Abstract
The seminal vesicles (SVs) have long been recognized for their role in male fertility, yet their contribution to male sexual function is often underestimated. In recent decades, studies have gradually unveiled an association between SVs and various male sexual dysfunctions (SDs), including diminished libido, erectile dysfunction, premature ejaculation, delayed ejaculation, and orgasmic disorder. We conducted a comprehensive literature search of publications up until April 2024 in PubMed, Google Scholar, and CNKI, focusing on original studies, case reports, and reviews addressing the relationship between SVs and male SDs. The aim was to explore the pathophysiological mechanisms, clinical evaluation, and management of this relationship, providing urologists and andrologists with new insights into diagnosing and treating complex male SDs. Current research suggests that SVs may play a role in male sexual function, but the evidence remains limited. Future large-scale, rigorously designed studies are needed to further validate this relationship.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data in this paper can be found by searching the listed references on PubMed, Google Scholar, and CNKI.
References
Brewster SF. The development and differentiation of human seminal vesicles. J Anat. 1985;143:45–55.
Aumüller G, Riva A. Morphology and functions of the human seminal vesicle. Andrologia. 1992;24:183–96.
Gonzales GF, Garcia-Hjarles MA, Gutierrez R, Guerra-Garcia R. The secretory activity of the seminal vesicles and its relationship to sperm motility: effects of infection in the male reproductive tract. Int J Androl. 1989;12:286–94.
Toragall MM, Satapathy SK, Kadadevaru GG, Hiremath MB. Evaluation of seminal fructose and citric acid levels in men with fertility problem. J Hum Reprod Sci. 2019;12:199–203.
Jin BF, Huang YF, Yang XY, Chen WZ, Xia XY, Jin JY, et al. The relationship between the secretary function of seminal vesical under MR image and the sexual function: a pilot research. Chin Imaging J Integr Tradit Western Med. 2006;4:413–7.
Jin BF, Huang YF, Zhu ZP, Zhang LB, Wu GZ. Experimental study on the influence upon rat’s sexual function after seminal vesicle was excised. J Nanjing Med Univ. 2006;31:268–70.
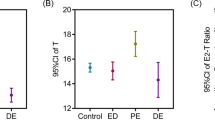
Hong ZW, Feng YM, Ge YF, Jing J, Hu XC, Shen JM, et al. Relation of size of seminal vesicles on ultrasound to premature ejaculation. Asian J Androl. 2017;19:554–60.
Mogorovich A, Nilsson AE, Tyritzis SI, Carlsson S, Jonsson M, Haendler L, et al. Radical prostatectomy, sparing of the seminal vesicles, and painful orgasm. J Sex Med. 2013;10:1417–23.
Tarchanoff IR. Zur physiologie des geschlechtsapparatus des frosches. Archiv für die Gesammte. Physiologie. 1887;40:330.
Allport FH. Social psychology. Boston, MA: Houghton Mifflin; 1924. p. 69–70.
Pauker RS. The effects of removing seminal vesicles, prostate, and testes on the mating behavior of the golden hamster Cricetus auratus. J Comp Physiol Psychol. 1948;41:252–7.
Beach FA, Wilson JR. Mating behavior in male rats after removal of the seminal vesicles. Proc Natl Acad Sci USA. 1963;49:624–6.
Larsson K, Swedin G. The sexual behavior of male rats after bilateral section of the hypogastric nerve and removal of the accessory genital glands. Physiol Behav. 1971;6:251–3.
Chow PH, Ng KW, Pang SF. Lack of effect of bilateral removal of accessory sex glands on sexual behaviour in the male golden hamster (Mesocricetus auratus). Physiol Behav. 1996;59:393–6.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The International Index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822–30.
Tang DD, Li C, Peng DW, Zhang XS. Validity of premature ejaculation diagnostic tool and its association with International Index of Erectile Function-15 in Chinese men with evidence-based-defined premature ejaculation. Asian J Androl. 2018;20:19–23.
Wang C, Zhang H, Liu Z, Tu X, Zhang Y. A modified procedure to diagnose erectile dysfunction using the International Index of Erectile Function (IIEF-6) combined with the premature ejaculation diagnosis tool (PEDT) via an internet survey. Sex Med. 2022;10:100506.
Yao Y, You YF. Correlation research of seminal vesicle secretion function with sexual function using MRI. Chin J Hum Sex. 2019;28:24–7.
Taniguchi H, Kawa G, Yoshida K, Takayasu K, Kinoshita H, Matsuda T. Relationship between volume of the seminal vesicles and sexual activity in middle-aged men. Andrologia. 2017;49. https://doi.org/10.1111/and.12618.
Birkhäuser FD, Schumacher C, Seiler R, de Meuron L, Zehnder P, Roth B, et al. Occlusion of seminal vesicles increases sexual activity in a mouse model. Eur Urol. 2012;62:855–62.
Mouras H, Stoléru S, Bittoun J, Glutron D, Pélégrini-Issac M, Paradis AL, et al. Brain processing of visual sexual stimuli in healthy men: a functional magnetic resonance imaging study. Neuroimage. 2003;20:855–69.
Weisstanner C, Pastore-Wapp M, Schmitt M, Zehnder P, Wiest R, Thalmann GN, et al. Distended seminal vesicles are involved in specific cerebral sexual arousal: a pilot study using functional brain imaging in young healthy men. Eur Urol Open Sci. 2022;42:10–6.
O’Connor DB, Lee DM, Corona G, Forti G, Tajar A, O’Neill TW, et al. The relationships between sex hormones and sexual function in middle-aged and older European men. J Clin Endocrinol Metab. 2011;96:E1577–87.
Cunningham GR, Stephens-Shields AJ, Rosen RC, Wang C, Bhasin S, Matsumoto AM, et al. Testosterone treatment and sexual function in older men with low testosterone levels. J Clin Endocrinol Metab. 2016;101:3096–104.
Tsuji M, Terada N, Sugihara A, Tsujimura T, Donjacour AA, Cunha GR. Later onset of apoptosis in the bulbourethral glands after castration compared to that in the seminal vesicles. J Steroid Biochem Mol Biol. 1998;67:113–8.
Mariotti A, Mawhinney M. Irreversible androgen induced growth in seminal vesicle smooth muscle. J Steroid Biochem. 1984;20:1361–3.
Mann T. Secretory function of the prostate, seminal vesicle and other male accessory organs of reproduction. J Reprod Fertil. 1974;37:179–88.
Aksglaede L, Jørgensen N, Skakkebaek NE, Juul A. Low semen volume in 47 adolescents and adults with 47,XXY Klinefelter or 46,XX male syndrome. Int J Androl. 2009;32:376–84.
Corona G, Petrone L, Paggi F, Lotti F, Boddi V, Fisher A, et al. Sexual dysfunction in subjects with Klinefelter’s syndrome. Int J Androl. 2010;33:574–80.
Sharma R, Agarwal A, Rohra VK, Assidi M, Abu-Elmagd M, Turki RF. Effects of increased paternal age on sperm quality, reproductive outcome and associated epigenetic risks to offspring. Reprod Biol Endocrinol. 2015;13:35.
Wylie K, Froggatt N. Late onset hypogonadism, sexuality and fertility. Hum Fertil. 2010;13:126–33.
Ogbera OA, Sonny C, Olufemi F, Wale A. Hypogonadism and subnormal total testosterone levels in men with type 2 diabetes mellitus. J Coll Physicians Surg Pak. 2011;21:517–21.
Lu X, Huang Y, Zhang H, Zhao J. Effect of diabetes mellitus on the quality and cytokine content of human semen. J Reprod Immunol. 2017;123:1–2.
Agbaje IM, Rogers DA, McVicar CM, McClure N, Atkinson AB, Mallidis C, et al. Insulin dependant diabetes mellitus: implications for male reproductive function. Hum Reprod. 2007;22:1871–7.
Corona G, Giorda CB, Cucinotta D, Guida P, Nada E, Gruppo di studio SUBITO-DE. Sexual dysfunction at the onset of type 2 diabetes: the interplay of depression, hormonal and cardiovascular factors. J Sex Med. 2014;11:2065–73.
Zitzmann M, Faber S, Nieschlag E. Association of specific symptoms and metabolic risks with serum testosterone in older men. J Clin Endocrinol Metab. 2006;91:4335–43.
Dean RC, Lue TF. Physiology of penile erection and pathophysiology of erectile dysfunction. Urol Clin North Am. 2005;32:379–v.
Kashiwagi E, Shiota M, Naganuma H, Monji K, Imada K, Lee K, et al. Testosterone level in seminal vesicle fluid is a better indicator of erectile function than serum testosterone in patients with prostate cancer. Int J Urol. 2022;29:1155–62.
Vroege JA. The sexual health inventory for men (IIEF-5). Int J Impot Res. 1999;11:177.
Zlotta AR, Roumeguère T, Ravery V, Hoffmann P, Montorsi F, Türkeri L, et al. Is seminal vesicle ablation mandatory for all patients undergoing radical prostatectomy? A multivariate analysis on 1283 patients. Eur Urol. 2004;46:42–9.
Simone G, Papalia R, Leonardo C, Sacco R, Damiano R, Guaglianone S, et al. Prostatic capsule and seminal vesicle-sparing cystectomy: improved functional results, inferior oncologic outcome. Urology. 2008;72:162–6.
Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol. 1982;128:492–7.
Gilbert SM, Dunn RL, Miller DC, Montgomery JS, Skolarus TA, Weizer AZ, et al. Functional outcomes following nerve sparing prostatectomy augmented with seminal vesicle sparing compared to standard nerve sparing prostatectomy: results from a randomized controlled trial. J Urol. 2017;198:600–7.
Menon M, Kaul S, Bhandari A, Shrivastava A, Tewari A, Hemal A. Potency following robotic radical prostatectomy: a questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J Urol. 2005;174:2291–6.
Costello AJ, Brooks M, Cole OJ. Anatomical studies of the neurovascular bundle and cavernosal nerves. BJU Int. 2004;94:1071–6.
Ganzer R, Stolzenburg JU, Neuhaus J, Weber F, Fuchshofer R, Burger M, et al. Anatomical study of pelvic nerves in relation to seminal vesicles, prostate and urethral sphincter: immunohistochemical staining, computerized planimetry and 3-dimensional reconstruction. J Urol. 2015;193:1205–12.
John H, Hauri D. Seminal vesicle-sparing radical prostatectomy: a novel concept to restore early urinary continence. Urology. 2000;55:820–4.
Albers P, Schäfers S, Löhmer H, de Geeter P. Seminal vesicle-sparing perineal radical prostatectomy improves early functional results in patients with low-risk prostate cancer. BJU Int. 2007;100:1050–4.
Thorstenson A, O’connor RC, Ahonen R, Jonsson MN, Wijkstrom H, Akre O, et al. Clinical outcome following prostatic capsule- and seminal-sparing cystectomy for bladder cancer in 25 men. Scand J Urol Nephrol. 2009;43:127–32.
McMahon CG, Abdo C, Incrocci L, Perelman M, Rowland D, Waldinger M, et al. Disorders of orgasm and ejaculation in men. J Sex Med. 2010;7:1668–86.
Kepper ME, Keast JR. Location, immunohistochemical features, and spinal connections of autonomic neurons innervating the rat seminal vesicles. Biol Reprod. 1997;57:1164–74.
Hsieh JT, Kuo YC, Chang HC, Liu SP, Chen JH, Tsai VF. The role of sympathetic and parasympathetic nerve systems on the smooth muscle of rat seminal vesicles - experimental results and speculation for physiological implication on ejaculation. Andrology. 2014;2:59–64.
Xin ZC, Chung WS, Choi YD, Seong DH, Choi YJ, Choi HK. Penile sensitivity in patients with primary premature ejaculation. J Urol. 1996;156:979–81.
Salem AM, Kamel II, Rashed LA, GamalEl Din SF. Effects of paroxetine on intravaginal ejaculatory latency time in Egyptian patients with lifelong premature ejaculation as a function of serotonin transporter polymorphism. Int J Impot Res. 2017;29:7–11.
Liu T, Jia C, Peng YF, Zhong W, Fang X. Correlation between premature ejaculation and psychological disorders in 270 Chinese outpatients. Psychiatry Res. 2019;272:69–72.
Screponi E, Carosa E, Di Stasi SM, Pepe M, Carruba G, Jannini EA. Prevalence of chronic prostatitis in men with premature ejaculation. Urology. 2001;58:198–202.
Carani C, Isidori AM, Granata A, Carosa E, Maggi M, Lenzi A, et al. Multicenter study on the prevalence of sexual symptoms in male hypo- and hyperthyroid patients. J Clin Endocrinol Metab. 2005;90:6472–9.
Yazici CM, Sarifakioglu B, Guzelant A, Turker P, Ates O. An unresolved discussion: presence of premature ejaculation and erectile dysfunction in lumbar disc hernia. Int Urol Nephrol. 2013;45:659–67.
Walden PD, Durkin MM, Lepor H, Wetzel JM, Gluchowski C, Gustafson EL. Localization of mRNA and receptor binding sites for the alpha 1a-adrenoceptor subtype in the rat, monkey and human urinary bladder and prostate. J Urol. 1997;157:1032–8.
Hisasue S, Furuya R, Itoh N, Kobayashi K, Furuya S, Tsukamoto T. Ejaculatory disorder caused by alpha-1 adrenoceptor antagonists is not retrograde ejaculation but a loss of seminal emission. Int J Urol. 2006;13:1311–6.
Hamamura M, Maróstica E, de Avellar MC, Porto CS. Muscarinic acetylcholine receptor subtypes in the rat seminal vesicle. Mol Cell Endocrinol. 2006;247:192–8.
Kedia K, Markland C. The effect of pharmacological agents on ejaculation. J Urol. 1975;114:569–73.
Hsieh JT, Chang HC, Law HS, Hsieh CH, Cheng JT. In vivo evaluation of serotonergic agents and alpha-adrenergic blockers on premature ejaculation by inhibiting the seminal vesicle pressure response to electrical nerve stimulation. Br J Urol. 1998;82:237–40.
Symonds T, Perelman MA, Althof S, Giuliano F, Martin M, May K, et al. Development and validation of a premature ejaculation diagnostic tool. Eur Urol. 2007;52:565–73.
Symonds T, Perelman M, Althof S, Giuliano F, Martin M, Abraham L, et al. Further evidence of the reliability and validity of the premature ejaculation diagnostic tool. Int J Impot Res. 2007;19:521–5.
Choi JH, Hwa JS, Kam SC, Jeh SU, Hyun JS. Effects of tamsulosin on premature ejaculation in men with benign prostatic hyperplasia. World J Mens Health. 2014;32:99–104.
Sato Y, Tanda H, Nakajima H, Nitta T, Akagashi K, Hanzawa T, et al. Silodosin and its potential for treating premature ejaculation: a preliminary report. Int J Urol. 2012;19:268–72.
Sato Y, Otani T, Amano T, Araki T, Kondou N, Matsukawa M, et al. Silodosin versus naftopidil in the treatment of premature ejaculation: a prospective multicenter trial. Int J Urol. 2017;24:626–31.
Waldinger MD, Olivier B. Utility of selective serotonin reuptake inhibitors in premature ejaculation. Curr Opin Investig Drugs. 2004;5:743–7.
Birowo P, Uckert S, Kedia GT, Scheller F, Meyer M, Taher A, et al. Evaluating the role of the serotoninergic system in the control of human seminal vesicle smooth muscle-an in vitro approach. J Sex Med. 2009;6:2672–9.
La Vignera S, Condorelli RA, Vicari E, Favilla V, Morgia G, Calogero AE. Acquired premature ejaculation and male accessory gland infection: relevance of ultrasound examination. Asian J Androl. 2016;18:769–72.
La Vignera S, Calogero AE, Arancio A, Castiglione R, De Grande G, Vicari E. Transrectal ultrasonography in infertile patients with persistently elevated bacteriospermia. Asian J Androl. 2008;10:731–40.
Kumar TR, Wiseman AL, Kala G, Kala SV, Matzuk MM, Lieberman MW. Reproductive defects in gamma-glutamyl transpeptidase-deficient mice. Endocrinology. 2000;141:4270–7.
Willem M, Miosge N, Halfter W, Smyth N, Jannetti I, Burghart E, et al. Specific ablation of the nidogen-binding site in the laminin gamma1 chain interferes with kidney and lung development. Development. 2002;129:2711–22.
Chen J. The pathophysiology of delayed ejaculation. Transl Androl Urol. 2016;5:549–62.
Abdel-Hamid IA, Ali OI. Delayed ejaculation: pathophysiology, diagnosis, and treatment. World J Mens Health. 2018;36:22–40.
Lindau ST, Tang H, Gomero A, Vable A, Huang ES, Drum ML, et al. Sexuality among middle-aged and older adults with diagnosed and undiagnosed diabetes: a national, population-based study. Diabetes Care. 2010;33:2202–10.
Shi GJ, Zheng J, Wu J, Qiao HQ, Chang Q, Niu Y, et al. Protective effects of Lycium barbarum polysaccharide on male sexual dysfunction and fertility impairments by activating hypothalamic pituitary gonadal axis in streptozotocin-induced type-1 diabetic male mice. Endocr J. 2017;64:907–22.
Li ZM, Liu N, Jiang YP, Yang JM, Zheng J, Sun M, et al. Vitexin alleviates streptozotocin-induced sexual dysfunction and fertility impairments in male mice via modulating the hypothalamus-pituitary-gonadal axis. Chem Biol Interact. 2019;297:119–29.
De A, Singh MF, Singh V, Ram V, Bisht S. Treatment effect of l-Norvaline on the sexual performance of male rats with streptozotocin induced diabetes. Eur J Pharmacol. 2016;771:247–54.
Pontes DA, Fernandes GS, Piffer RC, Gerardin DC, Pereira OC, Kempinas WG. Ejaculatory dysfunction in streptozotocin-induced diabetic rats: the role of testosterone. Pharmacol Rep. 2011;63:130–8.
Lert-Amornpat T, Maketon C, Fungfuang W. Effect of Kaempferia parviflora on sexual performance in streptozotocin-induced diabetic male rats. Andrologia. 2017;49: https://doi.org/10.1111/and.12770.
Morrison JF, Dhanasekaran S, Sheen R, Frampton CM, Mensah-Brown E. The effect of streptozotocin-induced diabetes on the rat seminal vesicle: a possible pathophysiological basis for disorders of ejaculation. Ann N Y Acad Sci. 2006;1084:267–79.
Yonezawa A, Ebiko M, Yoshizumi M, Ise SN, Watanabe C, Mizoguchi H, et al. Effects of insulin replacement on ejaculatory dysfunction in streptozotocin-induced diabetic rats. Int J Urol. 2009;16:208–11.
Tsounapi P, Honda M, Dimitriadis F, Kawamoto B, Hikita K, Muraoka K, et al. Impact of antioxidants on seminal vesicles function and fertilizing potential in diabetic rats. Asian J Androl. 2017;19:639–46.
La Vignera S, Condorelli RA, Di Mauro M, D’Agata R, Vicari E, Calogero AE. Seminal vesicles and diabetic neuropathy: ultrasound evaluation. J Androl. 2011;32:478–83.
Paduch DA, Polzer P, Morgentaler A, Althof S, Donatucci C, Ni X, et al. Clinical and demographic correlates of ejaculatory dysfunctions other than premature ejaculation: a prospective, observational study. J Sex Med. 2015;12:2276–86.
Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Premature and delayed ejaculation: two ends of a single continuum influenced by hormonal milieu. Int J Androl. 2011;34:41–8.
Corona G, Jannini EA, Lotti F, Boddi V, De Vita G, Forti G, et al. Different testosterone levels are associated with ejaculatory dysfunction. J Sex Med. 2008;5:1991–8.
Schmidt PJ, Steinberg EM, Negro PP, Haq N, Gibson C, Rubinow DR. Pharmacologically induced hypogonadism and sexual function in healthy young women and men. Neuropsychopharmacology. 2009;34:565–76.
Apfelbaum B. Retarded ejaculation: a much-misunderstood syndrome. In: Leiblum SR, Rosen RC, editors. Principles and practice of sex therapy: update for the 1990’s. New York: The Guildford Press; 1989. p. 168–206.
Shin DH, Spitz A. The evaluation and treatment of delayed ejaculation. Sex Med Rev. 2014;2:121–33.
Jin BF, Zhang HJ, Zhang XD, Sun DL, Gao YJ, Xia GS, et al. Yangjing capsule plus low-dose tadalafil for functional anejaculation. Zhonghua Nan Ke Xue. 2012;18:1140–2.
Sun D, Cui Y, Jin B, Zhang X, Yang X, Gao C. Effects of the Yangjing capsule extract on steroidogenesis and apoptosis in mouse leydig cells. Evid Based Complement Alternat Med. 2012;2012:985457.
Jin BF, Xue YY, Zhang XD, Xia GS, Sun DL. Effects of Yangjing capsule on the ultrastructure of seminal vesicles in aged rats. Zhonghua Nan Ke Xue. 2014;20:68–72.
Rago R, Salacone P, Caponecchia L, Marcucci I, Fiori C, Sebastianelli A. Effect of vardenafil on semen parameters in infertile men: a pilot study evaluating short-term treatment. J Endocrinol Invest. 2012;35:897–900.
Perelman MA. Men with ED also report changes in orgasmic sensations. J Androl. 2011;32:340–2.
Jenkins LC, Mulhall JP. Delayed orgasm and anorgasmia. Fertil Steril. 2015;104:1082–8.
Alwaal A, Breyer BN, Lue TF. Normal male sexual function: emphasis on orgasm and ejaculation. Fertil Steril. 2015;104:1051–60.
Otani T. Clinical review of ejaculatory dysfunction. Reprod Med Biol. 2019;18:331–43.
Van der Schoot DK, Ypma AF. Seminal vesiculectomy to resolve defecation-induced orgasm. BJU Int. 2002;90:761–2.
Jin BF, Huang YF, Lu XH. Clinical observation of the treatment of male sexual dysfunction by yangjingjiaonang. Zhonghua Nan Ke Xue. 2006;12:272–6.
Tong YC, Hung YC, Lin SN, Cheng JT. Treatment effect of “ryu-wei-ti-huang-wan” (a Chinese herbal prescription) on the sexual performance of male rats with streptozotocin-induced diabetes. Urol Int. 1996;57:230–4.
Angelini L, Castagnetti M, Rigamonti W. Painful orgasm in an adolescent after seminal-sparing cystoprostatectomy: a puzzling symptom. Urol Int. 2015;94:366–8.
Acknowledgements
The figure used in this study was created with the support of FigDraw (https://www.figdraw.com).
Funding
This work was supported by the National Natural Science Foundation of China (No. 82074440) and Zhongda Hospital, Southeast University, Jiangsu Province High-Level Hospital Construction Funds (2024GSPKY26).
Author information
Authors and Affiliations
Contributions
DG was responsible for writing the manuscript. CL and YJ participated in the literature screening. DS designed the structure of the article and assisted in manuscript preparation. YC and WC provided revisions to the manuscript. BJ contributed the research topic.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, D., Li, C., Jin, Y. et al. Seminal vesicles - an overlooked pair of accessory glands in male sexual dysfunction: a narrative review. Int J Impot Res (2024). https://doi.org/10.1038/s41443-024-01011-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-024-01011-4