Abstract
Serum lipid levels, which are influenced by both genetic and environmental factors, are key determinants of cardiometabolic health and are influenced by both genetic and environmental factors. Improving our understanding of their underlying biological mechanisms can have important public health and therapeutic implications. Although psychosocial factors, including depression, anxiety, and perceived social support, are associated with serum lipid levels, it is unknown if they modify the effect of genetic loci that influence lipids. We conducted a genome-wide gene-by-psychosocial factor interaction (G×Psy) study in up to 133,157 individuals to evaluate if G×Psy influences serum lipid levels. We conducted a two-stage meta-analysis of G×Psy using both a one-degree of freedom (1df) interaction test and a joint 2df test of the main and interaction effects. In Stage 1, we performed G×Psy analyses on up to 77,413 individuals and promising associations (P < 10−5) were evaluated in up to 55,744 independent samples in Stage 2. Significant findings (P < 5 × 10−8) were identified based on meta-analyses of the two stages. There were 10,230 variants from 120 loci significantly associated with serum lipids. We identified novel associations for variants in four loci using the 1df test of interaction, and five additional loci using the 2df joint test that were independent of known lipid loci. Of these 9 loci, 7 could not have been detected without modeling the interaction as there was no evidence of association in a standard GWAS model. The genetic diversity of included samples was key in identifying these novel loci: four of the lead variants displayed very low frequency in European ancestry populations. Functional annotation highlighted promising loci for further experimental follow-up, particularly rs73597733 (MACROD2), rs59808825 (GRAMD1B), and rs11702544 (RRP1B). Notably, one of the genes in identified loci (RRP1B) was found to be a target of the approved drug Atenolol suggesting potential for drug repurposing. Overall, our findings suggest that taking interaction between genetic variants and psychosocial factors into account and including genetically diverse populations can lead to novel discoveries for serum lipids.
Similar content being viewed by others
Introduction
The concentrations of key serum lipids, such as high-density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDLC), and triglycerides (TG) are routinely assessed to determine an individual’s cardiometabolic clinical risk profile, and to guide drug therapy (e.g., statins) aiming to reduce the morbidity and mortality associated with diseases such as coronary artery disease, stroke, and type 2 diabetes. Serum lipid levels are known to be influenced both by lifestyle, including diet, physical activity, smoking, and alcohol consumption, as well as genetic factors, with over 700 lipids loci identified using genome-wide association studies (GWAS) [1,2,3]. Although the importance of both genetic and lifestyle factors is well-established, the interplay between these two factors on serum lipid levels is less well understood. The Gene-Lifestyle Interactions Working Group, under the aegis of the Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Consortium [4], has developed a framework for studying gene-lifestyle interactions for cardiometabolic traits in large, multi-ancestry meta-analyses [5]. This strategy has facilitated the discovery of novel lipids loci in studies accounting for interactions with smoking [6], physical activity [7], alcohol consumption [8], educational attainment [9], and sleep duration [10], suggesting that these lifestyle factors may indeed modulate genetic effects on serum lipids. The loci identified in these efforts could potentially explain how lifestyle exposures can contribute to disturbances in lipid levels.
Psychosocial factors, especially depression, contribute to the pathogenesis of cardiovascular diseases (e.g., myocardial infarction) and increased mortality in patients with coronary heart disease [11,12,13], and Mendelian Randomization (MR) analysis suggests that this association is causal [14]. Depression and depressive symptoms are associated with serum lipid concentrations [13, 15], the plasma lipidome [16, 17], and lipid metabolism, with distinct metabolic signatures associated with various symptom dimensions [18]. APOE alleles associated with serum lipids have also been associated with anxiety and depression [19, 20]. Some evidence from MR analyses suggests that depression increases TG and decreases HDLC [21]. Serum lipids may also mediate the association between depression and cardiovascular disease. The association between depression and coronary artery disease was attenuated when an MR analysis was adjusted for serum lipids [14]. Similarly, in one study, nearly a third of the association of depression with arterial stiffness, a key intermediary of major cardiovascular events, was found to be mediated by metabolic syndrome, particularly hypertriglyceridemia among men [22]. Low social support has been associated with high cholesterol in a nationally representative US nonelderly population [23] and with high cholesterol, LDL, and non-HDL cholesterol among type 2 diabetics and their families [24]. Both anxiety and depression have been associated with elevated triglycerides [25]. Proposed mechanisms through which psychosocial factors and serum lipids may influence each other include high dietary intake of saturated fat and cholesterol, gut dysbiosis, the hypothalamic-pituitary-adrenal axis, and neuroinflammation [26,27,28]. Both direct and indirect mechanisms, such as psychosocial factor-associated changes in lifestyle or medication use, are plausible. This may confound interaction effects. Importantly, there is evidence for a genetic contribution to some of these psychosocial factors, particularly depression [29,30,31,32,33].
In this study, we assess how incorporating interaction between genetic variants and psychosocial factors (depressive symptoms, anxiety symptoms, and low social support) helps identify lipid loci missed by standard marginal genetic effect GWAS. To maximize the transferability of our results and to address known gaps in the field, we prioritized the inclusion of diverse population groups, as ancestry can influence both genetic (e.g. frequency of variants, linkage disequilibrium around associated signals) and psychosocial factors (e.g. presence of stigma, availability of healthcare access). We conducted multi-ancestry meta-analyses of genome-wide variant × psychosocial factor interaction (G×Psy) studies on serum lipids in up to 133,157 individuals.
Results
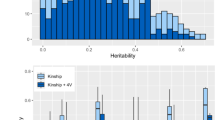
In this study of psychosocial factors and serum lipids, we meta-analyzed data on up to 133,157 individuals from 50 genome-wide interaction studies using a two-stage study design (Fig. 1; Study Details Supplementary Tables S1-2; Supplementary Note). Sample sizes and descriptive statistics of the studies participating in Stages 1 and 2 analyses are summarized in Supplementary Table 2. Study participants included European ancestry (EUR; 67.5%; n = 89,939), African ancestry (AFR; 14.4%; n = 19,133), Hispanic/Latino (HISP; 12.0%; n = 15,949), Asian ancestry (ASN; 3.5%; n = 4672), and Brazilian individuals (BRZ; 2.6%; n = 3464; see Methods for further details regarding selection of groups and population descriptors). All psychosocial factors were coded as binary variables. On average, 17.5% of Stage 1 participants were reported to have elevated depressive symptoms (DEPR) and 24.2% had elevated anxiety symptoms [ANXT], based on standard cutpoints, with a similar distribution among Stage 2 participants (15.8% [DEPR] and 24.3% [ANXT]). Low social support (SOCS) was defined as the lowest quartile of the distribution (Methods). Fewer studies had data on SOCS (n = 23) and ANXT (n = 21) than DEPR (n = 50; harmonization of psychosocial factors is described in Supplementary Table 3).
African ancestry (AFR), Asian ancestry (ASN), Brazilian (BRZ), European ancestry (EUR), Hispanic (HISP), cross-population meta-analysis (CPMA)1 Brazilian samples were only available in Stage 1, so a Stage 1 + 2 meta-analysis of BRZ was not possible. These samples are include in the cross-population Stage 1 + 2 meta-analysis; 2 As the 2df results joinly measure the variant's main and interaction effects, our main results only include those 2df findings that are also more than 500 kb from known lipids loci.
In Stage 1 population-specific and cross-population meta-analyses (CPMA), we identified 15,774 variants that met our selection criteria of P < 10−5 for either the 1 degree of freedom interaction test (1df) or the 2df joint test of the main and interaction effects (2df; Fig. 1). These variants were carried forward for further analysis in Stage 2 samples. In the meta-analysis of stages 1 and 2, there were 10,230 variants from 120 loci that were significantly associated in at least one model using either statistical test (P1df or P2df < 5 × 10−8; Supplementary Table 4). We found seven variants in four loci that were associated with serum lipids with a genome-wide significant p-value for the 1df test of interaction (Table 1). For instance, among those reporting low social support, the A allele of rs11949029 was associated with a much lower LDLC concentration than among those who did not (βInteraction = −19.2, SE 3.5 mg/dL, P1df = 4.1 × 10−8; Fig. 2A). Thus, among those with low social support, this allele was associated with 12.6 mg/dL lower LDLC, but 6.6 mg/dL higher LDLC among those not reporting low social support. In meta-analyses that did not include a multiplicative term (i.e. a standard GWAS model; available only for stage 1 studies), no association of the variant with LDLC was observed (P = 0.69), even after adjustment for SOCS (P = 0.75).
Forest plot showing all studies contributing data on an interaction of A. rs11949029 × social support (SOCS) on LDLC using a 1df test of the interaction term (this interaction was also statistically significant using the 2df joint test of the main effect and interaction, shown in Supplementary Figure 4D); and B. rs59808825 × anxiety symptoms (ANXT) on LDLC. Box size represents the precision of the estimate, with larger boxes shown for results with lower variance. Abbreviations: African ancestry (AFR), Brazilian (BRZ), Effect Allele Frequency (EAF), European Ancestry (EUR), Hispanic (HISP), cross-population meta-analysis (CPMA).
A significant association using the 2df joint test of the main effect and interaction can represent the main effect of a variant, its interaction with the exposure, or both. To exclude associations driven primarily by the main effect, we considered as previously unidentified only those variants with P2df < 5 × 10−8 that were independent of known loci (defined as ± 500 kb from the 95% credible sets reported in Graham et al [1] or variants reported in other major publications [34,35,36,37,38,39]). There were 14 variants and 8 loci that were significantly associated with serum lipids using the 2df test and independent from known loci (Table 2). Six of these loci displayed nominal significance for an interaction effect (P1df < 0.05). This includes three of the four loci that were genome-wide significant using the 1df test, with the remaining two near this threshold. Among these is rs59808825 (GRAMD1B [nearest gene]), for which the main effect of the C allele on LDLC was positive (β = 5.0, SE = 2.1 mg/dL) but an inverse interaction effect with ANXT (βInteraction = −22.9, SE = 4.2 mg/dL), so that the total effect of the C allele among those reporting anxiety symptoms was negative (P2df = 8.8 × 10−9; Fig. 2B). In the main effect only meta-analysis, no association between rs59808825 and LDLC was observed (P = 0.13). Of the 8 loci identified through the 2df test, two associations had P1df ≥ 0.1, suggesting that the 2df test may reflect novel main effect associations (though we cannot exclude that G×Psy interactions may contribute to these findings but are undetectable at the current sample sizes). For instance, the joint 2df test was significant for rs34636484 (CD96) × SOCS on LDLC (P2df = 3.1E-8), while the 1df test was not (P1df = 0.27; Supplementary Figure 4C). rs11702544 (RRP1B) × DEPR on HDLC was also plausibly driven by a main effect (Supplementary Figure 4H). Importantly, both of these potential main effect associations were identified in the CPMA results, highlighting the importance of including diverse populations for novel discoveries.
The inclusion of underrepresented population groups in this study also provided an advantage in identifying novel interaction associations, with associations observed at four lead loci at which no data from EUR studies were available because of a minor allele frequency < 0.01. For instance, an interaction of rs11949029 (CTC-207P7.1) and SOCS on LDLC was statistically significant for both the 1df test of interaction (Fig. 2A) and the 2df test of interaction and main effect (Supplementary Figure 4D) and was driven by data from the AFR and HISP populations. In this case, there was consistency of both the main and interaction associations across backgrounds. Such consistency was common among these lead findings; however, there were a few associations that were driven predominantly by one population, despite the availability of data for other groups. In the interaction between rs61248562 (UNC13 C) and DEPR on HDLC, the observed association among EUR reached statistical significance (β = 0.14; SE = 0.025; P1df = 5.2 × 10−9; Supplementary Figure 3C), yet this association was not seen in other populations despite a comparable number of samples with available data (EUR 15,052 vs. AFR 13,069 and HISP 15,977) and larger effect allele frequencies (EUR 0.02 vs. AFR 0.16 and HISP 0.07). As expected, the CPMA for this association was greatly reduced in statistical significance (P1df = 1.5 × 10−3). Similarly, the rs73597733 (MACROD2) × DEPR interaction on HDLC in AFR (P1df = 8.4 × 10−9) was not seen in HISP (P1df = 0.43; Supplementary Figure 3D).
Of the 10 lead associations in 9 loci that reached genome-wide statistical significance in the meta-analyses of Stages 1 and 2 (for one locus there were significant associations in two population groups), 4 were significant in both stages (P < 0.05) while 6 were only significant in stage 1 (Supplementary Table 5). There were 16 variants in 9 loci that were considered as the novel associated variant set for annotation and follow-up: those associated with either P1df < 5 × 10−8 (seven variants in four loci) or P2df < 5 × 10−8 and independent of known lipids loci (14 variants in 8 loci; five variants in three loci overlapping in 1df and 2df findings). The novel associated variants were characterized using FUMA. As expected, most of the variants were annotated to be intronic (n = 10) or intergenic (n = 3; Supplementary Table 6). While a single signal was detected for most of of the described loci in Tables 1 and 2, the associated region on chromosome 21 (CPMA-HDL-DEPR) had three independent genomic signals at variants rs11702544, rs6518309, and rs9977076. Each of these variants is an eQTL for three genes in a variety of tissues, including whole blood: PDXK, RRP1B, and HSF2BP [40] (Supplementary Table 7).
We also evaluated 257 variants in LD with our lead variants (R2 ≥ 0.6 in 1000 Genomes, Phase 3 ALL; Supplementary Table 8). Evaluation of these variants in RegulomeDB identified 75 variants (29.2%) with functional prediction scores ≤ 3, indicating moderate to high potential for regulatory effects. Variants within the locus on chromosome 21 characterized by rs11702544, rs6518309, and rs9977076 (RRP1B) had the lowest RegulomeDB scores in this set: 1a (n = 1) and 1b (n = 6), which indicates that they are likely to affect transcription factor binding to the gene targets, in this case HSF2BP, RRP1B, or LINC00313. These variants were also tested in our data and nearly reached statistical significance for the 2df interaction with DEPR on HDLC (P2df range 2.4 × 10−6 to 4.2 × 10−7), with similar effect sizes in all.
Next, we assessed the predicted chromatin state around our 16 novel associated variants using the minimum 15-core chromatin state models calculated across 127 tissue/cell types [41]. We identified histone chromatin markers in regions associated with strong transcription (n = 6; Supplementary Table 6). In the 257 variants in LD with our lead variants, there were histone chromatin markers consistent with active (n = 13) or flanking active (n = 21) transcription start sites, transcription at the 3′ or 5′ end (n = 7), or in regions associated with strong transcription (n = 50) (Supplementary Table 8). For most of our loci, significant chromatin interactions were detected between regions containing our variants and regions overlapping gene promoters (Supplementary Table 9); for instance, between the locus on chromosome 21 (lead variant rs11702544) and regions overlapping the promoter of multiple genes, including PDXK, RR1BP, and HSF2BP.
Finally, to explore the potential clinical relevance of our findings, we performed an integrated druggability analysis of identified genes, as previously described [42]. We queried high and medium priority candidate gene targets (identified by FUMA and OpenTargets) using the Drug-Gene Interaction database (DGIdb), which revealed 2 genes annotated as clinically actionable or members of the druggable genome (Supplementary Table 10). Several of these gene targets are implicated in ion transport (NKAIN3), vitamin metabolism (PDXK), and immune or viral response (CD96, RRP1B) pathways. We identified 1 gene, RRP1B, with a reported drug interaction. RRP1B was shown to interact with an FDA-approved drug, Atenolol, that has been evaluated in late-stage clinical trials using DrugBank and ClinicalTrials.gov databases (Supplementary Table 10). Atenolol is a well-established anti-hypertensive drug used to treat high blood pressure, heart failure, or angina in some patients. Together these results suggest a potential drug repurposing opportunity to intervene in a common pathway implicated in cardiometabolic disorders.
Discussion
In this study, we investigated genome-wide variant-by-psychosocial factor interactions (G×Psy) in large, multi-ancestry meta-analyses of serum lipids. We identified nine novel lipid loci using this strategy, including four loci based on the 1df test of interaction and eight loci based on the 2df joint test of interaction and main effects (with three loci significantly associated using both strategies). Importantly, most of these associations could not have been identified in a standard GWAS that does not take interaction into account. Our inclusion of relatively large sample sizes representing diverse ancestries facilitated novel findings. Functional annotation highlights the promise of some of these identified loci for understanding the potential influence of psychosocial factors on serum lipids.
Both the 1df test of interaction and the 2df test of main effect and interaction identified statistically significant results for rs73597733 (intronic to MACROD2) × DEPR on HDLC, in which the main effect of the variant was near zero, with a large positive association among those with depressive symptoms. Intriguingly, an interaction between an intronic variant in MACROD2 (not in LD with rs73597733) was previously found between thiazide diuretic use and HDLC [43]. Other intronic variants in MACROD2 have been associated with the ceramides and sphingomyelins, suggesting a potential role in lipids pathways [44]. There is a large body of evidence for associations of intronic variants in MACROD2 with complex psychosocial, neurological, and psychiatric traits, including: attention deficit hyperactivity disorder [45, 46], morningness (being a morning person) [47], risk-taking behavior [48], eating disorders [49], autism [50,51,52], and bipolar disorder [52, 53]. Infants with atypical neonatal neurobehavioral scores had differentially methylated CpG sites within the MACROD2 gene [54]. Macrod2 knockout mouse models displayed hyperactivity that became more pronounced with age [55]. Intronic variants in MACROD2 have also been associated with measures of cognitive ability [56,57,58] and a variety of brain measurements [59,60,61,62,63]. Given the significant evidence for the involvement of this gene in a range of complex psychological and psychiatric phenotypes and a previous finding for an interactive effect on HDLC, our reported finding of an interaction between an intronic variant in MACROD2 and DEPR on HDLC seems of particular interest and worthy of further investigation.
An association between rs59808825 (110 kb upstream of GRAMD1B) and ANXT on LDLC was P < 5 × 10−8 for both the 2df joint test of main effect and interaction and the 1df test of interaction, and no association was observed for this variant in an analysis without interaction modeled. GRAMD1B was identified as a locus for schizophrenia in multiple studies [64,65,66,67,68,69], a condition that has been linked with anxiety [70, 71]. The protein encoded by GRAMD1B, Gramd1b or Aster-B, has a role in cholesterol homeostasis, transporting accessible cholesterol from the plasma membrane to the endoplasmic reticulum [72, 73]. It was recently discovered that Aster proteins including Aster-B are key players in dietary lipid absorption in mice: the systemic absorption of dietary cholesterol was reduced by treatment with a small-molecule Aster inhibitor and mice without intestinal Aster proteins were protected from diet-induced hypercholesterolemia [74]. While further investigation is needed to propose a biological mechanism that might underlie the observed interaction between this variant and ANXT on LDLC, the known associations between nearby GRAMD1B with both complex psychiatric and psychological phenotypes and absorption of dietary lipid are intriguing.
We identified a 2df interaction of DEPR with variants on chromosome 21 (lead variant rs11702544 [RRP1B]) that appeared to represent a novel main effect of a common variant on HDLC. Interestingly, there was some evidence for an association of rs11702544 with HDLC using a standard GWAS model in the recent Global Lipids Genetics Consortium results (P = 2.2E-6) [1], consistent with the contribution of a main effect of this variant contributing to the 2df joint test of main effect and interaction. FUMA annotation identified 3 independent genomic loci in this region, each of which is an eQTL for PDXK, RRP1B, and HSF2BP. Each of the genes has been previously associated with risk of diseases for which serum lipids concentration is a key risk factor: PDXK and RRP1B with coronary artery disease [75] and HSF2BP with cardiovascular disease [76]. PDXK encodes a protein essential for the generation of the active form of Vitamin B6. PDXK mRNA levels in adipose tissue were strongly associated with adipogenic, lipid-droplet-related, and lipogenic genes, and administration of the active form of Vitamin B6 led to increased adipogenic markers in adipocyte precursor cells [77]. While the role for variants in this locus in HDLC concentration is not clear, they have been shown to affect PDXK expression, which could affect HDLC concentration through the expression of genes involved in lipogenesis. Our druggability analysis also identified PDXK as part of the druggable genome. RRP1B is a target gene that interacts with the beta-blocker drug Atenolol, which is sometimes used to treat hypertension and chronic angina.
We also identified an association using the 2df test rs34636484 (CD96) × SOCS on LDLC. The main effect appeared to contribute more to the association than the interaction at this locus, as the association was also apparent in a standard GWAS model in our data and the 1df test of interaction was not significant (P = 0.27). Based on these results, the association at rs34636484 appears to represent a novel main effect locus; however, this result should be interpreted with caution. The association of rs34636484 and LDLC was recently evaluated in the Global Lipids Genetics Consortium with a much larger sample size (n = 1,393,230 at this locus) and was not statistically significant (P = 0.029) [1].
Some of our significant associations were fairly consistent across studies within the same population group, but with no compelling evidence of association in other population groups, despite the availability of data. For instance, rs61248562 (UNC13C) × DEPR on HDLC was significant only among EUR, and not AFR or HISP in whom allele frequencies were higher and sample sizes were comparable. Similarly, an interaction of rs73597733 (MACROD2) × DEPR on HDLC in AFR was not seen in HISP at similar sample sizes (with a slightly lower allele frequency). It is unclear why these associations may differ by population group, but this phenomenon has been reported in previous gene-lifestyle interaction publications [6, 78, 79]. Differences in gene-lifestyle interactions across populations may arise from genomic factors, such as variations in linkage disequilibrium that lead to the tagging of different variants, as well as from lifestyle factors, such as differences in the measurement of or the experience of the psychosocial factor or in the behaviors or conditions associated with that psychosocial factor.
Psychosocial factors are complex traits that are associated with a variety of other factors, including some lifestyle exposures that we have previously evaluated using the same genome-wide interaction study approach. Overlap in the interaction results for this study and previous analyses for one of these associated lifestyle factors could be very informative for disentangling the mechanism underlying these statistical interactions. We compared our statistically significant findings with those that we have previously reported for genome-wide interactions of smoking [6], alcohol intake [8], physical activity [7], educational attainment [9], and sleep duration [10] on serum lipids; no overlap among the results was identified. If one of our loci were found to be associated with a psychosocial factor, that could provide additional context into the relationship between psychosocial factors and serum lipids. To explore this possibility, we evaluated recent GWAS for these traits [29, 33, 80,81,82,83,84], but did not identify any overlap with our loci of interest.
Some of the strengths of this study include the relatively large sample sizes for a study of psychosocial factors, with analyses including up to 133,157 individuals. Also notable was the particular attention to the inclusion of non-European ancestry individuals (reaching over 19,000 AFR and nearly 16,000 HISP, although the number of ASN and BRZ was smaller, <5000 per population). The sample sizes for the non-European ancestry groups, however, were relatively small in size, particularly in terms of the statiscial power needed for a gene-environment interaction study. We used a two-stage design with both a 1df test of interaction and a 2df joint test of main effect and interaction, an approach that is well-established for the study of gene-lifestyle interactions [6,7,8,9,10, 78, 79, 85, 86]. Our study also has some limitations. First, we had a smaller sample size for Stage 2, particularly for certain populations; as a result, the power for our two-stage approach was reduced. Second, despite our best efforts to harmonize psychosocial factors, the use of different instruments to measure these outcomes may have resulted in heterogeneity among studies, which would have reduced the power to identify lipids loci. In addition, these phenotypes themselves are quite complex and heterogeneous, and that complexity is not reflected in our categorization. Moreover, although our sample size is large for a study of lipids and psychosocial factors, it is not large enough to enable correction for multiple testing with adequate statistical power, and so its results need further validation. We did not have enough statistical power to usefully evaluate differences in these interactions by sex, which may prove to be of interest, as there are differences in the pathophysiology of cardiovascular disease by sex, and women experience a greater burden of depression [87]. Additionally, the association between TG and depressive symptoms has been shown to differ by sex, with men showing a stronger association [88], and low social support had a greater adverse effect on cardiovascular disease prevention among men than women [89]. Evaluating these interactions would require much greater sample sizes than were available in the current study. Although we have organized our contributing studies into population groups, there is likely to be meaningful heterogeneity within those groups in terms of relevant environmental background. For instance, the East Asian population group included individuals living in China as well as individuals with ancestry in China living in the United States. Information regarding neuropsychiatric medication use was not collected, though it is possible that use of these medications might directly or indirectly influence serum lipid levels [90]. In silico functional annotation and druggability analyses identified loci and candidate drug-gene interactions that are of interest for further follow-up; future experimental studies are needed to validate these findings.
In summary, we identified novel lipids loci in this large, multi-ancestry meta-analyses of genome-wide interaction studies of variants and psychosocial factors. Understanding these loci may help to disentangle the complex interplay between factors such as anxiety, depression, and low social support on serum lipids, a key biomarker of cardiometabolic risk.
Materials and methods
Study design
We adopted a two-stage study design (Fig. 1) that was implemented according to the Gene-Lifestyle Interactions Working Group of the CHARGE consortium [5]. We included men and women aged between 18 to 80 years of age with available data on lipids and psychosocial factors, and with genotype data imputed to the 1000 Genomes reference panel.
Stage 1 included 77,413 individuals in 31 study/population groups. Each study conducted genome-wide analyses (GWAS) incorporating a variant-by-psychosocial factor multiplicative interaction term. Centralized quality control was carried out, which was followed by a meta-analysis within and across five population groups: African ancestry (AFR), Asian ancestry (ASN), Brazilian (BRZ), European ancestry (EUR), and Hispanic (HISP). Variants that showed suggestive (P < 10−5) associations for either a 1df test of interaction or a 2df joint test of interaction and main effect were carried forward for evaluation in Stage 2. Stage 2 analyses included data on 55,744 individuals from 19 studies distributed in 4 population groups. As no BRZ samples were included in Stage 2, no population-specific Stage 1 + 2 meta-analysis was undertaken, though the BRZ samples were included in cross-population meta-analyses (CPMA). Analytical details (Supplementary Table S1) and descriptive statistics (Supplementary Table S2) of each participating study for Stages 1 and 2 are provided.
Phenotypes and lifestyle variables studied
Analyses were conducted separately for three lipid parameters: HDLC, LDLC, and TG. HDLC and TG were directly assayed and natural log-transformed prior to analysis. LDLC was either directly assayed or derived using the Friedewald equation: LDLC = TG – HDLC – (TG / 5), if TG ≤ 400 mg/dL [91]. If a sample was drawn from an individual who had not been fasting for at least 8 h, then neither TG nor derived LDLC values were used. LDLC values were adjusted for lipid-lowering medication use (defined as the use of a statin or of any unspecified lipid-lowering medication after 1994, when statin usage became common). If LDLC was directly assayed, adjustment for lipid-lowering drugs was performed by dividing the LDLC value by 0.7. If LDLC was derived using the Friedewald equation, total cholesterol was first adjusted for lipid-lowering drug use (total cholesterol/0.8) before calculation of LDLC. No adjustments were made for any other lipid medication, nor were adjustments made to HDLC or triglycerides for medication use. For longitudinal studies where multiple lipid measurements were available, analysts selected the measurement with the largest sample size for analysis.
The three psychosocial variables (elevated depressive symptoms [DEPR], low social support [SOCS], and elevated anxiety symptoms [ANXT]) were measured within each cohort using validated screening questionnaires and coded as binary (yes/no) variables. A standard cut point was used for DEPR and ANXT, and SOCS was defined based on the lowest quartile of perceived social support. Further details regarding the instruments used within each study are given (Supplementary Table 3). Where multiple measurements of psychosocial factors were available, we used the questionnaire administered concomitantly with the measurement of serum lipids.
Genotyping and imputation
To harmonize data across studies, all studies imputed to 1000 Genomes data. Details on genotyping and imputation for each of the included studies are given in Supplementary Table 1. Most studies used Affymetrix (Santa Clara, CA, USA) or Illumina (San Diego, CA, USA) arrays and imputed to the cosmopolitan reference panel of the 1000 Genomes Project Phase I Integrated Release Version 3 Haplotypes. Prior to analysis, studies excluded all variants with minor allele frequency <0.01 or those that mapped to the X and Y chromosomes or the mitochondria.
Study-level genome-wide analysis
Each cohort participating in Stage 1 analysis regressed serum lipids (Y) on the variant (G), psychosocial factor (E), and their interaction (G×E), with adjustment for covariates (C) including age, sex, principal components, and study-specific variables (listed for each study in Supplementary Table 1):
The 1df test was based on the null hypothesis H0: \({\beta }_{G\times E}=0\), while the 2df test was based on H0: \({{\beta }_{G}=\beta }_{G\times E}=0\). [92] To ensure robust estimates of covariance matrices and robust standard errors, studies of unrelated subjects used either the sandwich R package or ProbABEL genetic software [93]. Family studies used Mixed Model Analysis for Pedigrees and populations (MMAP), a comprehensive mixed model program that provides an optimized and flexible platform incorporating a wide range of covariance structures. Stage 2 studies carried out the same regressions, but only on the variants that reached suggestive significance (P < 10−5) in Stage 1 for any trait in population-specific or cross-population meta-analysis. For comparison, stage 1 studies also ran a main effect model (serum lipids as a function of the variant with adjustment for covariates and study-specific variables) and a main effect model additionally adjusted for the psychosocial factor.
Population groups
Appropriate selection of population descriptors is a matter of considerable discussion in the field and consensus regarding optimal terms has not yet emerged. In this work, contributing studies were subdivided into population groups based on where individuals included in those studies were expected to cluster genetically to reduce the potential for spurious findings due to population structure and to maximize the potential for discovery within a population. Inclusion of samples within a particular cluster of genetic similarity was based on consultation with study teams given their expertise and understanding of the study population. Our approach includes African ancestry (AFR), Asian ancestry (ASN), Brazilian (BRZ), European ancestry (EUR), and admixed Hispanic/Latino and Native American participants (HISP). The AFR population group includes sub-Saharan Africans as well as participants with predominantly African ancestry living in the United States. The ASN population group includes participants of predominantly Asian ancestry living in East Asia, Singapore, or the United States. The EUR population group includes participants with predominantly European ancestry living in Europe or the United States. The HISP population group includes admixed Hispanic/Latino and Native American participants living in the United States. Brazilian individuals (BRZ) were analyzed separately after consultation with local researchers regarding the genetic clustering of these participants.
Quality control and cross-population meta-analysis
We performed extensive study- and population-level quality control (QC) using the R package EasyQC for all GWAS results [94]. In study-level QC, allele frequencies for each study were compared visually to an ancestry-matched 1000 genomes reference panel to identify systematic errors in data preparation (no variants were excluded), and marker names were harmonized to ensure consistency across studies. Any resulting concerns were resolved in consultation with the contributing study. Variants were excluded if the imputation quality score was less than 0.5 or if 2×MAF×Nexposed×imputation quality score was less than 20. Population-level QC was also conducted prior to meta-analysis to check for any outliers among included studies, which might suggest improper trait transformation or model specification, among other things.
We then conducted population-specific and cross-population meta-analysis in Stage 1 using the approach developed by Manning et al. [95] and implemented in METAL [95, 96]. This method performs a joint meta-analysis of the variant and the G×Psy exposure regression coefficients and then uses a 2df test to identify genetic variants driven jointly by main and interaction effects. Additionally, we used the inverse-variance weighted meta-analysis implemented in METAL to meta-analyze G×Psy interaction coefficients alone using a 1df test. Variants in the Stage 1 meta-analysis had to be present in at least 2 cohorts or at least 3000 individuals for AFR and EUR, with a lower threshold (n = 2000) set for ASN, BRZ, and HISP because of the smaller number of individuals available in these ancestries. In Stage 2, we used the same approach as in Stage 1 to perform population-specific and cross-population meta-analyses. After combining results from Stages 1 and 2, variants with P < 5.0 × 10−8 for either the 2df joint test of the main effect and the interaction or the 1df test of the interaction were considered significant. Results with a heterozygosity p-value < 0.05 were evaluated further and excluded if results were driven by a single cohort.
The novelty of associated loci was determined by comparison to the recent Global Lipids Genetic Consortium results for GWAS meta-analyses including approximately 1.65 million individuals with notable inclusion of those of diverse ancestral backgrounds [1]. The 95% credible sets from the meta-analyses of all lipids traits (available at http://csg.sph.umich.edu/willer/public/glgc-lipids2021/results/credible_sets/) were compiled. Variants were considered novel if they were 500 kb from all variants listed in this list, as well as those reported in other major publications [34,35,36,37,38,39].
Identification of independent genomic loci and functional annotation
Identification of genetic loci related to each of the three serum lipids and functional annotation was accomplished using Functional Mapping and Annotation of GWAS (FUMA) v1.5.6 (http://fuma.ctglab.nl/) [97]. Variants were grouped into genomic loci using an R2 < 0.6 (1000 Genomes, Phase 3 ALL as the reference population) and a merge distance of 250 kb. Functional annotation was conducted using output from the set of tools incorporated within FUMA, including RegulomeDB score, Combined Annotation Dependent Deletion (CADD) score [98], 15-core chromatin state (ChromHMM) [41, 99, 100], and expression Quantitative Trait Loci (eQTL) on the variants from lead associations as well as those in LD with those variants (R2 > 0.1), using all tissues and all included databases (including GTex, BloodeQTL, BIOS, and BRAINEAC).
Druggability analysis
We first used the Drug-Gene Interaction database (DGIdb; v4.2.0) to query psychosocial factors-lipid interacting genes to determine the potential druggability of the candidate gene targets. We annotated genes for implicated pathways and functions using the Kyoto Encyclopedia of Genes and Genomes (KEGG) database. We annotated the druggability target categories and queried all interacting drugs reported in 41 databases (BaderLabGenes, CarisMolecularIntelligence, dGene, FoundationOneGenes, GO, HingoraniCasas, HopkinsGroom, HumanProteinAtlas, IDG, MskImpact, Oncomine, Pharos, RussLampel, Tempus, CGI, CIViC, COSMIC, CancerCommons, ChEMBL, ChemblDrugs, ChemblInteractions, ClearityFoundationBiomarkers, ClearityFoundationClinicalTrial, DTC, DoCM, DrugBank, Ensembl, Entrez, FDA, GuideToPharmacology, JAX-CKB, MyCancerGenome, MyCancerGenomeClinicalTrial, NCI, OncoKB, PharmGKB, TALC, TEND, TTD, TdgClinicalTrial, Wikidata). We queried protein targets for available active ligands in ChEMBL. We queried gene targets in the druggable genome using the most recent druggable genome list established by the NIH Illuminating the Druggable Genome Project (https://github.com/druggablegenome/IDGTargets) available through the Pharos web platform. We also queried FDA-approved drugs, late-stage clinical trials, and disease indications in the DrugBank, ChEMBL, ClinicalTrials.gov databases and provided results for the top MESH and DrugBank indications and clinical trials.
Data availability
All summary results are available in the GWAS Catalog with the following Accession IDs: AFR.HDLC.ANXT.2df (GCST90570645); AFR.HDLC.ANXT.1df (GCST90570646); AFR.HDLC.DEPR.2df (GCST90570647); AFR.HDLC.DEPR.1df (GCST90570648); AFR.HDLC.SOCS.2df (GCST90570649); AFR.HDLC.SOCS.1df (GCST90570650); AFR.LDLC.ANXT.2df (GCST90570651); AFR.LDLC.ANXT.1df (GCST90570652); AFR.LDLC.DEPR.2df (GCST90570653); AFR.LDLC.DEPR.1df (GCST90570654); AFR.TG.ANXT.2df (GCST90570655); AFR.TG.ANXT.1df (GCST90570656); AFR.TG.DEPR.2df (GCST90570657); AFR.TG.DEPR.1df (GCST90570658); ASN.HDLC.DEPR.2df (GCST90570659); ASN.HDLC.DEPR.1df (GCST90570660); ASN.LDLC.DEPR.2df (GCST90570661); ASN.LDLC.DEPR.1df (GCST90570662); ASN.TG.DEPR.2df (GCST90570663); ASN.TG.DEPR.1df (GCST90570664); EUR.HDLC.ANXT.2df (GCST90570665); EUR.HDLC.ANXT.1df (GCST90570666); EUR.HDLC.DEPR.2df (GCST90570667); EUR.HDLC.DEPR.1df (GCST90570668); EUR.HDLC.SOCS.2df (GCST90570669); EUR.HDLC.SOCS.1df (GCST90570670); EUR.LDLC.ANXT.2df (GCST90570671); EUR.LDLC.ANXT.1df (GCST90570672); EUR.LDLC.DEPR.2df (GCST90570673); EUR.LDLC.DEPR.1df (GCST90570674); EUR.LDLC.SOCS.2df (GCST90570675); EUR.LDLC.SOCS.1df (GCST90570676); EUR.TG.ANXT.2df (GCST90570677); EUR.TG.ANXT.1df (GCST90570678); EUR.TG.DEPR.2df (GCST90570679); EUR.TG.DEPR.1df (GCST90570680); EUR.TG.SOCS.2df (GCST90570681); EUR.TG.SOCS.1df (GCST90570682); HISP.HDLC.DEPR.2df (GCST90570683); HISP.HDLC.DEPR.1df (GCST90570684); HISP.HDLC.SOCS.2df (GCST90570685); HISP.HDLC.SOCS.1df (GCST90570686); HISP.LDLC.DEPR.2df (GCST90570687); HISP.LDLC.DEPR.1df (GCST90570688); HISP.LDLC.SOCS.2df (GCST90570689); HISP.LDLC.SOCS.1df (GCST90570690); HISP.TG.DEPR.2df (GCST90570691); HISP.TG.DEPR.1df (GCST90570692); HISP.TG.SOCS.2df (GCST90570693); HISP.TG.SOCS.1df (GCST90570694); CPMA.HDLC.ANXT.2df (GCST90570695); CPMA.HDLC.ANXT.1df (GCST90570696); CPMA.HDLC.DEPR.2df (GCST90570697); CPMA.HDLC.DEPR.1df (GCST90570698); CPMA.HDLC.SOCS.2df (GCST90570699); CPMA.HDLC.SOCS.1df (GCST90570700); CPMA.LDLC.ANXT.2df (GCST90570701); CPMA.LDLC.ANXT.1df (GCST90570702); CPMA.LDLC.DEPR.2df (GCST90570703); CPMA.LDLC.DEPR.1df (GCST90570704); CPMA.LDLC.SOCS.2df (GCST90570705); CPMA.LDLC.SOCS.1df (GCST90570706); CPMA.TG.ANXT.2df (GCST90570707); CPMA.TG.ANXT.1df (GCST90570708); CPMA.TG.DEPR.2df (GCST90570709); CPMA.TG.DEPR.1df (GCST90570710); CPMA.TG.SOCS.2df (GCST90570711); CPMA.TG.SOCS.1df (GCST90570712)
References
Graham SE, Clarke SL, Wu K-HH, Kanoni S, Zajac GJM, Ramdas S, et al. The power of genetic diversity in genome-wide association studies of lipids. Nature. 2021;600:675–9. https://doi.org/10.1038/s41586-021-04064-3.
Hoffmann TJ, Theusch E, Haldar T, Ranatunga DK, Jorgenson E, Medina MW, et al. A large electronic-health-record-based genome-wide study of serum lipids. Nat Genet. 2018;50:401–13. https://doi.org/10.1038/s41588-018-0064-5.
Klarin D, Damrauer SM, Cho K, Sun YV, Teslovich TM, Honerlaw J, et al. Genetics of blood lipids among ~300,000 multi-ethnic participants of the Million Veteran Program. Nat Genet. 2018;50:1514–23. https://doi.org/10.1038/s41588-018-0222-9.
Psaty BM, O’Donnell CJ, Gudnason V, Lunetta KL, Folsom AR, Rotter JI, et al. Cohorts for Heart and Aging Research in Genomic Epidemiology (CHARGE) Consortium: design of prospective meta-analyses of genome-wide association studies from 5 cohorts. Circ Cardiovasc Genet. 2009;2:73–80. https://doi.org/10.1161/CIRCGENETICS.108.829747.
Rao DC, Sung YJ, Winkler TW, Schwander K, Borecki I, Cupples LA, et al. Multiancestry study of gene-lifestyle interactions for cardiovascular traits in 610 475 individuals from 124 cohorts: design and rationale. Circ Cardiovasc Genet. 2017;10:e001649 https://doi.org/10.1161/CIRCGENETICS.116.001649.
Bentley AR, Sung YJ, Brown MR, Winkler TW, Kraja AT, Ntalla I, et al. Multi-ancestry genome-wide gene-smoking interaction study of 387,272 individuals identifies new loci associated with serum lipids. Nat Genet. 2019;51:636–48. https://doi.org/10.1038/s41588-019-0378-y.
Kilpelainen TO, Bentley AR, Noordam R, Sung YJ, Schwander K, Winkler TW, et al. Multi-ancestry study of blood lipid levels identifies four loci interacting with physical activity. Nat Commun. 2019;10:376 https://doi.org/10.1038/s41467-018-08008-w.
de Vries PS, Brown MR, Bentley AR, Sung YJ, Winkler TW, Ntalla I, et al. Multiancestry genome-wide association study of lipid levels incorporating gene-alcohol interactions. Am J Epidemiol. 2019;188:1033–54. https://doi.org/10.1093/aje/kwz005.
de Las Fuentes L, Schwander KL, Brown MR, Bentley AR, Winkler TW, Sung YJ, et al. Gene-educational attainment interactions in a multi-population genome-wide meta-analysis identify novel lipid loci. Front Genet. 2023;14:1235337 https://doi.org/10.3389/fgene.2023.1235337.
Noordam R, Bos MM, Wang H, Winkler TW, Bentley AR, Kilpeläinen TO, et al. Multi-ancestry sleep-by-SNP interaction analysis in 126,926 individuals reveals lipid loci stratified by sleep duration. Nat Commun. 2019;10:5121 https://doi.org/10.1038/s41467-019-12958-0.
Carney RM, Freedland KE. Depression and coronary heart disease. Nat Rev Cardiol. 2017;14:145–55. https://doi.org/10.1038/nrcardio.2016.181.
Juonala M, Pulkki-Råback L, Elovainio M, Hakulinen C, Magnussen CG, Sabin MA, et al. Childhood psychosocial factors and coronary artery calcification in adulthood: the cardiovascular risk in young finns study. JAMA Pediatrics. 2016;170:466–72. https://doi.org/10.1001/jamapediatrics.2015.4121.
Harshfield EL, Pennells L, Schwartz JE, Willeit P, Kaptoge S, Bell S, et al. Association between depressive symptoms and incident cardiovascular diseases. JAMA. 2020;324:2396–405. https://doi.org/10.1001/jama.2020.23068.
Li GH, Cheung CL, Chung AK, Cheung BM, Wong IC, Fok MLY, et al. Evaluation of bi-directional causal association between depression and cardiovascular diseases: a Mendelian randomization study. Psychol Med. 2022;52:1765–76. https://doi.org/10.1017/s0033291720003566.
Wei YG, Cai DB, Liu J, Liu RX, Wang SB, Tang YQ, et al. Cholesterol and triglyceride levels in first-episode patients with major depressive disorder: a meta-analysis of case-control studies. J Affect Disord. 2020;266:465–72. https://doi.org/10.1016/j.jad.2020.01.114.
Tkachev A, Stekolshchikova E, Vanyushkina A, Zhang H, Morozova A, Zozulya S, et al. Lipid alteration signature in the blood plasma of individuals with schizophrenia, depression, and bipolar disorder. JAMA Psychiatry. 2023;80:250–9. https://doi.org/10.1001/jamapsychiatry.2022.4350.
Bot M, Milaneschi Y, Al-Shehri T, Amin N, Garmaeva S, Onderwater GLJ, et al. Metabolomics profile in depression: a pooled analysis of 230 metabolic markers in 5283 cases with depression and 10,145 controls. Biol Psychiatry. 2020;87:409–18. https://doi.org/10.1016/j.biopsych.2019.08.016.
Brydges CR, Bhattacharyya S, Dehkordi SM, Milaneschi Y, Penninx B, Jansen R, et al. Metabolomic and inflammatory signatures of symptom dimensions in major depression. Brain, Behavior, Immun. 2022;102:42–52. https://doi.org/10.1016/j.bbi.2022.02.003.
Xu C, Padilla V, Lozano S, Gamez D, Su BB, Wang X, et al. APOE gene associated with dementia-related traits, depression, and anxiety in the hispanic population. Genes. 2023;14:1405.
Wang WW, Liu XL, Ruan Y, Wang L, Bao TH. Depression was associated with apolipoprotein E ε4 allele polymorphism: A meta-analysis. Iran J Basic Med Sci. 2019;22:112–7. https://doi.org/10.22038/ijbms.2018.30825.7436.
Zhang M, Chen J, Yin Z, Wang L, Peng L. The association between depression and metabolic syndrome and its components: a bidirectional two-sample Mendelian randomization study. Transl Psychiatry. 2021;11:633 https://doi.org/10.1038/s41398-021-01759-z.
Dregan A, Rayner L, Davis KAS, Bakolis I, Arias de la Torre J, Das-Munshi J, et al. Associations between depression, arterial stiffness, and metabolic syndrome among adults in the UK Biobank Population Study: a mediation analysis. JAMA Psychiatry. 2020;77:598–606. https://doi.org/10.1001/jamapsychiatry.2019.4712.
Datta BK, Coughlin SS, Gummadi A, Mehrabian D, Ansa BE. Perceived social support and cardiovascular risk among nonelderly adults in the United States. Am J Cardiol. 2023;209:146–53. https://doi.org/10.1016/j.amjcard.2023.09.106.
García-Ulloa AC, Miranda-Gil V, Díaz-Pineda M, Garnica-Carrillo MF, Serrano-Pérez NH, Tron-Gomez MS, et al. Comparison of metabolic, lifestyle and mental health parameters in people with diabetes and relatives with and without family support. Diabetes Metab Syndr Obes: Targets Ther. 2024;17:239–45. https://doi.org/10.2147/dmso.S445890.
Skogberg N, Castaneda AE, Agyemang C, Koponen P, Lilja E, Laatikainen T. The association of depressive and anxiety symptoms with the metabolic syndrome and its components among Russian, Somali, and Kurdish origin adults in Finland: a population-based study. J Psychosom Res. 2022;159:110944 https://doi.org/10.1016/j.jpsychores.2022.110944.
Milaneschi Y, Simmons WK, van Rossum EFC, Penninx BWJH. Depression and obesity: evidence of shared biological mechanisms. Mol Psychiatry. 2019;24:18–33. https://doi.org/10.1038/s41380-018-0017-5.
Zou L, Tian Y, Wang Y, Chen D, Lu X, Zeng Z, et al. High-cholesterol diet promotes depression- and anxiety-like behaviors in mice by impact gut microbe and neuroinflammation. J Affect Disord. 2023;327:425–38. https://doi.org/10.1016/j.jad.2023.01.122.
Yu H, Qin X, Yu Z, Chen Y, Tang L, Shan W. Effects of high-fat diet on the formation of depressive-like behavior in mice. Food Funct. 2021;12:6416–31. https://doi.org/10.1039/D1FO00044F.
Cheng B, Cheng S, Jia Y, Liu L, Meng P, Qi X, et al. Genome-wide association studies in non-anxiety individuals identified novel risk loci for depression. Eur Psychiatry. 2022;65:e38 https://doi.org/10.1192/j.eurpsy.2022.32.
Meng P, Ye J, Chu X, Cheng B, Cheng S, Liu L, et al. Associations between genetic loci, environment factors and mental disorders: a genome-wide survival analysis using the UK Biobank data. Transl Psychiatry. 2022;12:17 https://doi.org/10.1038/s41398-022-01782-8.
Pinakhina D, Yermakovich D, Vergasova E, Kasyanov E, Rukavishnikov G, Rezapova V, et al. GWAS of depression in 4520 individuals from the Russian population highlights the role of MAGI2 (S-SCAM) in the gut-brain axis. Front Genet. 2023;13:972196 https://doi.org/10.3389/fgene.2022.972196.
Schoeler T, Speed D, Porcu E, Pirastu N, Pingault J-B, Kutalik Z. Participation bias in the UK Biobank distorts genetic associations and downstream analyses. Nat Hum Behav. 2023;7:1216–27. https://doi.org/10.1038/s41562-023-01579-9.
Silveira PP, Pokhvisneva I, Howard DM, Meaney MJ. A sex-specific genome-wide association study of depression phenotypes in UK Biobank. Mol Psychiatry. 2023;28:2469–79. https://doi.org/10.1038/s41380-023-01960-0.
Do R, Willer CJ, Schmidt EM, Sengupta S, Gao C, Peloso GM, et al. Common variants associated with plasma triglycerides and risk for coronary artery disease. Nat Genet. 2013;45:1345–52. https://doi.org/10.1038/ng.2795.
Lanktree MB, Elbers CC, Li Y, Zhang G, Duan Q, Karczewski KJ, et al. Genetic meta-analysis of 15,901 African Americans identifies variation in EXOC3L1 is associated with HDL concentration[S]. J Lipid Res. 2015;56:1781–6. https://doi.org/10.1194/jlr.P059477.
Peloso GM, Auer PL, Bis JC, Voorman A, Morrison AC, Stitziel NO, et al. Association of low-frequency and rare coding-sequence variants with blood lipids and coronary heart disease in 56,000 whites and blacks. Am J Hum Genet. 2014;94:223–32. https://doi.org/10.1016/j.ajhg.2014.01.009.
Spracklen CN, Chen P, Kim YJ, Wang X, Cai H, Li S, et al. Association analyses of East Asian individuals and trans-ancestry analyses with European individuals reveal new loci associated with cholesterol and triglyceride levels. Hum Mol Genet. 2017;26:1770–84. https://doi.org/10.1093/hmg/ddx062.
Teslovich TM, Musunuru K, Smith AV, Edmondson AC, Stylianou IM, Koseki M, et al. Biological, clinical and population relevance of 95 loci for blood lipids. Nature. 2010;466:707–13. https://doi.org/10.1038/nature09270.
Willer CJ, Schmidt EM, Sengupta S, Peloso GM, Gustafsson S, Kanoni S, et al. Discovery and refinement of loci associated with lipid levels. Nat Genet. 2013;45:1274–83. https://doi.org/10.1038/ng.2797.
Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science. 2015;348:648–60. https://doi.org/10.1126/science.1262110.
GTEx Consortium. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science. 2015;348:648–60. https://doi.org/10.1126/science.1262110.
Kavousi M, Bos MM, Barnes HJ, Lino Cardenas CL, Wong D, Lu H, et al. Multi-ancestry genome-wide study identifies effector genes and druggable pathways for coronary artery calcification. Nat Genet. 2023;55:1651–64. https://doi.org/10.1038/s41588-023-01518-4.
de Las Fuentes L, Sung YJ, Sitlani CM, Avery CL, Bartz TM, Keyser C, et al. Genome-wide meta-analysis of variant-by-diuretic interactions as modulators of lipid traits in persons of European and African ancestry. Pharmacogenomics J. 2020;20:482–93. https://doi.org/10.1038/s41397-019-0132-y.
Montasser ME, Aslibekyan S, Srinivasasainagendra V, Tiwari HK, Patki A, Bagheri M, et al. An Amish founder population reveals rare-population genetic determinants of the human lipidome. Commun Biol. 2022;5:334 https://doi.org/10.1038/s42003-022-03291-2.
Rao S, Baranova A, Yao Y, Wang J, Zhang F. Genetic relationships between attention-deficit/hyperactivity disorder, autism spectrum disorder, and intelligence. Neuropsychobiology. 2022;81:484–96. https://doi.org/10.1159/000525411.
Karlsson Linnér R, Mallard TT, Barr PB, Sanchez-Roige S, Madole JW, Driver MN, et al. Multivariate analysis of 1.5 million people identifies genetic associations with traits related to self-regulation and addiction. Nat Neurosci. 2021;24:1367–76. https://doi.org/10.1038/s41593-021-00908-3.
Jansen PR, Watanabe K, Stringer S, Skene N, Bryois J, Hammerschlag AR, et al. Genome-wide analysis of insomnia in 1,331,010 individuals identifies new risk loci and functional pathways. Nat Genet. 2019;51:394–403. https://doi.org/10.1038/s41588-018-0333-3.
Karlsson Linnér R, Biroli P, Kong E, Meddens SFW, Wedow R, Fontana MA, et al. Genome-wide association analyses of risk tolerance and risky behaviors in over 1 million individuals identify hundreds of loci and shared genetic influences. Nat Genet. 2019;51:245–57. https://doi.org/10.1038/s41588-018-0309-3.
Kushima I, Imaeda M, Tanaka S, Kato H, Oya-Ito T, Nakatochi M, et al. Contribution of copy number variations to the risk of severe eating disorders. Psychiatry Clin Neurosci. 2022;76:423–8. https://doi.org/10.1111/pcn.13430.
Anney RJL, Ripke S, Anttila V, Grove J, Holmans P, Huang H, et al. Meta-analysis of GWAS of over 16,000 individuals with autism spectrum disorder highlights a novel locus at 10q24.32 and a significant overlap with schizophrenia. Mol Autism. 2017;8:21 https://doi.org/10.1186/s13229-017-0137-9.
Bacchelli E, Cameli C, Viggiano M, Igliozzi R, Mancini A, Tancredi R, et al. An integrated analysis of rare CNV and exome variation in Autism Spectrum Disorder using the Infinium PsychArray. Sci Rep. 2020;10:3198 https://doi.org/10.1038/s41598-020-59922-3.
Wu Y, Cao H, Baranova A, Huang H, Li S, Cai L, et al. Multi-trait analysis for genome-wide association study of five psychiatric disorders. Transl Psychiatry. 2020;10:209 https://doi.org/10.1038/s41398-020-00902-6.
Bigdeli TB, Fanous AH, Li Y, Rajeevan N, Sayward F, Genovese G, et al. Genome-wide association studies of schizophrenia and bipolar disorder in a diverse cohort of US veterans. Schizophrenia Bull. 2021;47:517–29. https://doi.org/10.1093/schbul/sbaa133.
Everson TM, Marsit CJ, Michael O’Shea T, Burt A, Hermetz K, Carter BS, et al. Epigenome-wide analysis identifies genes and pathways linked to neurobehavioral variation in preterm infants. Sci Rep. 2019;9:6322 https://doi.org/10.1038/s41598-019-42654-4.
Crawford K, Oliver PL, Agnew T, Hunn BHM, Ahel I. Behavioural characterisation of Macrod1 and Macrod2 knockout mice. Cells. 2021;10:368.
Hill WD, Marioni RE, Maghzian O, Ritchie SJ, Hagenaars SP, McIntosh AM, et al. A combined analysis of genetically correlated traits identifies 187 loci and a role for neurogenesis and myelination in intelligence. Mol Psychiatry. 2019;24:169–81. https://doi.org/10.1038/s41380-017-0001-5.
Davies G, Lam M, Harris SE, Trampush JW, Luciano M, Hill WD, et al. Study of 300,486 individuals identifies 148 independent genetic loci influencing general cognitive function. Nat Commun. 2018;9:2098 https://doi.org/10.1038/s41467-018-04362-x.
Lee JJ, Wedow R, Okbay A, Kong E, Maghzian O, Zacher M, et al. Gene discovery and polygenic prediction from a genome-wide association study of educational attainment in 1.1 million individuals. Nat Genet. 2018;50:1112–21. https://doi.org/10.1038/s41588-018-0147-3.
Fan CC, Loughnan R, Makowski C, Pecheva D, Chen C-H, Hagler DJ, et al. Multivariate genome-wide association study on tissue-sensitive diffusion metrics highlights pathways that shape the human brain. Nat Commun. 2022;13:2423 https://doi.org/10.1038/s41467-022-30110-3.
van der Meer D, Kaufmann T, Shadrin AA, Makowski C, Frei O, Roelfs D, et al. The genetic architecture of human cortical folding. Sci Adv. 2021;7:eabj9446 https://doi.org/10.1126/sciadv.abj9446.
Sha Z, Schijven D, Carrion-Castillo A, Joliot M, Mazoyer B, Fisher SE, et al. The genetic architecture of structural left–right asymmetry of the human brain. Nat Hum Behav. 2021;5:1226–39. https://doi.org/10.1038/s41562-021-01069-w.
Smith SM, Douaud G, Chen W, Hanayik T, Alfaro-Almagro F, Sharp K, et al. An expanded set of genome-wide association studies of brain imaging phenotypes in UK Biobank. Nat Neurosci. 2021;24:737–45. https://doi.org/10.1038/s41593-021-00826-4.
Shadrin AA, Kaufmann T, van der Meer D, Palmer CE, Makowski C, Loughnan R, et al. Vertex-wise multivariate genome-wide association study identifies 780 unique genetic loci associated with cortical morphology. Neuroimage. 2021;244:118603 https://doi.org/10.1016/j.neuroimage.2021.118603.
Lam M, Chen C-Y, Li Z, Martin AR, Bryois J, Ma X, et al. Comparative genetic architectures of schizophrenia in East Asian and European populations. Nat Genet. 2019;51:1670–8. https://doi.org/10.1038/s41588-019-0512-x.
Periyasamy S, John S, Padmavati R, Rajendren P, Thirunavukkarasu P, Gratten J, et al. Association of schizophrenia risk with disordered niacin metabolism in an indian genome-wide association study. JAMA Psychiatry. 2019;76:1026–34. https://doi.org/10.1001/jamapsychiatry.2019.1335.
Pardiñas AF, Holmans P, Pocklington AJ, Escott-Price V, Ripke S, Carrera N, et al. Common schizophrenia alleles are enriched in mutation-intolerant genes and in regions under strong background selection. Nat Genet. 2018;50:381–9. https://doi.org/10.1038/s41588-018-0059-2.
Ikeda M, Takahashi A, Kamatani Y, Momozawa Y, Saito T, Kondo K, et al. Genome-wide association study detected novel susceptibility genes for schizophrenia and shared trans-populations/diseases genetic effect. Schizophrenia Bull. 2019;45:824–34. https://doi.org/10.1093/schbul/sby140.
Trubetskoy V, Pardiñas AF, Qi T, Panagiotaropoulou G, Awasthi S, Bigdeli TB, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502–8. https://doi.org/10.1038/s41586-022-04434-5.
Li Z, Chen J, Yu H, He L, Xu Y, Zhang D, et al. Genome-wide association analysis identifies 30 new susceptibility loci for schizophrenia. Nat Genet. 2017;49:1576–83. https://doi.org/10.1038/ng.3973.
Hall J. Schizophrenia — an anxiety disorder? Br J Psychiatry. 2017;211:262–3. https://doi.org/10.1192/bjp.bp.116.195370.
Bulbena A, Bulbena-Cabre A. Schizophrenia and anxiety: yes, they are relatives not just neighbours. Br J Psychiatry. 2018;213:498–498. https://doi.org/10.1192/bjp.2018.126.
Naito T, Saheki Y. GRAMD1-mediated accessible cholesterol sensing and transport. Biochimica et Biophysica Acta - Mol Cell Biol Lipids. 2021;1866:158957 https://doi.org/10.1016/j.bbalip.2021.158957.
Ercan B, Naito T, Koh DHZ, Dharmawan D, Saheki Y. Molecular basis of accessible plasma membrane cholesterol recognition by the GRAM ___domain of GRAMD1b. EMBO J. 2021;40:e106524 https://doi.org/10.15252/embj.2020106524.
Ferrari A, Whang E, Xiao X, Kennelly JP, Romartinez-Alonso B, Mack JJ, et al. Aster-dependent nonvesicular transport facilitates dietary cholesterol uptake. Science. 2023;382:eadf0966 https://doi.org/10.1126/science.adf0966.
Aragam KG, Jiang T, Goel A, Kanoni S, Wolford BN, Atri DS, et al. Discovery and systematic characterization of risk variants and genes for coronary artery disease in over a million participants. Nat Genet. 2022;54:1803–15. https://doi.org/10.1038/s41588-022-01233-6.
Kichaev G, Bhatia G, Loh PR, Gazal S, Burch K, Freund MK, et al. Leveraging polygenic functional enrichment to improve GWAS power. Am J Hum Genet. 2019;104:65–75. https://doi.org/10.1016/j.ajhg.2018.11.008.
Moreno-Navarrete JM, Jove M, Ortega F, Xifra G, Ricart W, Obis È, et al. Metabolomics uncovers the role of adipose tissue PDXK in adipogenesis and systemic insulin sensitivity. Diabetologia. 2016;59:822–32. https://doi.org/10.1007/s00125-016-3863-1.
Sung YJ, de las Fuentes L, Winkler TW, Chasman DI, Bentley AR, Kraja AT, et al. A multi-ancestry genome-wide study incorporating gene–smoking interactions identifies multiple new loci for pulse pressure and mean arterial pressure. Hum Mol Genet. 2019;28:2615–33. https://doi.org/10.1093/hmg/ddz070.
Sung YJ, Winkler TW, de las Fuentes L, Bentley AR, Brown MR, Kraja AT, et al. A large-scale multi-ancestry genome-wide study accounting for smoking behavior identifies multiple significant loci for blood pressure. Am J Hum Genet. 2018;102:375–400. https://doi.org/10.1016/j.ajhg.2018.01.015.
Amare AT, Vaez A, Hsu YH, Direk N, Kamali Z, Howard DM, et al. Bivariate genome-wide association analyses of the broad depression phenotype combined with major depressive disorder, bipolar disorder or schizophrenia reveal eight novel genetic loci for depression. Mol Psychiatry. 2020;25:1420–9. https://doi.org/10.1038/s41380-018-0336-6.
Backman JD, Li AH, Marcketta A, Sun D, Mbatchou J, Kessler MD, et al. Exome sequencing and analysis of 454,787 UK Biobank participants. Nature. 2021;599:628–34. https://doi.org/10.1038/s41586-021-04103-z.
Li QS, Tian C, Hinds D. Genome-wide association studies of antidepressant class response and treatment-resistant depression. Transl Psychiatry. 2020;10:360 https://doi.org/10.1038/s41398-020-01035-6.
Mitchell BL, Campos AI, Whiteman DC, Olsen CM, Gordon SD, Walker AJ, et al. The Australian genetics of depression study: new risk loci and dissecting heterogeneity between subtypes. Biol Psychiatry. 2022;92:227–35. https://doi.org/10.1016/j.biopsych.2021.10.021.
Yakovchik AY, Tolynyova DV, Kashtanova DA, Sutulova ER, Ivanov MV, Mamchur AA, et al. Genetics of psycho-emotional well-being: genome-wide association study and polygenic risk score analysis. Front Psychiatry. 2023;14:1188427 https://doi.org/10.3389/fpsyt.2023.1188427.
Wang H, Noordam R, Cade BE, Schwander K, Winkler TW, Lee J, et al. Multi-ancestry genome-wide gene–sleep interactions identify novel loci for blood pressure. Mol Psychiatry. 2021;26:6293–304. https://doi.org/10.1038/s41380-021-01087-0.
Feitosa MF, Kraja AT, Chasman DI, Sung YJ, Winkler TW, Ntalla I, et al. Novel genetic associations for blood pressure identified via gene-alcohol interaction in up to 570K individuals across multiple ancestries. PLoS ONE. 2018;13:e0198166 https://doi.org/10.1371/journal.pone.0198166.
Bucciarelli V, Caterino AL, Bianco F, Caputi CG, Salerni S, Sciomer S, et al. Depression and cardiovascular disease: The deep blue sea of women’s heart. Trends Cardiovasc Med. 2020;30:170–6. https://doi.org/10.1016/j.tcm.2019.05.001.
Xu L, Wang K, Wang S, Liu L, Lv X, Song Y. Sex differences in the association between serum lipids and depressive symptoms: a longitudinal population-based study. J Affect Disord. 2021;291:154–62. https://doi.org/10.1016/j.jad.2021.05.011.
Blakoe M, Petrova D, Garcia-Retamero R, Gonçalves K, Catena A, Ramírez Hernández JA, et al. Sex moderates the relationship between social support and cardiovascular prevention behaviors in middle-aged and older adults. Ann Behav Med. 2023;57:877–87. https://doi.org/10.1093/abm/kaad030.
Olfson M, Marcus SC, Corey-Lisle P, Tuomari AV, Hines P, L’Italien GJ. Hyperlipidemia following treatment with antipsychotic medications. Am J Psychiatry. 2006;163:1821–5. https://doi.org/10.1176/ajp.2006.163.10.1821.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Kraft P, Yen YC, Stram DO, Morrison J, Gauderman WJ. Exploiting gene-environment interaction to detect genetic associations. Hum Heredity. 2007;63:111–9. https://doi.org/10.1159/000099183.
Aulchenko YS, Struchalin MV, van Duijn CM. ProbABEL package for genome-wide association analysis of imputed data. BMC Bioinforma. 2010;11:134 https://doi.org/10.1186/1471-2105-11-134.
Winkler TW, Day FR, Croteau-Chonka DC, Wood AR, Locke AE, Magi R, et al. Quality control and conduct of genome-wide association meta-analyses. Nat Protoc. 2014;9:1192–212. https://doi.org/10.1038/nprot.2014.071.
Manning AK, LaValley M, Liu CT, Rice K, An P, Liu Y, et al. Meta-analysis of gene-environment interaction: joint estimation of SNP and SNP x environment regression coefficients. Genet Epidemiol. 2011;35:11–18. https://doi.org/10.1002/gepi.20546.
Willer CJ, Li Y, Abecasis GR. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics. 2010;26:2190–1. https://doi.org/10.1093/bioinformatics/btq340.
Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat Commun. 2017;8:1826 https://doi.org/10.1038/s41467-017-01261-5.
Kircher M, Witten DM, Jain P, O’Roak BJ, Cooper GM, Shendure J. A general framework for estimating the relative pathogenicity of human genetic variants. Nat Genet. 2014;46:310–5. https://doi.org/10.1038/ng.2892.
Ernst J, Kellis M. ChromHMM: automating chromatin-state discovery and characterization. Nat Methods. 2012;9:215–6. https://doi.org/10.1038/nmeth.1906.
Zhu Z, Zhang F, Hu H, Bakshi A, Robinson MR, Powell JE, et al. Integration of summary data from GWAS and eQTL studies predicts complex trait gene targets. Nat Genet. 2016;48:481–7. https://doi.org/10.1038/ng.3538.
Acknowledgements
This project was largely supported by two grants from the U.S. National Heart, Lung, and Blood Institute (NHLBI), the National Institutes of Health, R01HL118305 and R01HL156991. This research was supported in part by the Intramural Research Program of the National Human Genome Research Institute (NHGRI) in the Center for Research on Genomics and Global Health (CRGGH—Z01HG200362). CRGGH is also supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Center for Information Technology, and the Office of the Director at the National Institutes of Health. Tuomas O. Kilpeläinen was supported by grants from the Novo Nordisk Foundation (NNF18CC0034900, NNF21SA0072102, NNF22OC0074128, NNF23SA0084103). W. Jim Gauderman was supported by the National Cancer Institute (NCI; P01 CA196569). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of NHLBI, NHGRI, the NCI; the National Institutes of Health; or the U.S. Department of Health and Human Services. Study-specific acknowledgments are included in the Supplementary Note. The authors gratefully acknowledge the invaluable contributions of Adolfo Correa, Lisa W. Martin, Annette Peters, and Astrid Petersmann. The authors would also like to recognize L. Adrienne Cupples, Diane M. Becker, and John M. Starr, who participated in this effort, but passed away prior to the completion of the manuscript.
Funding
Open access funding provided by the National Institutes of Health.
Author information
Authors and Affiliations
Consortia
Contributions
ARB and SKM drafted the manuscript with substantial contributions from MRB, KLS, TWW, CLM, DCR, CNR, MF, and ERF. HA, ARB, MRB, LFB, MF, MFF, ERF, LdlF, JG, ATK, TOK, C-TL, CLM, AKM, SKM, RN, JRO’C, MProvince, BMP, PAP, DCR, KR, SSR, CNR, YJS, KLS, PSdV, TWW, XZhu contributed to the conception and design of the work. HA, NA, DEA, DKA, ARB, MRB, LB, TMB, CB, EB, Y-DIC, J-FC, KNC, MLD, KWvD, JACD, IJD, CMvD, LE, MKE, JDF, AMF, NF, MF, ERF, MFF, VG, LCG, MG, XG, CG, HJG, CAH, DvH, FPH, GH, ARVRH, SEH, SH, MAI, CRI, JBJ, LK-J, PK, SLRK, CK, JEK, C-TL, JL, KL, TAL, TL, LL, L-PL, EL, YL, D-OMK, CLM, ACM, AKM, AWM, SKM, PJvdM, PM-V, SEM, YM, IMN, RN, KEN, AJO, BWJHP, ACP, PAP, MPreisig, GP, CNR, MAR, JIR, RR, DCR, XS, PJS, LS, JMS, X-oS, JAS, HS, NS, KLS, MS, AVS, KDT, LT, MYT, AGU, DV, EW, MW, GW, SW, Y-XW, RBW, H-LW, DRW, W-BW, RW, WW, YW, JY, LRY, XZhang, XZhu, WZheng, WZhao, ABZ contributed in the acquisition, analysis, or interpretation of the data. MRB conducted centralized data cleaning and meta-analyses. TWW designed the software pipeline used for harmonization, visualization, and quality control of study data. DEA, HA, TMB, LFB, EB, KNC, JACD, LE, MKE, MFF, NF, AMF, LdlF, MG, JG, LG, HJG, ARVRH, DvH, SEH, CRI, MAI, ATK, C-TL, AIL, L-PL, PM-V, YM, SEM, RN, JRO’C, AJO, PAP, GP, MPreisig, MProvince, BP, KR, SSR, JIR, JAS, JMS, PJS, X-oS, EST, LT, PSdV, RBW, SW, H-LW, KLY, LRY, WZheng, WZhao, XZhu made substantial revisions to the manuscript. All authors approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare the following competing interests: BMP serves on the Data and Safety Monitoring Board of a clinical trial funded by the manufacturer (Zoll LifeCor) and on the Steering Committee of the Yale Open Data Access Project funded by Johnson & Johnson; CMvD was sponsored by GlaxoSmithKline; HJG received travel grants and speakers honoraria from Fresenius Medical Care, Neuraxpharm and Janssen Cilag as well as research funding from Fresenius Medical Care; JBJ serves in the Advisory Board Novartis; Patent holder with Biocompatibles UK Ltd. (Franham, Surrey, UK) (Title: Treatment of eye diseases using encapsulated cells encoding and secreting neuroprotective factor and / or anti-angiogenic factor; Patent number: 20120263794), and Europäische Patentanmeldung 16 720 043.5 and Patent application US 2019 0085065 A1 (Agents for use in the therapeutic or prophylactic treatment of myopia or hyperopia).
Ethics Approval and Consent to Participate
For all participating cohorts, the appropriate institutional review boards approved research activities and informed consent was obtained from each participant. Further details on all participating cohorts is given in the Supplementary Note.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bentley, A.R., Brown, M.R., Musani, S.K. et al. Multi-ancestry genome-wide association analyses incorporating SNP-by-psychosocial interactions identify novel loci for serum lipids. Transl Psychiatry 15, 207 (2025). https://doi.org/10.1038/s41398-025-03418-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03418-z