Abstract
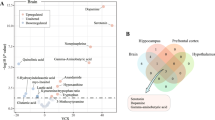
Despite the widespread use of metabolomics and proteomics to explore the molecular landscape of depression, there is a lack of consensus regarding dysregulated molecules with replicable evidence. Thus, this study aimed to identify robust metabolomic and proteomic features in depression by integrating evidence from large-scale studies. In this study, a knowledge base-mining approach was adopted to compile a list of dysregulated molecules derived from metabolomic and proteomic studies. A vote-counting approach was performed to identify consistently altered molecules in the blood and urine samples of patients with depression. A total of 2398 molecular entries were selected, comprising 857 unique metabolites and 468 unique proteins from 143 metabolomic and 23 proteomic studies in depression. The results of vote-counting analyses revealed that 11 metabolites in blood and 5 metabolites in urine exhibited consistent disturbances across studies. Circulating levels of glutamic acid and phosphatidylcholine (32:0) were elevated in depressive patients, whereas the levels of tryptophan, kynurenic acid, kynurenine, acetylcarnitine, serotonin, creatinine, inosine, phenylalanine, and valine were lower. Urinary levels of isobutyric acid, alanine, and nicotinic acid were higher, whereas the levels of N-methylnicotinamide and tyrosine were lower. Moreover, analysis of the proteomic dataset identified only one circulating protein, ceruloplasmin, that was consistently dysregulated. Convergence comparison prioritized tryptophan as the top-ranked circulating metabolite, followed by kynurenic acid, acetylcarnitine, creatinine, serotonin, and valine. Collectively, robust evidence of metabolomic changes was observed in patients with depression, pointing to a role as potential biomarkers. Further investigation of consensus proteomic features for depression is necessitated.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets generated in the current study are available in Supplemental Datasets 1–4, or on the ProMENDA website (https://menda.cqmu.edu.cn).
References
Malhi GS, Mann JJ. Depression. Lancet. 2018;392:2299–312.
Arias-de la Torre J, Vilagut G, Ronaldson A, Serrano-Blanco A, Martín V, Peters M, et al. Prevalence and variability of current depressive disorder in 27 European countries: a population-based study. Lancet Public Health. 2021;6:e729–38.
Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in U.S. depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. 2022;63:726–33.
Vigo D, Thornicroft G, Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3:171–8.
Marx W, Penninx BWJH, Solmi M, Furukawa TA, Firth J, Carvalho AF, et al. Major depressive disorder. Nat Rev Dis Primers. 2023;9:44.
Tian H, Hu Z, Xu J, Wang C. The molecular pathophysiology of depression and the new therapeutics. MedComm. 2022;3:e156.
Harmer CJ, Duman RS, Cowen PJ. How do antidepressants work? New perspectives for refining future treatment approaches. Lancet Psychiatry. 2017;4:409–18.
Villas Boas GR, Boerngen de Lacerda R, Paes MM, Gubert P, Almeida WLDC, Rescia VC, et al. Molecular aspects of depression: a review from neurobiology to treatment. Eur J Pharmacol. 2019;851:99–121.
Suhre K, McCarthy MI, Schwenk JM. Genetics meets proteomics: perspectives for large population-based studies. Nat Rev Genet. 2021;22:19–37.
Nedic Erjavec G, Konjevod M, Nikolac Perkovic M, Svob Strac D, Tudor L, Barbas C, et al. Short overview on metabolomic approach and redox changes in psychiatric disorders. Redox Biol. 2018;14:178–86.
Zheng P, Gao HC, Li Q, Shao WH, Zhang ML, Cheng K, et al. Plasma metabonomics as a novel diagnostic approach for major depressive disorder. J Proteome Res. 2012;11:1741–8.
Xu HB, Zhang RF, Luo D, Zhou Y, Wang Y, Fang L, et al. Comparative proteomic analysis of plasma from major depressive patients: identification of proteins associated with lipid metabolism and immunoregulation. Int J Neuropsychopharmacol. 2012;15:1413–25.
Tkachev A, Stekolshchikova E, Vanyushkina A, Zhang H, Morozova A, Zozulya S, et al. Lipid alteration signature in the blood plasma of individuals with schizophrenia, depression, and bipolar disorder. JAMA Psychiatry. 2023;80:250–9.
Ogawa S, Koga N, Hattori K, Matsuo J, Ota M, Hori H, et al. Plasma amino acid profile in major depressive disorder: analyses in two independent case-control sample sets. J Psychiatr Res. 2018;96:23–32.
Caspani G, Turecki G, Lam RW, Milev RV, Frey BN, MacQueen GM, et al. Metabolomic signatures associated with depression and predictors of antidepressant response in humans: a CAN-BIND-1 report. Commun Biol. 2021;4:903.
Silva-Costa LC, Smith BJ, Carregari VC, Souza GHMF, Vieira EM, Mendes-Silva AP, et al. Plasma proteomic signature of major depressive episode in the elderly. J Proteom. 2022;269:104713.
Bot M, Milaneschi Y, Al-Shehri T, Amin N, Garmaeva S, Onderwater GLJ, et al. Metabolomics profile in depression: a pooled analysis of 230 metabolic markers in 5283 cases with depression and 10,145 controls. Biol Psychiatry. 2020;87:409–18.
Pu J, Liu Y, Zhang H, Tian L, Gui S, Yu Y, et al. An integrated meta-analysis of peripheral blood metabolites and biological functions in major depressive disorder. Mol Psychiatry. 2021;26:4265–76.
Comes AL, Papiol S, Mueller T, Geyer PE, Mann M, Schulze TG. Proteomics for blood biomarker exploration of severe mental illness: pitfalls of the past and potential for the future. Transl Psychiatry. 2018;8:160.
Guest PC, Guest FL, Martins-de Souza D. Making sense of blood-based proteomics and metabolomics in psychiatric research. Int J Neuropsychopharmacol. 2016;19:pyv138.
Romeo B, Choucha W, Fossati P, Rotge JY. Meta-analysis of central and peripheral γ-aminobutyric acid levels in patients with unipolar and bipolar depression. J Psychiatry Neurosci. 2018;43:58–66.
Arnone D, Saraykar S, Salem H, Teixeira AL, Dantzer R, Selvaraj S. Role of kynurenine pathway and its metabolites in mood disorders: a systematic review and meta-analysis of clinical studies. Neurosci Biobehav Rev. 2018;92:477–85.
Pan JX, Xia JJ, Deng FL, Liang WW, Wu J, Yin BM, et al. Diagnosis of major depressive disorder based on changes in multiple plasma neurotransmitters: a targeted metabolomics study. Transl Psychiatry. 2018;8:130.
Goveia J, Pircher A, Conradi LC, Kalucka J, Lagani V, Dewerchin M, et al. Meta-analysis of clinical metabolic profiling studies in cancer: challenges and opportunities. EMBO Mol Med. 2016;8:1134–42.
Pu J, Liu Y, Gui S, Tian L, Yu Y, Song X, et al. Metabolomic changes in animal models of depression: a systematic analysis. Mol Psychiatry. 2021;26:7328–36.
Pu J, Liu Y, Gui S, Tian L, Yu Y, Wang D, et al. Effects of pharmacological treatment on metabolomic alterations in animal models of depression. Transl Psychiatry. 2022;12:175.
Pu J, Yu Y, Liu Y, Tian L, Gui S, Zhong X, et al. MENDA: a comprehensive curated resource of metabolic characterization in depression. Brief Bioinform. 2020;21:1455–64.
Pu J, Yu Y, Liu Y, Wang D, Gui S, Zhong X, et al. ProMENDA: an updated resource for proteomic and metabolomic characterization in depression. Transl Psychiatry. 2024;14:229.
Pang Z, Lu Y, Zhou G, Hui F, Xu L, Viau C, et al. MetaboAnalyst 6.0: towards a unified platform for metabolomics data processing, analysis and interpretation. Nucleic Acids Res. 2024;52:W398–W406.
Fischer M, Hoffmann S. Synthesizing genome regulation data with vote-counting. Trends Genet. 2022;38:1208–16.
Rikke BA, Wynes MW, Rozeboom LM, Barón AE, Hirsch FR. Independent validation test of the vote-counting strategy used to rank biomarkers from published studies. Biomark Med. 2015;9:751–61.
Xue C, Li G, Zheng Q, Gu X, Shi Q, Su Y, et al. Tryptophan metabolism in health and disease. Cell Metab. 2023;35:1304–26.
Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2023;28:3243–56.
Jauhar S, Cowen PJ, Browning M. Fifty years on: serotonin and depression. J Psychopharmacol. 2023;37:237–41.
Vécsei L, Szalárdy L, Fülöp F, Toldi J. Kynurenines in the CNS: recent advances and new questions. Nat Rev Drug Discov. 2013;12:64–82.
Marx W, McGuinness AJ, Rocks T, Ruusunen A, Cleminson J, Walker AJ, et al. The kynurenine pathway in major depressive disorder, bipolar disorder, and schizophrenia: a meta-analysis of 101 studies. Mol Psychiatry. 2021;26:4158–78.
Tóth F, Cseh EK, Vécsei L. Natural molecules and neuroprotection: kynurenic acid, pantethine and α-lipoic acid. Int J Mol Sci. 2021;22:403.
Roiser JP, McLean A, Ogilvie AD, Blackwell AD, Bamber DJ, Goodyer I, et al. The subjective and cognitive effects of acute phenylalanine and tyrosine depletion in patients recovered from depression. Neuropsychopharmacology. 2005;30:775–85.
Huang T, Balasubramanian R, Yao Y, Clish CB, Shadyab AH, Liu B, et al. Associations of depression status with plasma levels of candidate lipid and amino acid metabolites: a meta-analysis of individual data from three independent samples of US postmenopausal women. Mol Psychiatry. 2021;26:3315–27.
Mitani H, Shirayama Y, Yamada T, Maeda K, Ashby CR Jr, Kawahara R. Correlation between plasma levels of glutamate, alanine and serine with severity of depression. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1155–8.
Ho CSH, Tay GWN, Wee HN, Ching J. The utility of amino acid metabolites in the diagnosis of major depressive disorder and correlations with depression severity. Int J Mol Sci. 2023;24:2231.
Peng YF, Xiang Y, Wei YS. The significance of routine biochemical markers in patients with major depressive disorder. Sci Rep. 2016;6:34402.
Liu X, Zhao W, Hu F, Hao Q, Hou L, Sun X, et al. Comorbid anxiety and depression, depression, and anxiety in comparison in multi-ethnic community of west China: prevalence, metabolic profile, and related factors. J Affect Disord. 2022;298:381–7.
Lee BJ. Association of depressive disorder with biochemical and anthropometric indices in adult men and women. Sci Rep. 2021;11:13596.
Lieu C, Anderson R. Serum creatinine: why lower may not be better. Crit Care Med. 2007;35:2458–9.
Xu Y, Zeng L, Zou K, Shan S, Wang X, Xiong J, et al. Role of dietary factors in the prevention and treatment for depression: an umbrella review of meta-analyses of prospective studies. Transl Psychiatry. 2021;11:478.
Licht K, Hartl M, Amman F, Anrather D, Janisiw MP, Jantsch MF. Inosine induces context-dependent recoding and translational stalling. Nucleic Acids Res. 2019;47:3–14.
Niemann B, Haufs-Brusberg S, Puetz L, Feickert M, Jaeckstein MY, Hoffmann A, et al. Apoptotic brown adipocytes enhance energy expenditure via extracellular inosine. Nature. 2022;609:361–8.
Muto J, Lee H, Lee H, Uwaya A, Park J, Nakajima S, et al. Oral administration of inosine produces antidepressant-like effects in mice. Sci Rep. 2014;4:4199.
Liu X, Teng T, Li X, Fan L, Xiang Y, Jiang Y, et al. Impact of inosine on chronic unpredictable mild stress-induced depressive and anxiety-like behaviors with the alteration of gut microbiota. Front Cell Infect Microbiol. 2021;11:697640.
Yang J, Zhang Z, Xie Z, Bai L, Xiong P, Chen F, et al. Metformin modulates microbiota-derived inosine and ameliorates methamphetamine-induced anxiety and depression-like withdrawal symptoms in mice. Biomed Pharmacother. 2022;149:112837.
Bongiovanni R, Newbould E, Jaskiw GE. Tyrosine depletion lowers dopamine synthesis and desipramine-induced prefrontal cortex catecholamine levels. Brain Res. 2008;1190:39–48.
Tian S, Wu L, Zheng H, Zhong X, Liu M, Yu X, et al. Dietary niacin intake in relation to depression among adults: a population-based study. BMC Psychiatry. 2023;23:678.
Zhao L, Guo S, Yang J, Wang Q, Lu X. Association between niacin intake and depression: a nationwide cross-sectional study. J Affect Disord. 2023;340:347–54.
Zhao J, Zhang Y, Liu Y, Tang WQ, Ji CH, Gu JH, et al. Antidepressant-like effects of 1-methylnicotinamide in a chronic unpredictable mild stress model of depression. Neurosci Lett. 2021;742:135535.
Liu Z, Li C, Fan X, Kuang Y, Zhang X, Chen L, et al. Nicotinamide, a vitamin B3 ameliorates depressive behaviors independent of SIRT1 activity in mice. Mol Brain. 2020;13:162.
Chen Y, Xiao N, Chen Y, Chen X, Zhong C, Cheng Y, et al. Semen sojae praeparatum alters depression-like behaviors in chronic unpredictable mild stress rats via intestinal microbiota. Food Res Int. 2021;150:110808.
Liu X, Zhong S, Yan L, Zhao H, Wang Y, Hu Y, et al. Correlations among mRNA expression levels of ATP7A, serum ceruloplasmin levels, and neuronal metabolism in unmedicated major depressive disorder. Int J Neuropsychopharmacol. 2020;23:642–52.
Perng W, Aslibekyan S. Find the needle in the haystack, then find it again: replication and validation in the ‘omics era. Metabolites. 2020;10:286.
Halvey P, Farutin V, Koppes L, Gunay NS, Pappas DA, Manning AM, et al. Variable blood processing procedures contribute to plasma proteomic variability. Clin Proteom. 2021;18:5.
Ashkarran AA, Gharibi H, Voke E, Landry MP, Saei AA, Mahmoudi M. Measurements of heterogeneity in proteomics analysis of the nanoparticle protein corona across core facilities. Nat Commun. 2022;13:6610.
Lin Y, Caldwell GW, Li Y, Lang W, Masucci J. Inter-laboratory reproducibility of an untargeted metabolomics GC-MS assay for analysis of human plasma. Sci Rep. 2020;10:10918.
Ioannidis JP, Khoury MJ. Improving validation practices in “omics” research. Science. 2011;334:1230–2.
Pu J, Liu X, Liu Y, Gui S, Zhong X, Tian L, et al. Sex-specific plasma metabolome signatures in major depressive disorder. Psychiatry Clin Neurosci. 2019;73:713–4.
Chen JJ, Xie J, Li WW, Bai SJ, Wang W, Zheng P, et al. Age-specific urinary metabolite signatures and functions in patients with major depressive disorder. Aging. 2019;11:6626–37.
Chen JJ, Zhou CJ, Zheng P, Cheng K, Wang HY, Li J, et al. Differential urinary metabolites related with the severity of major depressive disorder. Behav Brain Res. 2017;332:280–7.
Acknowledgements
This work was supported by the Joint project of Chongqing Municipal Science and Technology Bureau and Chongqing Health Commission (2023CCXM003), the Natural Science Foundation Project of China (82371526), the Natural Science Foundation of Chongqing (CSTB2024NSCQ-QCXMX0033 and CSTB2024NSCQ-MSX1027), the Young Elite Scientists Sponsorship Program by CAST (2021QNRC001), and the Chongqing Medical Science and Technology Innovation Four Centers Construction Project - Chongqing Clinical Evaluation and Research Center for Cardiovascular and Cerebrovascular Drug and Devices (Materials) Project.
Author information
Authors and Affiliations
Contributions
Conception and design and interpretation of data: Juncai Pu and Peng Xie. Acquisition and analysis of data: Juncai Pu, Yiyun Liu, Yin Chen, Wei Tang, Yue Yu, Siwen Gui, Xiaogang Zhong, Dongfang Wang, Xiaopeng Chen, Yue Chen, Xiang Chen, Renjie Qiao, Yanyi Jiang, Hanping Zhang, Yi Ren, Li Fan and Haiyang Wang. Drafting display items: Juncai Pu, Hailin Wu, and Chi Liu. Drafting and revising the manuscript: Juncai Pu, Hailin Wu, Chi Liu and Peng Xie. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. The study was approved by The Ethics Committee of Chongqing Medical University (IACUC-CQMU-2024-0115). The datasets generated in the current study were collected from publicly available literature or reports, therefore informed consent forms are not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pu, J., Liu, Y., Wu, H. et al. Characterizing metabolomic and proteomic changes in depression: a systematic analysis. Mol Psychiatry 30, 3120–3128 (2025). https://doi.org/10.1038/s41380-025-02919-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-025-02919-z