Abstract
Introduction
Deep brain stimulation (DBS) is a neuromodulatory intervention for severe, treatment-refractory obsessive-compulsive disorder (OCD). We conducted the first meta-analysis using individual participant outcome data, systematically evaluating (1) efficacy of DBS compared to sham-stimulation in randomized controlled trials (RCTs), (2) adverse events and (3) methodological trial quality.
Methods
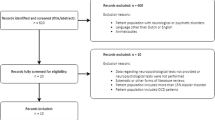
We conducted a systematic search across multiple databases, including all RCTs comparing DBS with sham in adults with OCD, regardless of stimulation target. We obtained Yale-Brown Obsessive-Compulsive Scale (YBOCS) data for individual participants and performed a two-stage random-effects meta-analysis. We evaluated trial quality using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE) approach.
Results
Nine RCTs with small sample sizes were included, resulting in a total sample of 91 patients. Meta-analysis showed a decrease of 5.1 YBOCS points in favor of DBS compared to sham (95% confidence interval, CI, 2.0–8.1, 0.56 Hedges’ g). OR was 4.7, 95% CI 1.8–12.2), with a NNT of 3.9. Optimization strategy appeared to impact efficacy, in favor of trials using gradual adjustments of DBS parameters guiding towards maximal improvement (beta 5.1, 95% CI 0.59–9.5, p-value 0.026). Adverse events occurred during surgery, active- and sham trial phases, and follow-up, with hypomania and cognitive problems being the most frequently reported stimulation-related adverse events. GRADE quality of evidence was rated low.
Discussion
Concluding, we found a significant effect of DBS compared to sham in treating OCD. However, the quality of evidence was low, and heterogeneity was high. Additional, rigorous, sham-controlled evidence could further improve credibility of DBS for OCD.
PROSPERO-registration number
CRD42024546836
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Code, and data that is available publicly, will be made available upon request.
References
Torres AR, Fontenelle L, Shavitt RG, Hoexter MQ, Pittenger C, Miguel E. Epidemiology, comorbidity, and burden of OCD. Oxford: Obsessivecompulsive disorder: phenomenology, pathophysiology, and treatment Oxford University Press; 2017.
Fawcett EJ, Power H, Fawcett JM. Women are at greater risk of OCD than men: a meta-analytic review of OCD prevalence worldwide. J Clin Psychiatry. 2020;81:13075.
Mian MK, Campos M, Sheth SA, Eskandar EN. Deep brain stimulation for obsessive-compulsive disorder: past, present, and future. Neurosurg Focus. 2010;29:E10.
Lai Y, Wang T, Zhang C, Lin G, Voon V, Chang J, Sun B. Effectiveness and safety of neuroablation for severe and treatment-resistant obsessive–compulsive disorder: a systematic review and meta-analysis. J Psychiatry Neurosci. 2020;45:356–69.
Pugh J. No going back? reversibility and why it matters for deep brain stimulation. J Med Ethics. 2019;45:225–30.
Lozano AM, Lipsman N, Bergman H, Brown P, Chabardes S, Chang JW, et al. Deep brain stimulation: current challenges and future directions. Nat Rev Neurol. 2019;15:148–60.
Nuttin B, Cosyns P, Demeulemeester H, Gybels J, Meyerson B. Electrical stimulation in anterior limbs of internal capsules in patients with obsessive-compulsive disorder. Lancet. 1999;354:1526.
Denys D, Graat I, Mocking R, de Koning P, Vulink N, Figee M, et al. Efficacy of deep brain stimulation of the ventral anterior limb of the internal capsule for refractory obsessive-compulsive disorder: a clinical cohort of 70 patients. Am J Psychiatry. 2020;177:265–71.
Chabardes S, Krack P, Piallat B, Bougerol T, Seigneuret E, Yelnik J, et al. Deep brain stimulation of the subthalamic nucleus in obsessive–compulsives disorders: long-term follow-up of an open, prospective, observational cohort. J Neurol Neurosurg Psychiatry. 2020;91:1349–56.
Alonso P, Cuadras D, Gabriëls L, Denys D, Goodman W, Greenberg BD, et al. Deep brain stimulation for obsessive-compulsive disorder: a meta-analysis of treatment outcome and predictors of response. PLoS ONE. 2015;10:e0133591.
Gadot R, Najera R, Hirani S, Anand A, Storch E, Goodman WK, et al. Efficacy of deep brain stimulation for treatment-resistant obsessive-compulsive disorder: systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2022;93:1166–73.
Kisely S, Hall K, Siskind D, Frater J, Olson S, Crompton D. Deep brain stimulation for obsessive-compulsive disorder: a systematic review and meta-analysis. Psychol Med. 2014;44:3533–42.
Martinho FP, Duarte GS, do Couto FS. Efficacy, effect on mood symptoms, and safety of deep brain stimulation in refractory obsessive-compulsive disorder: a systematic review and meta-analysis. J Clin Psychiatry. 2020;81:4067.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, Schünemann HJ. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, Stewart G, et al. Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–65.
Riley RD, Lambert PC, Abo-Zaid G. Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ. 2010;340:c221.
Buhmann C, Huckhagel T, Engel K, Gulberti A, Hidding U, Poetter-Nerger M, et al. Adverse events in deep brain stimulation: a retrospective long-term analysis of neurological, psychiatric and other occurrences. PLoS ONE. 2017;12:e0178984.
Bouwens van der Vlis TAM, van de Veerdonk MMGH, Ackermans L, Leentjens AFG, Janssen MLF, Kuijf ML, et al. Surgical and hardware-related adverse events of deep brain stimulation: a ten-year single-center experience. Neuromodulation. 2022;25:296–304.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Farris SG, McLean CP, Van Meter PE, Simpson HB, Foa EB. Treatment response, symptom remission, and wellness in obsessive-compulsive disorder. J Clin Psychiatry. 2013;74:685–90.
Rohatgi A. Webplotdigitizer: version 4.5. 2020. https://automeris.io/v4/. Accessed date: 14 June 2024.
Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Prasad M. Introduction to the GRADE tool for rating certainty in evidence and recommendations. Clin Epidemiol Glob Health. 2024;25:101484.
Riley RD, Ensor J, Hattle M, Papadimitropoulou K, Morris TP. Two-stage or not two-stage? That is the question for IPD meta-analysis projects. Res Synth Methods. 2023;14:903–10.
IntHout J, Ioannidis JPA, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14:25.
Turner H, Bernard R. Calculating and synthesizing effect sizes. Contemp Issues Commun Sci Disord. 2006;33:42–55.
Deeks JJ, Higgins JP, Altman DG, Group obotCSM. Analysing data and undertaking meta-analyses. Book chapter, in: Cochrane handbook for systematic reviews of interventions. Cochrane Training. 2019. p. 241–84.
van Westen M, Rietveld E, Bergfeld IO, de Koning P, Vullink N, Ooms P, et al. Optimizing deep brain stimulation parameters in obsessive–compulsive disorder. Neuromodulation. 2021;24:307–15.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63.
Bai RLL, Boland MR, Chen Y. A robust bayesian copas selection model for quantifying and correcting publication bias. arXiv:2005.029302021 [Preprint]. Available from: https://arxiv.org/abs/2005.029302021.
Harrer MCP, Furukawa T, Ebert DD. dmetar: companion R package for the guide ‘Doing Meta-Analysis in R. https://dmetar.protectlab.org/reference/. Access date: 1 July 2024.
Angelo CRB. boot: Bootstrap R (S-Plus) Functions. R package version 1.3-30.2024. https://cran.r-project.org/web//packages//boot/boot.pdf.
R Core Team, R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022.
Nuttin BJ, Gabriels LA, Cosyns PR, Meyerson BA, Andreewitch S, Sunaert SG, et al. Long-term electrical capsular stimulation in patients with obsessive-compulsive disorder. Neurosurgery. 2003;52:1263–72.
Schuurman PR, Van den Munckhoff P, M, Denys D, Deep brain stimulation in obsessive compulsive disorder: double-blind crossover study. Acta Neurochir. 2011;153:729–30.
Denys D, Mantione M, Figee M, van den Munckhof P, Koerselman F, Westenberg H, et al. Deep brain stimulation of the nucleus accumbens for treatment-refractory obsessive-compulsive disorder. Arch Gen Psychiatry. 2010;67:1061–8.
Mallet L, Polosan M, Jaafari N, Baup N, Welter ML, Fontaine D, et al. Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N Engl J Med. 2008;359:2121–34.
Welter ML, Alves Dos Santos JF, Clair AH, Lau B, Diallo HM, Fernandez-Vidal S, et al. Deep brain stimulation of the subthalamic, accumbens, or caudate nuclei for patients with severe obsessive-compulsive disorder: a randomized crossover controlled study. Biol Psychiatry. 2021;90:e45–e7.
Mosley PE, Windels F, Morris J, Coyne T, Marsh R, Giorni A, et al. A randomised, double-blind, sham-controlled trial of deep brain stimulation of the bed nucleus of the stria terminalis for treatment-resistant obsessive-compulsive disorder. Transl Psychiatry. 2021;11:190.
Goodman WK, Foote KD, Greenberg BD, Ricciuti N, Bauer R, Ward H, et al. Deep brain stimulation for intractable obsessive compulsive disorder: pilot study using a blinded, staggered-onset design. Biol Psychiatry. 2010;67:535–42.
Barcia JA, Avecillas-Chasin JM, Nombela C, Arza R, Garcia-Albea J, Pineda-Pardo JA, et al. Personalized striatal targets for deep brain stimulation in obsessive-compulsive disorder. Brain Stimul. 2019;12:724–34.
Huff W, Lenartz D, Schormann M, Lee SH, Kuhn J, Koulousakis A, et al. Unilateral deep brain stimulation of the nucleus accumbens in patients with treatment-resistant obsessive-compulsive disorder: outcomes after one year. Clin Neurol Neurosurg. 2010;112:137–43.
Abelson JL, Curtis GC, Sagher O, Albucher RC, Harrigan M, Taylor SF, et al. Deep brain stimulation for refractory obsessive-compulsive disorder. Biol Psychiatry. 2005;57:510–6.
Luyten L, Hendrickx S, Raymaekers S, Gabriels L, Nuttin B. Electrical stimulation in the bed nucleus of the stria terminalis alleviates severe obsessive-compulsive disorder. Mol Psychiatry. 2016;21:1272–80.
Stewart LA, Tierney JF. To IPD or not to IPD? advantages and disadvantages of systematic reviews using individual patient data. Eval Health Prof. 2002;25:76–97.
Skapinakis P, Caldwell DM, Hollingworth W, Bryden P, Fineberg NA, Salkovskis P, et al. Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2016;3:730–9.
Maiti R, Mishra A, Srinivasan A, Mishra BR. Pharmacological augmentation of serotonin reuptake inhibitors in patients with obsessive-compulsive disorder: a network meta-analysis. Acta Psychiatr Scand. 2023;148:19–31.
Vogt GS, Avendaño-Ortega M, Schneider SC, Goodman WK, Storch EA. Optimizing obsessive-compulsive symptom measurement with the yale-brown obsessive-compulsive scales-second edition. J Psychiatr Pract. 2022;28:294–309.
Karas PJ, Lee S, Jimenez-Shahed J, Goodman WK, Viswanathan A, Sheth SA. Deep brain stimulation for obsessive compulsive disorder: evolution of surgical stimulation target parallels changing model of dysfunctional brain circuits. Front Neurosci. 2018;12:998.
Raviv N, Staudt MD, Rock AK, MacDonell J, Slyer J, Pilitsis JG. A systematic review of deep brain stimulation targets for obsessive compulsive disorder. Neurosurgery. 2020;87:1098–110.
Mills EJ, Chan A-W, Wu P, Vail A, Guyatt GH, Altman DG. Design, analysis, and presentation of crossover trials. Trials. 2009;10:27.
Lathyris DN, Trikalinos TA, Ioannidis JP. Evidence from crossover trials: empirical evaluation and comparison against parallel arm trials. Int J Epidemiol. 2007;36:422–30.
Nuttin B, Gybels J, Cosyns P, Gabriels L, Meyerson B, Andreewitch S, et al. Deep brain stimulation for psychiatric disorders. Neurosurg Clin N Am. 2003;14:xv–xvi.
Haber SN, Yendiki A, Jbabdi S. Four deep brain stimulation targets for obsessive-compulsive disorder: are they different? Biol Psychiatry. 2021;90:667–77.
Baldermann JC, Schüller T, Kohl S, Voon V, Li N, Hollunder B, et al. Connectomic deep brain stimulation for obsessive-compulsive disorder. Biol Psychiatry. 2021;90:678–88.
Li N, Baldermann JC, Kibleur A, Treu S, Akram H, Elias GJB, et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat Commun. 2020;11:3364.
Meyer GM, Hollunder B, Li N, Butenko K, Dembek TA, Hart L, et al. Deep brain stimulation for obsessive-compulsive disorder: optimal stimulation sites. Biol Psychiatry. 2024;96:101–13.
Patrick EE, Fleeting CR, Patel DR, Casauay JT, Patel A, Shepherd H, Wong JK. Modeling the volume of tissue activated in deep brain stimulation and its clinical influence: a review. Front Hum Neurosci. 2024;18:1333183.
Graat I, Mocking R, Figee M, Vulink N, de Koning P, Ooms P, et al. Long-term outcome of deep brain stimulation of the ventral part of the anterior limb of the internal capsule in a cohort of 50 patients with treatment-refractory obsessive-compulsive disorder. Biol Psychiatry. 2021;90:714–20.
Bouwens TAM. Neurosurgery in obsessive compulsive disorder: from targets to treatment to tracts and back again. Doctoral Thesis. Maastricht University. Dat 6 Oct 2022. https://doi.org/10.26481/dis.20221006tb2022.
Hitti FL, Widge AS, Riva-Posse P, Malone DA Jr., Okun MS, Shanechi MM, et al. Future directions in psychiatric neurosurgery: proceedings of the 2022 American Society for Stereotactic and Functional Neurosurgery meeting on surgical neuromodulation for psychiatric disorders. Brain Stimul. 2023;16:867–78.
Wu H, Hariz M, Visser-Vandewalle V, Zrinzo L, Coenen VA, Sheth SA, et al. Deep brain stimulation for refractory obsessive-compulsive disorder (OCD): emerging or established therapy? Mol Psychiatry. 2021;26:60–5.
Vitek JL, Jain R, Chen L, Tröster AI, Schrock LE, House PA, et al. Subthalamic nucleus deep brain stimulation with a multiple independent constant current-controlled device in Parkinson’s disease (INTREPID): a multicentre, double-blind, randomised, sham-controlled study. Lancet Neurol. 2020;19:491–501.
Perestelo-Pérez L, Rivero-Santana A, Pérez-Ramos J, Serrano-Pérez P, Panetta J, Hilarion P. Deep brain stimulation in Parkinson’s disease: meta-analysis of randomized controlled trials. J Neurol. 2014;261:2051–60.
Graat I, van Rooijen G, Prinsen J, Bergfeld I, Figee M, Denys D, Mocking R. Cyclic versus continuous deep brain stimulation in patients with obsessive compulsive disorder: a randomized controlled trial. Brain Stimul. 2023;16:82–7.
Menchón JM, Real E, Alonso P, Aparicio MA, Segalas C, Plans G, et al. A prospective international multi-center study on safety and efficacy of deep brain stimulation for resistant obsessive-compulsive disorder. Mol Psychiatry. 2021;26:1234–47.
Tyagi H, Apergis-Schoute AM, Akram H, Foltynie T, Limousin P, Drummond LM, et al. A randomized trial directly comparing ventral capsule and anteromedial subthalamic nucleus stimulation in obsessive-compulsive disorder: clinical and imaging evidence for dissociable effects. Biol Psychiatry. 2019;85:726–34.
Provenza NR, Sheth SA, Dastin-van Rijn EM, Mathura RK, Ding Y, Vogt GS, et al. Long-term ecological assessment of intracranial electrophysiology synchronized to behavioral markers in obsessive-compulsive disorder. Nat Med. 2021;27:2154–64.
Mocking RJT, Graat I, Denys D. Why has deep brain stimulation had so little impact in psychiatry? Front Neurol. 2021;12:757142.
Brozek JL, Akl EA, Alonso-Coello P, Lang D, Jaeschke R, Williams JW, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines. Part 1 of 3. An overview of the GRADE approach and grading quality of evidence about interventions. Allergy. 2009;64:669–77.
Chong MC, Sharp MK, Smith SM, O’Neill M, Ryan M, Lynch R, et al. Strong recommendations from low certainty evidence: a cross-sectional analysis of a suite of national guidelines. BMC Med Res Methodol. 2023;23:68.
Nuttin B, Wu H, Mayberg H, Hariz M, Gabriëls L, Galert T, et al. Consensus on guidelines for stereotactic neurosurgery for psychiatric disorders. J Neurol Neurosurg Psychiatry. 2014;85:1003–8.
Acknowledgements
We thank MMG. Leeflang, PhD, for her guidance on statistical considerations and JG. Daams, MA, for his guidance on conducting the systematic search.
Author information
Authors and Affiliations
Contributions
SEC, MJN and JBZ designed the study. SEC and MN acquired, interpreted and analyzed the data. GAvW, RJTM supported the statistical analyses. SEC and MJN drafted the manuscript. JBZ and DD supervised the initial drafting of the manuscript. JBZ, GAvW, RJTM and DD provided critical revision and gave guidance in interpretation of findings and editing. All authors approved of the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. Denys, van Wingen and Mocking are currently executing an investigator-initiated clinical trial on deep brain stimulation for depression, where DBS-devices are funded by Boston Scientific. Mocking has received funding from the ZonMw GGZ Fellowship, Amsterdam UMC Starter Grant and National Plan Hoofdzaken.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cohen, S.E., Niemeijer, M.J., Zantvoord, J.B. et al. Deep brain stimulation for obsessive-compulsive-disorder: a systematic review and meta-analysis of individual participant outcome data from sham-controlled trials. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03092-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-025-03092-z