Abstract
Introduction
Falls are detrimental to the well-being of individuals with spinal cord injury (SCI). To establish effective fall prevention initiatives, a comprehensive understanding of falls after SCI is needed.
Objectives
To report the incidence proportion of falls and summarize the factors contributing to falls in individuals with SCI.
Study design
Systematic review and meta-analysis.
Methods
Eight databases were searched. Abstracts/full articles were screened by two researchers independently. Data concerning study design, participant characteristics, and the incidence proportion, factors, and consequences of falls were extracted. Risk of bias was assessed using a ___domain-based approach that considered sampling and measurement bias. The incidence proportions of falls were pooled for ambulators and wheelchair users separately using random-effects meta-analyses, and compared descriptively for inpatients and community-dwelling individuals. Fall-related factors were organized according to the Biological, Behavioral, Social & Economic and Environmental Model of fall risk.
Results
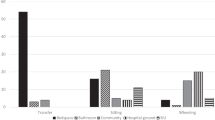
The search resulted in 1706 articles; 24 unique studies were included. The risk of sampling bias was high. All but one study focused on community-dwelling individuals; 78% (95% confidence interval 73–83%, I2 = 0%) of ambulators and 69% (95% confidence interval 60–76%, I2 = 59%) of wheelchair users fell ≥1 over 12 months. In contrast, only 13% of inpatients fell. Most fall-related factors were categorized as biological (e.g., muscle weakness), behavioral (e.g., inattentiveness) or environmental (e.g., uneven surfaces).
Conclusions
Falls are frequent among community-dwelling individuals with SCI. A variety of biological, behavioral, and environmental factors contribute to falls, some of which are modifiable and may be addressed through SCI-specific fall prevention initiatives.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Scuffham P, Chaplin S, Leegood R. Incidence and costs of unintentional falls in older people in the United Kingdom. J Epidemiol. 2003;57:740–4.
World Health Organization. WHO Global Report on Falls Prevention in Older Age. 2007. Accessed on 9 July 2015. Available from: www.who.int/ageing/publications/Falls_prevention7March.pdf.
Veterans Affairs Canada. Seniors’ falls – an emerging public health crisis. Accessed on 2 August 2017. Available from: https://www.veterans.gc.ca/eng/services/health/promotion/fallsp/senfalls.
Batchelor F, Hill K, Mackintosh S, Said C. What works in falls prevention after stroke?: a systematic review and meta-analysis. Stroke. 2010;41:1715–22.
Allen NE, Schwarzel AK, Canning CG. Recurrent falls in Parkinson’s disease: a systematic review. Parkinson’s Dis. 2013;2013:906274.
Canning CG, Paul SS, Nieuwboer A. Prevention of falls in Parkinson’s disease: a review of fall risk factors and the role of physical interventions. Neurodegener Dis Manag. 2014;4:203–21.
Cameron M, Coote S, Sosnoff JJ. Whom to target for falls-prevention trials: recommendations from the international MS falls prevention research network. Int J MS Care. 2014;16:203–7.
Matsuda PN, Verrall AM, Finlayson ML, Molton IR, Jensen MP. Falls among adults aging with disability. Arch Phys Med Rehabil. 2015;96:464–71.
Craven BC, Verrier M, Balioussis C, et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation. 2012. Rick Hansen Institute, Canada. Accessed 13 October 2017. Available from: https://rickhanseninstitute.org/e-scan-atlas.
Skelton F, Hoffman JM, Reyes M, Burns SP. Examining health-care utilization in the first year following spinal cord injury. J Spinal Cord Med. 2015;38:690–5.
Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord. 2012;50:365–72.
Thompson C, Mutch J, Parent S, Mac-Thiong J. The changing demographics of traumatic spinal cord injury: an 11-year study of 831 patients. J Spinal Cord Med. 2015;38:214–23.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Higgins JP, Altman DG, Sterne JA. Assessing risk of bias in included studies. In: Higgins JP, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0. The CochraneCollaboration; March 2011, chapter 8. Accessed May 23, 2016. Available at: http://www.cochranehandbook.org.
Rothman KJ, Greenland S, Lash TL. Case-control studies. In: Rothman KJ, Greenland S, Lash TL (eds). Modern Epidemiology. 3rd edn. (Lippincott Williams & Wilkins, Philadelphia, PA, 2008) pp 112.
Arora T, Oates AR, Lynd K, Musselman KE. Current state of balance assessment during transferring, sitting, standing and walking activities for the spinal cord injured population: a systematic review. J Spinal Cord Med 2018; 5:1–14.
Greenland S, Rothman KJ. Measures of occurrence. In: Rothman KJ, Greenland S, Lash TL, (eds). Modern Epidemiology. 3rd edn. Philadelphia, PA: Lippincott Williams & Wilkins; 2008. p. 33.
Brown LD, Cai TT, DasGupta A. Interval estimation for a binomial proportion. Stat Sci. 2001;16:101–33.
Valentine JC, Pigott TD, Rothstein HR. How many studies do you need? A primer on statistical power for meta-analysis. J Educ Behav Stat. 2010;35:215–47.
Wang, N How to Conduct a Meta-Analysis of Proportions in R: A Comprehensive Tutorial. 2018. Accessed 17 January 2019. Available from: https://doi.org/10.13140/RG.2.2.27199.00161.
Canadian Patient Safety Institute. Reducing Falls and Injuries From Falls: Getting Started Kit. June 2013. Accessed March 24, 2016. Available from: www.safehealthcarenow.ca.
Canadian Patient Safety Institute. What’s new in falls best practices? July 2013. Accessed 5 July 2016. Available from: http://www.patientsafetyinstitute.ca/en/NewsAlerts/News/pages/whats-new-in-falls-best-practices.aspx.
Brotherton SS, Krause JS, Nietert PJ. Falls in individuals with incomplete spinal cord injury. Spinal Cord. 2007;45:37–40.
Brotherton SS, Krause JS, Nietert PJ. A pilot study of factors associated with falls in individuals with incomplete spinal cord injury. J Spinal Cord Med. 2007;30:243–50.
Wannapakhe J, Arayawichanon P, Saengsuwan J, Amatachaya S. Changes of functional ability in patients with spinal cord injury with and without falls during 6 months after discharge. Phys Ther. 2014;94:675–81.
Wannapakhe J, Arrayawichanon P, Saengsuwan J, Amatachaya S. Medical complications and falls in patients with spinal cord injury during the immediate phase after completing a rehabilitation program. J Spinal Cord Med. 2015;38:84–90.
Sung J, Trace Y, Peterson EW, Sosnoff JJ, Rice LA. Falls among full-time wheelchair users with spinal cord injury and multiple sclerosis: a comparison of characteristics of fallers and circumstances of falls. Disabil Rehabil. 2017;41:1–7. E-pub Oct 25.
Jannings W. A quality improvement project to investigate the circumstances of lower limb fractures in non-ambulant persons with spinal cord injury. JARNA. 2017;20:14–18.
Jørgensen V, Roaldsen KS. Negotiating identity and self-image: perceptions of falls in ambulatory individuals with spinal cord injury – a qualitative study. Clin Rehabil. 2017;31:544–54.
Musselman KE, Arnold C, Pujol C, Lynd K, Oosman S. Falls, mobility, and physical activity after spinal cord injury: an exploratory study using photo-elicitation interviewing. Spinal Cord Ser Cases. 2018;4:39.
Forrest G, Huss S, Patel V, Jeffries J, Myers D, Barber C, et al. Falls on an inpatient rehabilitation unit: risk assessment and prevention. Rehabil Nurs. 2012;37:56–61.
Nelson A, Ahmed S, Harrow J, Fitzgerald S, Sanchez-Anguiano A, Gavin-Dreschnack D. Fall-related fractures in persons with spinal cord impairment: a descriptive analysis. SCI Nurs. 2003;20:30–37.
Nelson AL, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, et al. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil. 2010;91:1166–73.
Labruyère R, van Hedel HJ. Instrument validity and reliability of a choice response time test for subjects with incomplete spinal cord injury: relationship with function. Arch Phys Med Rehabil. 2011;92:1443–9.
Saunders LL, Krause JS. Injuries and falls in an aging cohort with spinal cord injury: SCI aging study. Top Spinal Cord Inj Rehabil. 2015;21:201–7.
Phonthee S, Saengsuwan J, Siritaratiwat W, Amatachaya S. Incidence and factors associated with falls in independent ambulatory individuals with spinal cord injury: a 6-month prospective study. Phys Ther. 2013;93:1061–72.
Phonthee S, Saengsuwan J, Amatachaya S. Falls in independent ambulatory patients with spinal cord injury: incidence, associated factors and levels of ability. Spinal Cord. 2013;51:365–8.
Jørgensen V, Forslund EB, Franzén E, Opheim A, Seiger Å, Ståhle A, et al. Factors associated with recurrent falls in individuals with traumatic spinal cord injury: a multicenter study. Arch Phys Med Rehabil. 2016;97:1908–16.
Kumprou M, Amatachaya P, Sooknuan T, Thaweewannakij T, Amatachaya S. Is walking symmetry important for ambulatory patients with spinal cord injury? Disabil Rehabil. 2018;40:836–41.
Saunders L, DiPiro N, Krause J, Brotherton S, Kraft S. Risk of fall-related injuries among ambulatory participants with spinal cord injury. Top Spinal Cord Inj Rehabil. 2013;19:259–66.
Amatachaya S, Wannapakhe J, Arrayawichanon P, Siritarathiwat W, Wattanapun P. Functional abilities, incidences of complications and falls of patients with spinal cord injury 6 months after discharge. Spinal Cord. 2011;49:520–4.
Amatachaya S, Pramodhyakul W, Wattanapan P, Eungpinichpong W. Ability of obstacle crossing is not associated with falls in independent ambulatory patients with spinal cord injury. Spinal Cord. 2015;53:598–603.
Forslund EB, Jørgensen V, Franzén E, Opheim A, Seiger Å, Ståhle A, et al. High incidence of falls and fall-related injuries in wheelchair users with spinal cord injury: a prospective study of risk indicators. J Rehabil Med. 2017;49:144–51.
Srisim K, Saengsuwan J, Amatachaya S. Functional assessments for predicting a risk of multiple falls in independent ambulatory patients with spinal cord injury. J Spinal Cord Med. 2015;38:439–45.
Jørgensen V, Forslund EB, Opheim A, Franzén E, Wahman K, Hultling C, et al. Falls and fear of falling predict future falls and related injuries in ambulatory individuals with spinal cord injury: a longitudinal observational study. J Physiother. 2017;63:108–13.
Wirz M, Müller R, Bastiaenen C. Falls in persons with spinal cord injury: validity and reliability of the Berg Balance Scale. Neurorehabil Neural Repair. 2010;24:70–77.
Prudham D, Evans JG. Factors associated with falls in the elderly: a community study. Age Ageing. 1981;10:141–6.
Public Health Agency of Canada. Seniors’ Falls in Canada. Second Report. 2014. Accessed 9 July 2016. Available at: http://www.phac-aspc.gc.ca/seniors-aines/publications/public/injury-blessure/seniors_falls-chutes_aines/assets/pdf/seniors_falls-chutes_aines-eng.pdf.
Simpson LA, Miller WC, Eng JJ. Effect of stroke on fall rate, ___location and predictors: a prospective comparison of older adults with and without stroke. PLoS ONE. 2011;6:e19431.
Stack E, Ashburn A. Fall events described by people with Parkinson’s disease: implications for clinical interviewing and the research agenda. Physiother Res Int. 1999;4:190–200.
Wood BH, Bilclough JA, Bowron A, Walker RW. Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. J Neurol Neurosurg Psychiatry. 2002;72:721–5.
Spoelstra SL, Given BA, Given CW. Fall prevention in hospitals: an integrative review. Clin Nurs Res. 2012;21:92–112.
Singh H, Craven BC, Flett HM, Kerry C, Jaglal SB, Silver MP, et al. Factors influencing fall prevention for patients with spinal cord injury from the perspectives of administrators in Canadian rehabilitation hospitals. 57th Annual Meeting of the International Spinal Cord Society. Sydney, Australia. 13–15 September, 2018.
Acknowledgements
We thank Katherine Chan, MSc, for assistance with data analysis.
Funding
This research was funded by a Craig H. Neilsen Foundation grant (#440070) to KEM.
Author information
Authors and Affiliations
Contributions
AK was responsible for data extraction and analysis, interpreting results and writing the manuscript. CP was responsible for data extraction and analysis, interpreting results and editing the manuscript. ML and NU were responsible for abstract and full-text screening and editing the manuscript. MP conducted the search and edited the manuscript. JD contributed to the interpretation of results and editing the manuscript. KEM was responsible for designing the review, overseeing screening and extraction, interpreting results and writing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Khan, A., Pujol, C., Laylor, M. et al. Falls after spinal cord injury: a systematic review and meta-analysis of incidence proportion and contributing factors. Spinal Cord 57, 526–539 (2019). https://doi.org/10.1038/s41393-019-0274-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-019-0274-4
This article is cited by
-
Amplify Gait to Improve Locomotor Engagement in Spinal Cord Injury (AGILE SCI) trial: study protocol for an assessor blinded randomized controlled trial
BMC Neurology (2024)
-
Feasibility of using a depth camera or pressure mat for visual feedback balance training with functional electrical stimulation
BioMedical Engineering OnLine (2024)
-
Identifying priorities for balance interventions through a participatory co-design approach with end-users
BMC Neurology (2023)
-
Technology used in activity based therapy for individuals living with spinal cord injury across Canada
Spinal Cord Series and Cases (2023)
-
Falls on an inpatient rehabilitation spinal injuries unit: the characteristics, circumstances, and consequences
Spinal Cord (2023)