Abstract
Study design
Retrospective multicenter study.
Objectives
To evaluate how preoperative neck pain influences clinical outcomes following posterior decompression for cervical ossification of the posterior longitudinal ligament (OPLL).
Setting
Fourteen medical institutions in Japan.
Methods
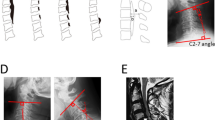
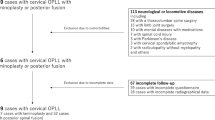
We enrolled 90 patients with cervical OPLL who underwent posterior decompression and were followed for a minimum of two years. We collected demographic data, medical history, and imaging findings. Patients were divided into two groups based on preoperative neck pain presence (Pre-op. neck pain (−) and (+) groups), and their outcomes were compared.
Results
There were no significant differences in patient demographics between the Pre-op. neck pain (−) and (+) groups. Both groups showed similar distributions of ossification types and K-line positivity. Perioperative complications were comparable between the two groups. Radiographic analysis revealed no significant differences in C2–7 angles or cervical range of motion, pre- and postoperatively. Both groups demonstrated significant improvement in postoperative Japanese orthopedic association (JOA) scores, but there were no significant differences in scores or recovery rates. In the Pre-op. neck pain (−) group, factors associated with appearance of postoperative neck pain included pre- and postoperative lower JOA scores and larger C2–7 angles in neutral and extension positions.
Conclusions
It emerges that lower pre- and postoperative JOA scores or larger C2–7 angles in neutral and extension positions predispose to postoperative neck pain even in those patients without preoperative neck pain. Therefore, this is worth discussing at the time of consenting patients for surgical decompression and fixation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in this study are available from the corresponding author on request.
References
Matsunaga S, Sakou T. Ossification of the posterior longitudinal ligament of the cervical spine: etiology and natural history. Spine. 2012;37:E309–314.
Abiola R, Rubery P, Mesfin A. Ossification of the posterior longitudinal ligament: etiology, diagnosis, and outcomes of nonoperative and operative management. Glob Spine J. 2016;6:195–204.
Nagoshi N, Tetreault LA, Nakashima H, Nouri A, Arnold P, Zileli M, et al. Do caucasians and east asians have different outcomes following surgery for the treatment of degenerative cervical myelopathy?: Results from the prospective multicenter AOSpine International Study. Spine. 2016;41:1428–35.
Matsumoto M, Chiba K, Toyama Y. Surgical treatment of ossification of the posterior longitudinal ligament and its outcomes. Spine. 2012;37:E303–308.
Nakashima H, Tetreault L, Nagoshi N, Nouri A, Arnold P, Yukawa Y, et al. Comparison of outcomes of surgical treatment for ossification of the posterior longitudinal ligament versus other forms of degenerative cervical myelopathy:Results from the prospective, multicenter AOSpine CSM-International Study of 479 patients. J Bone Joint Surg Am. 2016;98:370–8.
An HS, Al-Shihabi L, Kurd M. Surgical treatment for ossification of the posterior longitudinal ligament in the cervical spine. J Am Acad Orthop Surg. 2014;22:420–9.
Hirai T, Yoshii T, Iwanami A, Takeuchi K, Mori K, Yamada T, et al. Prevalence and distribution of ossified lesions in the whole spine of patients with cervical ossification of the posterior longitudinal ligament a multicenter study (JOSL CT study). PLoS One. 2016;11:e0160117.
Yoshii T, Hirai T, Iwanami A, Nagoshi N, Yakeuchi K, Mori K, et al. Co-existence of ossification of the nuchal ligament is associated with severity of ossification in the whole spine in patients with cervical ossification of the posterior longitudinal ligament -A multi-center CT study. J Orthop Sci. 2019;24:35–41.
Sakai K, Okawa A, Takahashi M, Arai Y, Kawabata S, Enomoto M, et al. Five-year follow-up evaluation of surgical treatment for cervical myelopathy caused by ossification of the posterior longitudinal ligament: a prospective comparative study of anterior decompression and fusion with floating method versus laminoplasty. Spine. 2012;37:367–76.
Hirai T, Yoshii T, Ushio S, Mori K, Maki S, Katsumi K, et al. Clinical characteristics in patients with ossification of the posterior longitudinal ligament: A prospective multi-institutional cross-sectional study. Sci Rep. 2020;10:5532.
Kumagai G, Ono A, Numasawa T, Wada K, Inoue R, Iwasaki H, et al. Association between roentgenographic findings of the cervical spine and neck symptoms in a Japanese community population. J Orthop Sci. 2014;19:390–7.
Nakajima H, Uchida K, Taguchi T, Yamashita T, Tominaga T, Tanaka M, et al. Multicenter cross-sectional study of the clinical features and types of treatment of spinal cord-related pain syndrome. J Orthop Sci. 2019;24:798–804.
Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine. 1981;6:354–64.
Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine. 2001;26:479–87.
Shiraishi T, Kato M, Yato Y, Ueda S, Aoyama R, Yamane J, et al. New techniques for exposure of posterior cervical spine through intermuscular planes and their surgical application. Spine. 2012;37:E286–E296.
Koda M, Yoshii T, Egawa S, Sakai K, Kusano K, Nakagawa Y, et al. Factors significantly associated with postoperative neck pain deterioration after surgery for cervical ossification of the posterior longitudinal ligament: Study of a cohort using a prospective registry. J Clin Med. 2021;10:5026.
Katsumi K, Hirai T, Yoshii T, Maki S, Mori K, Nagoshi N, et al. The impact of ossification spread on cervical spine function in patients with ossification of the posterior longitudinal ligament. Sci Rep. 2021;11:14337.
Choi BW, Hum TW. Significance of intramedullary high signal intensity on magnetic resonance imaging in patients with cervical ossification of the posterior longitudinal ligament. Clin Orthop Surg. 2015;7:465–9.
Mori K, Yoshii T, Egawa S, Sakai K, Kusano K, Tsutsui S, et al. Impact of obesity on cervical ossification of the posterior longitudinal ligament: a nationwide prospective study. Sci Rep. 2022;12:8884.
Nagoshi N, Watanabe K, Nakamura M, Matsumoto M, Lin N, Ma S, et al. Does diabetes affect the surgical outcomes in cases with cervical ossification of the posterior longitudinal ligament? A multicenter study from asia pacific spine study group. Global Spine J. 2023;13:353–9.
Li C, Zha G, Yang Z, Pang Y, Qiu S, Fan W, et al. K-line in patients with cervical ossification of the posterior longitudinal ligament: relationship with change in sagittal cervical curvature and laminoplasty outcomes. Arch Orthop Trauma Surg. 2022;142:1743–51.
Shi H, Chen L, Zhu L, Jiang ZL, Wu XT. Instrumented fusion versus instrumented non-fusion following expansive open-door laminoplasty for multilevel cervical ossification of the posterior longitudinal ligament. Arch Orthop Trauma Surg. 2023;143:2919–27.
Fujiwara H, Oda T, Makino T, Moriguchi Y, Yonenobu K, Kaito T. Impact of cervical sagittal alignment on axial neck pain and health-related quality of life after cervical laminoplasty in patients with cervical spondylotic myelopathy or ossification of the posterior longitudinal ligament: A prospective comparative study. Clin Spine Surg. 2018;31:E245–E251.
Nakashima H, Imagama S, Yoshii T, Egawa S, Sakai K, Kusano K, et al. Factors associated with loss of cervical lordosis after laminoplasty for patients with cervical ossification of the posterior longitudinal ligament: Data from a prospective multicenter study. Spine. 2023;48:1047–56.
Xu C, Zhang Y, Dong M, Wu H, Yu W, Tian Y, et al. The relationship between preoperative cervical sagittal balance and clinical outcome of laminoplasty treated cervical ossification of the posterior longitudinal ligament patients. Spine J. 2020;20:1422–9.
Lee CK, Shin DA, Yi S, Kim KN, Shin HC, Yoon DH, et al. Correlation between cervical spine sagittal alignment and clinical outcome after cervical laminoplasty for ossification of the posterior longitudinal ligament. J Neurosurg Spine. 2016;24:100–7.
Ogawa Y, Chiba K, Matsumoto M, Nakamura M, Takaishi H, Hirabayashi H, et al. Long-term results after expansive open-door laminoplasty for the segmental-type of ossification of the posterior longitudinal ligament of the cervical spine: a comparison with nonsegmental-type lesions. J Neurosurg Spine. 2005;3:198–204.
Martin AR, Jentzsch T, Wilson JRF, Moghaddamjou A, Jiang F, Rienmueller A, et al. Inter-rater Reliability of the Modified Japanese Orthopedic Association Score in Degenerative Cervical Myelopathy: A Cross-sectional Study. Spine. 2021;46:1063–9.
Joshi S, Balthillaya G, Neelapala YV. Thoracic posture and mobility in mechanical neck pain population: A review of the literature. Asian Spine J. 2019;13:849–60.
Zaed I, Bossi B, Ganau M, Tinterri B, Giordano M, Chibbaro S. Current state of benefits of Enhanced Recovery After Surgery (ERAS) in spinal surgeries: A systematic review of the literature. Neurochirurgie. 2022;68:61–68.
Author information
Authors and Affiliations
Contributions
TO collected and interpreted the data, and wrote the initial draft of this manuscript. NN, KT, MO, and SS assisted in the preparation of the manuscript. TO designed the study, and TI, TT, YH, KK, KD, HF, OT, MM, MN, KW, KI, and JY critically reviewed the manuscript. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work to ensure that questions associated with the accuracy or integrity of any part of the work were appropriately evaluated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics and Institutional Review Board of Keio University School of Medicine (approval number: #20110142). Informed consent was obtained from all participants prior to undergoing surgery. We certify that all applicable governmental and institutional regulations concerning the ethical use of human volunteers were followed during the course of this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Okubo, T., Nagoshi, N., Iga, T. et al. Does the presence of preoperative neck pain impact clinical outcomes after posterior decompression in patients with cervical ossification of the posterior longitudinal ligament?: Retrospective multicenter cohort study. Spinal Cord 62, 619–624 (2024). https://doi.org/10.1038/s41393-024-01027-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41393-024-01027-z