Abstract
Small-cell lung cancer (SCLC) is a highly aggressive malignancy with poor prognosis. For decades, etoposide–platinum-based chemotherapy had been the mainstay treatment for SCLC; however, despite initial high response rates, most patients developed resistance. In 2019, the US Food and Drug Administration approved the anti-PD-L1 antibody atezolizumab in combination with etoposide–platinum as the new first-line standard of care for extensive-stage SCLC, heralding a paradigm shift in SCLC therapy. This Review aims to provide an overview of the current landscape and emerging treatment strategies of immunotherapies in SCLC as well as highlight the importance of developing biomarkers to facilitate patient selection.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Gazdar, A. F., Bunn, P. A. & Minna, J. D. Small-cell lung cancer: what we know, what we need to know and the path forward. Nat. Rev. Cancer 17, 765 (2017).
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33 (2022).
Dowlati, A. et al. Immune checkpoint blockade outcome in small-cell lung cancer and its relationship with retinoblastoma mutation status and function. JCO Precis. Oncol. 6, e2200257 (2022).
Sivakumar, S. et al. Integrative analysis of a large real-world cohort of small cell lung cancer identifies distinct genetic subtypes and insights into histologic transformation. Cancer Discov. 13, 1572–1591 (2023).
Wildey, G. et al. Retinoblastoma expression and targeting by CDK4/6 inhibitors in small cell lung cancer. Mol. Cancer Ther. 22, 264–273 (2023).
George, J. et al. Comprehensive genomic profiles of small cell lung cancer. Nature 524, 47–53 (2015).
Khuder, S. A. Effect of cigarette smoking on major histological types of lung cancer: a meta-analysis. Lung Cancer 31, 139–148 (2001).
Sun, J. M. et al. Small-cell lung cancer detection in never-smokers: clinical characteristics and multigene mutation profiling using targeted next-generation sequencing. Ann. Oncol. 26, 161–166 (2015).
Cho, J. et al. Proportion and clinical features of never-smokers with non-small cell lung cancer. Chin. J. Cancer 36, 20 (2017).
Liu, X. et al. Characterization of never-smoking and its association with clinical outcomes in Chinese patients with small-cell lung cancer. Lung Cancer 115, 109–115 (2018).
Torres-Duran, M. et al. Small-cell lung cancer in never-smokers. ESMO Open 6, 100059 (2021).
Rodriguez-Martinez, A., Torres-Duran, M., Barros-Dios, J. M. & Ruano-Ravina, A. Residential radon and small cell lung cancer. A systematic review. Cancer Lett. 426, 57–62 (2018).
Kim, C. H. et al. Exposure to secondhand tobacco smoke and lung cancer by histological type: a pooled analysis of the International Lung Cancer Consortium (ILCCO). Int. J. Cancer 135, 1918–1930 (2014).
Yu, H. A. et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin. Cancer Res. 19, 2240–2247 (2013).
Balla, A., Khan, F., Hampel, K. J., Aisner, D. L. & Sidiropoulos, N. Small-cell transformation of ALK-rearranged non-small-cell adenocarcinoma of the lung. Cold Spring Harb. Mol. Case Stud. 4, a002394 (2018).
Ou, S. I. et al. Dual occurrence of ALK G1202R solvent front mutation and small cell lung cancer transformation as resistance mechanisms to second generation ALK inhibitors without prior exposure to crizotinib. Pitfall of solely relying on liquid re-biopsy? Lung Cancer 106, 110–114 (2017).
Cha, Y. J., Cho, B. C., Kim, H. R., Lee, H. J. & Shim, H. S. A case of ALK-rearranged adenocarcinoma with small cell carcinoma-like transformation and resistance to crizotinib. J. Thorac. Oncol. 11, e55–e58 (2016).
Takegawa, N. et al. Transformation of ALK rearrangement-positive adenocarcinoma to small-cell lung cancer in association with acquired resistance to alectinib. Ann. Oncol. 27, 953–955 (2016).
Fujita, S., Masago, K., Katakami, N. & Yatabe, Y. Transformation to SCLC after treatment with the ALK inhibitor alectinib. J. Thorac. Oncol. 11, e67–e72 (2016).
Miyamoto, S. et al. Transformation to small-cell lung cancer as a mechanism of acquired resistance to crizotinib and alectinib. Jpn. J. Clin. Oncol. 46, 170–173 (2016).
Lin, J. J. et al. Small cell transformation of ROS1 fusion-positive lung cancer resistant to ROS1 inhibition. NPJ Precis. Oncol. 4, 21 (2020).
Liu, Y. Small cell lung cancer transformation from EGFR-mutated lung adenocarcinoma: a case report and literatures review. Cancer Biol. Ther. 19, 445–449 (2018).
Yamagata, A., Yokoyama, T., Fukuda, Y. & Ishida, T. Alectinib re-challenge in small cell lung cancer transformation after chemotherapy failure in a patient with ALK-positive lung cancer: a case report. Respir. Med. Case Rep. 33, 101440 (2021).
Shen, Q., Qu, J., Sheng, L., Gao, Q. & Zhou, J. Case report: transformation from non-small cell lung cancer to small cell lung cancer during anti-PD-1 therapy: a report of two cases. Front. Oncol. 11, 619371 (2021).
Imakita, T., Fujita, K., Kanai, O., Terashima, T. & Mio, T. Small cell lung cancer transformation during immunotherapy with nivolumab: a case report. Respir. Med. Case Rep. 21, 52–55 (2017).
Sehgal, K. et al. Small cell transformation of non-small cell lung cancer on immune checkpoint inhibitors: uncommon or under-recognized? J. Immunother. Cancer 8, e000697 (2020).
Fruh, M. et al. Small-cell lung cancer (SCLC): ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 24, vi99–vi105 (2013).
Rudin, C. M., Giaccone, G. & Ismaila, N. Treatment of small-cell lung cancer: American Society of Clinical Oncology endorsement of the American College of Chest Physicians guideline. J. Oncol. Pract. 12, 83–86 (2016).
Cheng, Y. et al. Durvalumab after chemoradiotherapy in limited-stage small-cell lung cancer. N. Engl. J. Med. 391, 1313–1327 (2024).
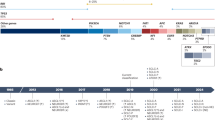
Horn, L. et al. First-line atezolizumab plus chemotherapy in extensive-stage small-cell lung cancer. N. Engl. J. Med. 379, 2220–2229 (2018).
Paz-Ares, L. et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): a randomised, controlled, open-label, phase 3 trial. Lancet 394, 1929–1939 (2019).
von Pawel, J. et al. Topotecan versus cyclophosphamide, doxorubicin, and vincristine for the treatment of recurrent small-cell lung cancer. J. Clin. Oncol. 17, 658–667 (1999).
Pardoll, D. M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer 12, 252–264 (2012).
Ribas, A. & Wolchok, J. D. Cancer immunotherapy using checkpoint blockade. Science 359, 1350–1355 (2018).
Ma, Y. et al. Anticancer chemotherapy-induced intratumoral recruitment and differentiation of antigen-presenting cells. Immunity 38, 729–741 (2013).
Emens, L. A. & Middleton, G. The interplay of immunotherapy and chemotherapy: harnessing potential synergies. Cancer Immunol. Res. 3, 436–443 (2015).
Sordo-Bahamonde, C. et al. Chemo-immunotherapy: a new trend in cancer treatment. Cancers 15, 2912 (2023).
Liu, S. V. et al. Updated overall survival and PD-L1 subgroup analysis of patients with extensive-stage small-cell lung cancer treated with atezolizumab, carboplatin, and etoposide (IMpower133). J. Clin. Oncol. 39, 619–630 (2021).
Hellmann, M. D. et al. Tumor mutational burden and efficacy of nivolumab monotherapy and in combination with ipilimumab in small-cell lung cancer. Cancer Cell 35, 329 (2019).
Paz-Ares, L. et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer: 3-year overall survival update from CASPIAN. ESMO Open 7, 100408 (2022).
Paz-Ares, L. et al. LBA89 - PD-L1 expression, patterns of progression and patient-reported outcomes (PROs) with durvalumab plus platinum-etoposide in ES-SCLC: results from CASPIAN. Ann. Oncol. 30, v928–v929 (2019).
Wang, J. et al. Adebrelimab or placebo plus carboplatin and etoposide as first-line treatment for extensive-stage small-cell lung cancer (CAPSTONE-1): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 23, 739–747 (2022).
Cheng, Y. et al. Effect of first-line serplulimab vs placebo added to chemotherapy on survival in patients with extensive-stage small cell lung cancer: the ASTRUM-005 randomized clinical trial. JAMA 328, 1223–1232 (2022).
Rudin, C. M. et al. Pembrolizumab or placebo plus etoposide and platinum as first-line therapy for extensive-stage small-cell lung cancer: randomized, double-blind, phase III KEYNOTE-604 study. J. Clin. Oncol. 38, 2369–2379 (2020).
Spigel, D. R. et al. Second-line nivolumab in relapsed small-cell lung cancer: CheckMate 331. Ann. Oncol. 32, 631–641 (2021).
Cheng, Y. et al. LBA9 Updated results of first-line serplulimab versus placebo combined with chemotherapy in extensive-stage small cell lung cancer: An international multicentre phase III study (ASTRUM-005). Ann. Oncol. 33, S1562 (2022).
Cheng, Y. et al. Tislelizumab plus platinum and etoposide versus placebo plus platinum and etoposide as first-line treatment for extensive-stage SCLC (RATIONALE-312): a multicenter, double-blind, placebo-controlled, randomized, phase 3 clinical trial. J. Thorac. Oncol. 19, 1073–1085 (2024).
Cheng, Y. et al. Toripalimab plus chemotherapy as a first-line therapy for extensive-stage small cell lung cancer: the phase 3 EXTENTORCH randomized clinical trial. JAMA Oncol. 11, 16–25 (2025).
Issafras, H. et al. Structural basis of HLX10 PD-1 receptor recognition, a promising anti-PD-1 antibody clinical candidate for cancer immunotherapy. PLoS ONE 16, e0257972 (2021).
Reck, M. et al. Ipilimumab in combination with paclitaxel and carboplatin as first-line therapy in extensive-disease-small-cell lung cancer: results from a randomized, double-blind, multicenter phase 2 trial. Ann. Oncol. 24, 75–83 (2013).
Reck, M. et al. Phase III randomized trial of ipilimumab plus etoposide and platinum versus placebo plus etoposide and platinum in extensive-stage small-cell lung cancer. J. Clin. Oncol. 34, 3740–3748 (2016).
Goldman, J. W. et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide versus platinum-etoposide alone in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): updated results from a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 22, 51–65 (2021).
Rudin, C. M. et al. SKYSCRAPER-02: tiragolumab in combination with atezolizumab plus chemotherapy in untreated extensive-stage small-cell lung cancer. J. Clin. Oncol. 42, 324–335 (2024).
Sands, J. et al. 1463 Coformulated vibostolimab/pembrolizumab plus chemotherapy as first-line therapy vs atezolizumab plus chemotherapy for extensive-stage small-cell lung cancer (ES-SCLC): randomized, phase 3 KEYVIBE-008. J. Immunother. Cancer 12, A1693–A1694 (2024).
Zitvogel, L., Kepp, O. & Kroemer, G. Immune parameters affecting the efficacy of chemotherapeutic regimens. Nat. Rev. Clin. Oncol. 8, 151–160 (2011).
van der Most, R. G. et al. Tumor eradication after cyclophosphamide depends on concurrent depletion of regulatory T cells: a role for cycling TNFR2-expressing effector-suppressor T cells in limiting effective chemotherapy. Cancer Immunol. Immunother. 58, 1219–1228 (2009).
Gadgeel, S. M. et al. Phase II study of maintenance pembrolizumab in patients with extensive-stage small cell lung cancer (SCLC). J. Thorac. Oncol. 13, 1393–1399 (2018).
Owonikoko, T. K. et al. Nivolumab and ipilimumab as maintenance therapy in extensive-disease small-cell lung cancer: CheckMate 451. J. Clin. Oncol. 39, 1349–1359 (2021).
Bhavnani, K. Jazz Pharmaceuticals announces statistically significant overall survival and progression-free survival results for Zepzelca® (lurbinectedin) and atezolizumab combination in first-line maintenance therapy for extensive-stage small cell lung cancer. PR Newswire (15 October 2024).
Pignon, J. P. et al. A meta-analysis of thoracic radiotherapy for small-cell lung cancer. N. Engl. J. Med. 327, 1618–1624 (1992).
Warde, P. & Payne, D. Does thoracic irradiation improve survival and local control in limited-stage small-cell carcinoma of the lung? A meta-analysis. J. Clin. Oncol. 10, 890–895 (1992).
Murray, N. et al. Importance of timing for thoracic irradiation in the combined modality treatment of limited-stage small-cell lung cancer. The National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 11, 336–344 (1993).
Turrisi, A. T. 3rd & Glover, D. J. Thoracic radiotherapy variables: influence on local control in small cell lung cancer limited disease. Int. J. Radiat. Oncol. Biol. Phys. 19, 1473–1479 (1990).
McCracken, J. D. et al. Concurrent chemotherapy/radiotherapy for limited small-cell lung carcinoma: a Southwest Oncology Group Study. J. Clin. Oncol. 8, 892–898 (1990).
Takada, M. et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with cisplatin and etoposide for limited-stage small-cell lung cancer: results of the Japan Clinical Oncology Group Study 9104. J. Clin. Oncol. 20, 3054–3060 (2002).
Johnson, B. E. et al. Patients with limited-stage small-cell lung cancer treated with concurrent twice-daily chest radiotherapy and etoposide/cisplatin followed by cyclophosphamide, doxorubicin, and vincristine. J. Clin. Oncol. 14, 806–813 (1996).
Peters, S. et al. Consolidation nivolumab and ipilimumab versus observation in limited-disease small-cell lung cancer after chemo-radiotherapy – results from the randomised phase II ETOP/IFCT 4-12 STIMULI trial. Ann. Oncol. 33, 67–79 (2022).
Gong, Y. et al. Abstract CT255: AdvanTIG-204: A phase 2, multicenter, randomized, 3-arm, open-label study investigating the preliminary efficacy and safety of ociperlimab (anti-TIGIT) + tislelizumab (anti-PD-1) + concurrent chemoradiotherapy (cCRT) in patients with untreated limited-stage small cell lung cancer (SCLC). Cancer Res. 84, CT255 (2024).
Higgins, K. et al. Concurrent chemoradiation ± atezolizumab (atezo) in limited-stage small cell lung cancer (LS-SCLC): results of NRG Oncology/Alliance LU005. Int. J. Radiat. Oncol. Biol. Phys. 120, S2 (2024).
Rosenthal, R. et al. Neoantigen-directed immune escape in lung cancer evolution. Nature 567, 479–485 (2019).
Marty Pyke, R. et al. Evolutionary pressure against MHC class II binding cancer mutations. Cell 175, 416–428.e413 (2018).
Dejima, H. et al. Immune evolution from preneoplasia to invasive lung adenocarcinomas and underlying molecular features. Nat. Commun. 12, 2722 (2021).
Hu, X. et al. Evolution of DNA methylome from precancerous lesions to invasive lung adenocarcinomas. Nat. Commun. 12, 687 (2021).
von Pawel, J. et al. Randomized phase III trial of amrubicin versus topotecan as second-line treatment for patients with small-cell lung cancer. J. Clin. Oncol. 32, 4012–4019 (2014).
Trigo, J. et al. Lurbinectedin as second-line treatment for patients with small-cell lung cancer: a single-arm, open-label, phase 2 basket trial. Lancet Oncol. 21, 645–654 (2020).
Antonia, S. J. et al. Nivolumab alone and nivolumab plus ipilimumab in recurrent small-cell lung cancer (CheckMate 032): a multicentre, open-label, phase 1/2 trial. Lancet Oncol. 17, 883–895 (2016).
Ready, N. E. et al. Nivolumab monotherapy and nivolumab plus ipilimumab in recurrent small cell lung cancer: results from the CheckMate 032 randomized cohort. J. Thorac. Oncol. 15, 426–435 (2020).
Ott, P. A. et al. Pembrolizumab in patients with extensive-stage small-cell lung cancer: results from the phase Ib KEYNOTE-028 study. J. Clin. Oncol. 35, 3823–3829 (2017).
Chung, H. C. et al. Phase 2 study of pembrolizumab in advanced small-cell lung cancer (SCLC): KEYNOTE-158. J. Clin. Oncol. 36, 8506 (2018).
Chung, H. C. et al. Pembrolizumab after two or more lines of previous therapy in patients with recurrent or metastatic SCLC: results from the KEYNOTE-028 and KEYNOTE-158 studies. J. Thorac. Oncol. 15, 618–627 (2020).
Reinmuth, N. et al. Novel combinations of immunotherapies or DNA damage repair inhibitors in platinum-refractory extensive-stage small cell lung cancer: the phase II BALTIC study. Clin. Cancer Res. 30, 4055–4067 (2024).
Navarro, A. et al. Abstract CT256: Results from KEYNOTE-B98: a phase 1b/2 study of pembrolizumab plus investigational agents in patients with anti-PD-(L)1-refractory extensive-stage small-cell lung cancer (ES-SCLC). Cancer Res. 84, CT256 (2024).
Haen, S. P., Loffler, M. W., Rammensee, H. G. & Brossart, P. Towards new horizons: characterization, classification and implications of the tumour antigenic repertoire. Nat. Rev. Clin. Oncol. 17, 595–610 (2020).
Lin, M. J. et al. Cancer vaccines: the next immunotherapy frontier. Nat. Cancer 3, 911–926 (2022).
Krug, L. M. et al. Immunization with N-propionyl polysialic acid-KLH conjugate in patients with small cell lung cancer is safe and induces IgM antibodies reactive with SCLC cells and bactericidal against group B meningococci. Cancer Immunol. Immunother. 61, 9–18 (2012).
Giaccone, G. et al. Phase III study of adjuvant vaccination with Bec2/bacille Calmette-Guerin in responding patients with limited-disease small-cell lung cancer (European Organisation for Research and Treatment of Cancer 08971-08971B; Silva Study). J. Clin. Oncol. 23, 6854–6864 (2005).
Chiappori, A. A. et al. Randomized-controlled phase II trial of salvage chemotherapy after immunization with a TP53-transfected dendritic cell-based vaccine (Ad.p53-DC) in patients with recurrent small cell lung cancer. Cancer Immunol. Immunother. 68, 517–527 (2019).
Sabari, J. K., Lok, B. H., Laird, J. H., Poirier, J. T. & Rudin, C. M. Unravelling the biology of SCLC: implications for therapy. Nat. Rev. Clin. Oncol. 14, 549–561 (2017).
Byers, L. et al. 697 A phase 1 study of AMG 119, a DLL3-targeting, chimeric antigen receptor (CAR) T cell therapy, in relapsed/refractory small cell lung cancer (SCLC). J. Immunother. Cancer 10, A728 (2022).
Huehls, A. M., Coupet, T. A. & Sentman, C. L. Bispecific T-cell engagers for cancer immunotherapy. Immunol. Cell Biol. 93, 290–296 (2015).
Paz-Ares, L. et al. Tarlatamab, a first-in-class DLL3-targeted bispecific T-Cell Engager, in recurrent small-cell lung cancer: an open-label, phase I study. J. Clin. Oncol. 41, 2893–2903 (2023).
Ahn, M. J. et al. Tarlatamab for patients with previously treated small-cell lung cancer. N. Engl. J. Med. 389, 2063–2075 (2023).
Wermke, M. et al. First-in-human dose-escalation trial of BI 764532, a delta-like ligand 3 (DLL3)/CD3 IgG-like T-cell engager in patients (pts) with DLL3-positive (DLL3+) small-cell lung cancer (SCLC) and neuroendocrine carcinoma (NEC). J. Clin. Oncol. 41, 8502–8502 (2023).
Beltran, H. et al. Updated results from a phase 1/2 study of HPN328, a tri-specific, half-life (T1/2) extended DLL3-targeting T-cell engager in patients (pts) with small cell lung cancer (SCLC) and other neuroendocrine cancers (NEC). J. Clin. Oncol. 42, 8090 (2024).
Clamon, G. et al. Interleukin-2 activity in patients with extensive small-cell lung cancer: a phase II trial of cancer and leukemia group B. J. Natl Cancer Inst. 85, 316–320 (1993).
Clamon, G., Herndon, J., Akerley, W. & Green, M. Subcutaneous interleukin-2 as initial therapy for patients with extensive small cell lung cancer:: a phase II trial of cancer and leukemia group B. Lung Cancer 19, 25–29 (1998).
Zarogoulidis, K. et al. Interferon α-2a and combined chemotherapy as first line treatment in SCLC patients: a randomized trial. Lung Cancer 15, 197–205 (1996).
Zarogoulidis, K. et al. Immunomodifiers in combination with conventional chemotherapy in small cell lung cancer: a phase II, randomized study. Drug Des. Devel. Ther. 7, 611–617 (2013).
Mattson, K. et al. Natural interferon alfa as maintenance therapy for small cell lung cancer. Eur. J. Cancer 28a, 1387–1391 (1992).
Jett, J. R. et al. Phase III trial of recombinant interferon γ in complete responders with small-cell lung cancer. J. Clin. Oncol. 12, 2321–2326 (1994).
Kelly, K. et al. Role of recombinant interferon alfa-2a maintenance in patients with limited-stage small-cell lung cancer responding to concurrent chemoradiation: a Southwest Oncology Group study. J. Clin. Oncol. 13, 2924–2930 (1995).
van Zandwijk, N. et al. Role of recombinant interferon-γ maintenance in responding patients with small cell lung cancer. A randomised phase III study of the EORTC Lung Cancer Cooperative Group. Eur. J. Cancer 33, 1759–1766 (1997).
Pillai, R. N. et al. Interferon α plus 13-cis-retinoic acid modulation of BCL-2 plus paclitaxel for recurrent small-cell lung cancer (SCLC): an Eastern Cooperative Oncology Group study (E6501). Cancer Chemother. Pharmacol. 74, 177–183 (2014).
Thomas, M. et al. Immunotherapeutic maintenance treatment with toll-like receptor 9 agonist lefitolimod in patients with extensive-stage small-cell lung cancer: results from the exploratory, controlled, randomized, international phase II IMPULSE study. Ann. Oncol. 29, 2076–2084 (2018).
Fu, Z., Li, S., Han, S., Shi, C. & Zhang, Y. Antibody drug conjugate: the “biological missile” for targeted cancer therapy. Signal Transduct. Target Ther. 7, 93 (2022).
Vitorino, P. et al. Rova-T enhances the anti-tumor activity of anti-PD1 in a murine model of small cell lung cancer with endogenous Dll3 expression. Transl. Oncol. 14, 100883 (2021).
Chapoval, A. I. et al. B7-H3: a costimulatory molecule for T cell activation and IFN-γ production. Nat. Immunol. 2, 269–274 (2001).
Luo, L. et al. B7-H3 enhances tumor immunity in vivo by costimulating rapid clonal expansion of antigen-specific CD8+ cytolytic T cells. J. Immunol. 173, 5445–5450 (2004).
Zhou, W. T. & Jin, W. L. B7-H3/CD276: an emerging cancer immunotherapy. Front. Immunol. 12, 701006 (2021).
Lee, Y. H. et al. Inhibition of the B7-H3 immune checkpoint limits tumor growth by enhancing cytotoxic lymphocyte function. Cell Res. 27, 1034–1045 (2017).
Scribner, J. A. et al. Preclinical development of MGC018, a duocarmycin-based antibody-drug conjugate targeting B7-H3 for solid cancer. Mol. Cancer Ther. 19, 2235–2244 (2020).
Metrangolo, V. & Engelholm, L. H. Antibody–drug conjugates: the dynamic evolution from conventional to next-generation constructs. Cancers 16, 447 (2024).
Wang, W., Erbe, A. K., Hank, J. A., Morris, Z. S. & Sondel, P. M. NK cell-mediated antibody-dependent cellular cytotoxicity in cancer immunotherapy. Front. Immunol. 6, 368 (2015).
Hubert, P. et al. Antibody-dependent cell cytotoxicity synapses form in mice during tumor-specific antibody immunotherapy. Cancer Res. 71, 5134–5143 (2011).
Zahavi, D., AlDeghaither, D., O’Connell, A. & Weiner, L. M. Enhancing antibody-dependent cell-mediated cytotoxicity: a strategy for improving antibody-based immunotherapy. Antib. Ther. 1, 7–12 (2018).
Blackhall, F. et al. Efficacy and safety of rovalpituzumab tesirine compared with topotecan as second-line therapy in DLL3-High SCLC: results from the phase 3 TAHOE study. J. Thorac. Oncol. 16, 1547–1558 (2021).
Johnson, M. L. et al. Rovalpituzumab tesirine as a maintenance therapy after first-line platinum-based chemotherapy in patients with extensive-stage SCLC: results from the phase 3 MERU study. J. Thorac. Oncol. 16, 1570–1581 (2021).
Kahl, B. S. et al. A phase I study of ADCT-402 (loncastuximab tesirine), a novel pyrrolobenzodiazepine-based antibody-drug conjugate, in relapsed/refractory B-cell non-Hodgkin lymphoma. Clin. Cancer Res. 25, 6986–6994 (2019).
Stein, E. M. et al. A phase 1 trial of vadastuximab talirine as monotherapy in patients with CD33-positive acute myeloid leukemia. Blood 131, 387–396 (2018).
Phillips, T. et al. A phase 1 trial of SGN-CD70A in patients with CD70-positive diffuse large B cell lymphoma and mantle cell lymphoma. Invest. New Drugs 37, 297–306 (2019).
Bardia, A. et al. Sacituzumab govitecan, a Trop-2-directed antibody-drug conjugate, for patients with epithelial cancer: final safety and efficacy results from the phase I/II IMMU-132-01 basket trial. Ann. Oncol. 32, 746–756 (2021).
Gray, J. E. et al. Therapy of small cell lung cancer (SCLC) with a topoisomerase-I-inhibiting antibody-drug conjugate (ADC) targeting Trop-2, sacituzumab govitecan. Clin. Cancer Res. 23, 5711–5719 (2017).
Johnson, M. et al. OA05.05 Ifinatamab deruxtecan (I-DXd; DS-7300) in patients with refractory SCLC: a subgroup analysis of a phase 1/2 study. J. Thorac. Oncol. 18, S54–S55 (2023).
Bhowmick, S. J. AbbVie showcases robust solid tumor pipeline at ASCO 2024 with new data from its innovative antibody–drug conjugate (ADC) platform AbbVie News Center (28 May 2024).
Chandana, S. R. et al. First-in-human study of ABBV-706, a seizure-related homolog protein 6 (SEZ6) targeting antibody–drug conjugate (ADC), in patients (pts) with advanced solid tumors. J. Clin. Oncol. 42, 3001 (2024).
Chu, Q. et al. BMS-986012, an anti-fucosyl-GM1 monoclonal antibody as monotherapy or in combination with nivolumab in relapsed/refractory SCLC: results from a first-in-human phase 1/2 study. JTO Clin. Res. Rep. 3, 100400 (2022).
Wei, J., Li, W., Zhang, P., Guo, F. & Liu, M. Current trends in sensitizing immune checkpoint inhibitors for cancer treatment. Mol. Cancer 23, 279 (2024).
Krebs, M. G. et al. Olaparib and durvalumab in patients with relapsed small cell lung cancer (MEDIOLA): an open-label, multicenter, phase 1/2, basket study. Lung Cancer 180, 107216 (2023).
Gandara, D. R. et al. Blood-based tumor mutational burden as a predictor of clinical benefit in non-small-cell lung cancer patients treated with atezolizumab. Nat. Med. 24, 1441–1448 (2018).
Peters, S. et al. Atezolizumab versus chemotherapy in advanced or metastatic NSCLC with high blood-based tumor mutational burden: primary analysis of BFAST cohort C randomized phase 3 trial. Nat. Med. 28, 1831–1839 (2022).
Chen, M. et al. Cold and heterogeneous T cell repertoire is associated with copy number aberrations and loss of immune genes in small-cell lung cancer. Nat. Commun. 12, 6655 (2021).
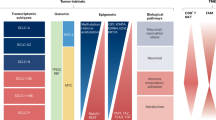
Rudin, C. M. et al. Molecular subtypes of small cell lung cancer: a synthesis of human and mouse model data. Nat. Rev. Cancer 19, 289–297 (2019).
Gay, C. M. et al. Patterns of transcription factor programs and immune pathway activation define four major subtypes of SCLC with distinct therapeutic vulnerabilities. Cancer Cell 39, 346–360.e347 (2021).
Xie, M. et al. Abstract CT024: Durvalumab (D) + platinum-etoposide (EP) in 1L extensive-stage small-cell lung cancer (ES-SCLC): exploratory analysis of SCLC molecular subtypes in CASPIAN. Cancer Res. 82, CT024 (2022).
Nabet, B. Y. et al. Immune heterogeneity in small-cell lung cancer and vulnerability to immune checkpoint blockade. Cancer Cell 42, 429–443.e424 (2024).
Busch, S. E. et al. Lung cancer subtypes generate unique immune responses. J. Immunol. 197, 4493–4503 (2016).
Wang, H. et al. Prognostic significance of PD-L1 expression and CD8+ T cell infiltration in pulmonary neuroendocrine tumors. Diagn. Pathol. 13, 30 (2018).
Chen, D. S. & Mellman, I. Oncology meets immunology: the cancer-immunity cycle. Immunity 39, 1–10 (2013).
Kalari, S., Jung, M., Kernstine, K. H., Takahashi, T. & Pfeifer, G. P. The DNA methylation landscape of small cell lung cancer suggests a differentiation defect of neuroendocrine cells. Oncogene 32, 3559–3568 (2013).
Nguyen, E. M. et al. Targeting lysine-specific demethylase 1 rescues major histocompatibility complex class I antigen presentation and overcomes programmed death-ligand 1 blockade resistance in SCLC. J. Thorac. Oncol. 17, 1014–1031 (2022).
Zheng, Y., Wang, Z., Wei, S., Liu, Z. & Chen, G. Epigenetic silencing of chemokine CCL2 represses macrophage infiltration to potentiate tumor development in small cell lung cancer. Cancer Lett. 499, 148–163 (2021).
Peng, D. et al. Epigenetic silencing of TH1-type chemokines shapes tumour immunity and immunotherapy. Nature 527, 249–253 (2015).
Arner, E. N. & Rathmell, J. C. Metabolic programming and immune suppression in the tumor microenvironment. Cancer Cell 41, 421–433 (2023).
Ricci, J.-E. Tumor-induced metabolic immunosuppression: mechanisms and therapeutic targets. Cell Rep. 44, 115206 (2025).
Elia, I. & Haigis, M. C. Metabolites and the tumour microenvironment: from cellular mechanisms to systemic metabolism. Nat. Metab. 3, 21–32 (2021).
Chiu, D. K. C. et al. Hypoxia induces myeloid‐derived suppressor cell recruitment to hepatocellular carcinoma through chemokine (C‐C motif) ligand 26. Hepatology 64, 797–813 (2016).
Liu, B. & Wei, C. Hypoxia Induces overexpression of CCL28 to recruit Treg cells to enhance angiogenesis in lung adenocarcinoma. J. Environ. Pathol. Toxicol. Oncol. 40, 65–74 (2021).
Watson, M. J. et al. Metabolic support of tumour-infiltrating regulatory T cells by lactic acid. Nature 591, 645–651 (2021).
Nishiga, Y. et al. Radiotherapy in combination with CD47 blockade elicits a macrophage-mediated abscopal effect. Nat. Cancer 3, 1351–1366 (2022).
Zhang, H. et al. CDK7 inhibition potentiates genome instability triggering anti-tumor immunity in small cell lung cancer. Cancer Cell 37, 37–54.e39 (2020).
Oser, M. G., MacPherson, D., Oliver, T. G., Sage, J. & Park, K. S. Genetically-engineered mouse models of small cell lung cancer: the next generation. Oncogene 43, 457–469 (2024).
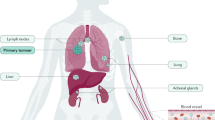
Qu, F. et al. Crosstalk between small-cell lung cancer cells and astrocytes mimics brain development to promote brain metastasis. Nat. Cell Biol. 25, 1506–1519 (2023).
Hiatt, J. B. et al. Inhibition of LSD1 with bomedemstat sensitizes small cell lung cancer to immune checkpoint blockade and T-cell killing. Clin. Cancer Res. 28, 4551–4564 (2022).
Sattler, M. & Salgia, R. LSD1-targeted therapy-a multi-purpose key to unlock immunotherapy in small cell lung cancer. Transl. Lung Cancer Res. 12, 1350–1354 (2023).
Hu, H. et al. Current status in rechallenge of immunotherapy. Int. J. Biol. Sci. 19, 2428–2442 (2023).
Welsh, J. W. et al. Phase I trial of pembrolizumab and radiation therapy after induction chemotherapy for extensive-stage small cell lung cancer. J. Thorac. Oncol. 15, 266–273 (2020).
Acknowledgements
The work of the authors is supported by a Barbanti Small Cell Lung Cancer Award, University of Texas MD Anderson Physician Scientist Award, University Cancer Foundation Sister Institution Network Fund, National Institutes of Health (NIH)/NCI U01-CA213273, NIH/NCI U01-CA256780-01, the LUNGevity Foundation, Rexanna’s Foundation for Fighting Lung Cancer, the Andrew Sabin Family Foundation, Cancer Prevention Research Institute of Texas, the University of Texas MD Anderson Lung Cancer Moon Shot Program, The University of Texas Lung SPORE Program, the University of Texas MD Anderson Lung Cancer Genomics Program, the University of Texas MD Anderson Lung Cancer Interception Program, and the generous support from the Andrea Mugnaini and Edward LC Smith Fund. We thank C. Hu, Z. H. Kwok and J. Li from Helius for their support during preparation of this Review.
Author information
Authors and Affiliations
Contributions
J.Z. and L.B. jointly supervised the preparation of this manuscript. K.Q. and C.M.G. contributed their clinical and translational expertise on the topic.
Corresponding authors
Ethics declarations
Competing interests
C.M.G. serves on advisory committees for Abdera, AstraZeneca, BMS, Daiichi Sankyo, G1, Jazz, MonteRosa, Roche/Genentech and reports Speaking Engagement from AstraZeneca, BeiGene, MJH, OncLive, PeerView, Targeted Healthcare, and receives Paid Consulting from Catalyst, Kisoji, STCube. L.A.B. serves on advisory committees for AstraZeneca, AbbVie, Genetech, Amgen, Daiichi Sankyo, Novartis and has research support from AstraZeneca, Amgen. J.Z. reports grants from Merck and Helius, grants and personal fees from Johnson and Johnson and Novartis, personal fees from Bristol-Myers Squibb, AstraZeneca, GenePlus, Innovent, Varian, Catalyst and Hengrui outside the submitted work. K.G. declares no competing interests.
Peer review
Peer review information
Nature Cancer thanks Christine Lovly and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qin, K., Gay, C.M., Byers, L.A. et al. The current and emerging immunotherapy paradigm in small-cell lung cancer. Nat Cancer 6, 954–966 (2025). https://doi.org/10.1038/s43018-025-00992-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s43018-025-00992-5