. Sports Med. 2024;54:1459–97.
Gambardella J, Morelli MB, Wang XJ, Santulli G. Pathophysiological mechanisms underlying the beneficial effects of physical activity in hypertension. J Clin Hypertens. 2020;22:291–5.
Motoyama M, Sunami Y, Kinoshita F, Kiyonaga A, Tanaka H, Shindo M, et al. Blood pressure lowering effect of low intensity aerobic training in elderly hypertensive patients. Med Sci Sports Exerc. 1998;30:818–23.
Hagberg JM, Montain SJ, Martin WH 3rd, Ehsani AA. Effect of exercise training in 60- to 69-year-old persons with essential hypertension. Am J Cardiol. 1989;64:348–53.
Lee LL, Mulvaney CA, Wong YKY, Chan ES, Watson MC, Lin HH. Walking for hypertension. Cochrane Database Syst Rev. 2021;2:CD008823.
Fecchio RY, de Sousa JCS, Oliveira-Silva L, da Silva Junior ND, Pio-Abreu A, da Silva GV, et al. Effects of dynamic, isometric and combined resistance training on blood pressure and its mechanisms in hypertensive men. Hypertens Res. 2023;46:1031–43.
MacDonald HV, Johnson BT, Huedo-Medina TB, Livingston J, Forsyth KC, Kraemer WJ, et al. Dynamic Resistance Training as Stand-Alone Antihypertensive Lifestyle Therapy: A Meta-Analysis. J Am Heart Assoc. 2016;5:e003231.
Baffour-Awuah B, Pearson MJ, Dieberg G, Smart NA. Isometric Resistance Training to Manage Hypertension: Systematic Review and Meta-analysis. Curr Hypertens Rep. 2023;25:35–49.
Caminiti G, Iellamo F, Mancuso A, Cerrito A, Montano M, Manzi V, et al. Effects of 12 weeks of aerobic versus combined aerobic plus resistance exercise training on short-term blood pressure variability in patients with hypertension. J Appl Physiol. 2021;130:1085–92.
Pires NF, Coelho-Junior HJ, Gambassi BB, de Faria APC, Ritter AMV, de Andrade Barboza C, et al. Combined Aerobic and Resistance Exercises Evokes Longer Reductions on Ambulatory Blood Pressure in Resistant Hypertension: A Randomized Crossover Trial. Cardiovasc Ther. 2020;2020:8157858.
Kanaley JA, Colberg SR, Corcoran MH, Malin SK, Rodriguez NR, Crespo CJ, et al. Exercise/Physical Activity in Individuals with Type 2 Diabetes: A Consensus Statement from the American College of Sports Medicine. Med Sci Sports Exerc. 2022;54:353–68.
Phoemsapthawee J, Sriton B. Combined exercise training improves blood pressure at rest and during exercise in young obese prehypertensive men. J Sports Med Phys Fit. 2021;61:468–79.
Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2013;2:e004473.
Carlson DJ, Dieberg G, Hess NC, Millar PJ, Smart NA. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clin Proc. 2014;89:327–34.
Schultz MG, La Gerche A, Sharman JE. Blood Pressure Response to Exercise and Cardiovascular Disease. Curr Hypertens Rep. 2017;19:89.
Peng Y, Su Y, Wang YD, Yuan LR, Wang R, Dai JS. Effects of regular dance therapy intervention on blood pressure in hypertension individuals: a systematic review and meta-analysis. J Sports Med Phys Fit. 2021;61:301–9.
Wang Y, Liu Y, Liu L, Hong L, Chen H. Comparative Analysis of Hypertension Guidelines: Unveiling Consensus and Discrepancies in Lifestyle Modifications for Blood Pressure Control. Cardiol Res Pr. 2023;2023:5586403.
Saco-Ledo G, Valenzuela PL, Ruiz-Hurtado G, Ruilope LM, Lucia A. Exercise Reduces Ambulatory Blood Pressure in Patients With Hypertension: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J Am Heart Assoc. 2020;9:e018487.
Wen H, Wang L. Reducing effect of aerobic exercise on blood pressure of essential hypertensive patients: A meta-analysis. Medicine. 2017;96:e6150.
Cornelissen VA, Fagard RH. Effects of endurance training on blood pressure, blood pressure-regulating mechanisms, and cardiovascular risk factors. Hypertension. 2005;46:667–75.
Edwards JJ, Deenmamode AHP, Griffiths M, Arnold O, Cooper NJ, Wiles JD, et al. Exercise training and resting blood pressure: a large-scale pairwise and network meta-analysis of randomised controlled trials. Br J Sports Med. 2023;57:1317–26.
Hanssen H, Boardman H, Deiseroth A, Moholdt T, Simonenko M, Krankel N, et al. Personalized exercise prescription in the prevention and treatment of arterial hypertension: a Consensus Document from the European Association of Preventive Cardiology (EAPC) and the ESC Council on Hypertension. Eur J Prev Cardiol. 2022;29:205–15.
Li T, Jiang H, Ding J. The role of exercise-based cardiac rehabilitation after percutaneous coronary intervention in patients with coronary artery disease: a meta-analysis of randomised controlled trials. Acta Cardiol. 2024;79:127–35.
Oldridge N. Exercise-based cardiac rehabilitation in patients with coronary heart disease: meta-analysis outcomes revisited. Future Cardiol. 2012;8:729–51.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
De Ciuceis C, Rizzoni D, Palatini P. Microcirculation and Physical Exercise In Hypertension. Hypertension. 2023;80:730–9.
Makita S, Yasu T, Akashi YJ, Adachi H, Izawa H, Ishihara S, et al. JCS/JACR 2021 Guideline on Rehabilitation in Patients With Cardiovascular Disease. Circ J. 2022;87:155–235.
Schuttler D, Clauss S, Weckbach LT, Brunner S. Molecular Mechanisms of Cardiac Remodeling and Regeneration in Physical Exercise. Cells. 2019;8:1128.
Carvalho VO, Ciolac EG, Guimaraes GV, Bocchi EA. Effect of exercise training on 24-hour ambulatory blood pressure monitoring in heart failure patients. Congest Heart Fail. 2009;15:176–80.
Mitchell BL, Davison K, Parfitt G, Spedding S, Eston RG. Physiological and Perceived Exertion Responses during Exercise: Effect of beta-blockade. Med Sci Sports Exerc. 2019;51:782–91.
Forton K, Lamotte M, Gillet A, Chaumont M, van de Borne P, Faoro V. Beta-Adrenergic Receptor Blockade Effects on Cardio-Pulmonary Exercise Testing in Healthy Young Adults: A Randomized, Placebo-Controlled Trial. Sports Med Open. 2022;8:150.
Taylor RS, Unal B, Critchley JA, Capewell S. Mortality reductions in patients receiving exercise-based cardiac rehabilitation: how much can be attributed to cardiovascular risk factor improvements? Eur J Cardiovasc Prev Rehabil. 2006;13:369–74.
Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682–92.
Fraga R, Franco FG, Roveda F, de Matos LN, Braga AM, Rondon MU, et al. Exercise training reduces sympathetic nerve activity in heart failure patients treated with carvedilol. Eur J Heart Fail. 2007;9:630–6.
Bristow MR. The adrenergic nervous system in heart failure. N Engl J Med. 1984;311:850–1.
Pina IL, Apstein CS, Balady GJ, Belardinelli R, Chaitman BR, Duscha BD, et al. Exercise and heart failure: A statement from the American Heart Association Committee on exercise, rehabilitation, and prevention. Circulation. 2003;107:1210–25.
Brown MD, Feairheller DL. Are there race-dependent endothelial cell responses to exercise? Exerc Sport Sci Rev. 2013;41:44–54.
Feairheller DL, Park JY, Rizzo V, Kim B, Brown MD. Racial differences in the responses to shear stress in human umbilical vein endothelial cells. Vasc Health Risk Manag. 2011;7:425–31.
Collaboration NCDRF. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Collaborators GBDRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
Overweight and Obesity. The Australian Government, Australian Institute of Health and Welfare. 2014. Available online: https://www.aihw.gov.au/reports/overweight-obesity/overweight-and-obesity/contents/about. Accessed on 19 September 2024.
Huse O, Hettiarachchi J, Gearon E, Nichols M, Allender S, Peeters A. Obesity in Australia. Obes Res Clin Pr. 2018;12:29–39.
Hayes A, Tan EJ, Killedar A, Lung T. Socioeconomic inequalities in obesity: modelling future trends in Australia. BMJ Open. 2019;9:e026525.
Grech A, Sui Z, Siu HY, Zheng M, Allman-Farinelli M, Rangan A. Socio-Demographic Determinants of Diet Quality in Australian Adults Using the Validated Healthy Eating Index for Australian Adults (HEIFA-2013). Healthcare. 2017;5:7.
Williams ED, Tapp RJ, Magliano DJ, Shaw JE, Zimmet PZ, Oldenburg BF. Health behaviours, socioeconomic status and diabetes incidence: the Australian Diabetes Obesity and Lifestyle Study (AusDiab). Diabetologia. 2010;53:2538–45.
Powles J, Fahimi S, Micha R, Khatibzadeh S, Shi P, Ezzati M, et al. Global, regional and national sodium intakes in 1990 and 2010: a systematic analysis of 24 h urinary sodium excretion and dietary surveys worldwide. BMJ Open. 2013;3:e003733.
Stevens AL, Ferferieva V, Bito V, Wens I, Verboven K, Deluyker D, et al. Exercise improves cardiac function and attenuates insulin resistance in Dahl salt-sensitive rats. Int J Cardiol. 2015;186:154–60.
Libonati JR, Gaughan JP. Low-intensity exercise training improves survival in Dahl salt hypertension. Med Sci Sports Exerc. 2006;38:856–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
KO has received grants from Otsuka Holdings. KN has received honoraria from AstraZeneca, Bayer Yakuhin, Boehringer Ingelheim Japan, Daiichi Sankyo, Eli Lilly Japan, Kowa, Mitsubishi Tanabe Pharma, MSD, Novartis Pharma, Novo Nordisk Pharma, Otsuka; research grants from Astellas, Bayer Yakuhin, Boehringer Ingelheim Japan, Fuji Yakuhin, Mochida Pharmaceutical, Novartis Pharma; and scholarships from Abbott Medical, Boehringer Ingelheim Japan, Daiichi Sankyo Healthcare, Mitsubishi Tanabe Pharma, Teijin Pharma. SM has received honoraria from Daiichi Sankyo, Otsuka Pharma. and Novartis Pharma, scholarships from Abbott Medical and Sumitomo Pharma, and research grants from AMGEN, Bayer Yakuhin, Novo Nordisk Pharma, and MSD.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suematsu, Y., Morita, H., Abe, M. et al. Differences in the effects of exercise on blood pressure depending on the physical condition of the subject and the type of exercise: a systematic review and meta-analysis. Hypertens Res 48, 720–732 (2025). https://doi.org/10.1038/s41440-024-01974-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-024-01974-3