Abstract
Aim The hypothesis was tested that dentine carious lesion progression is higher in sealed micro-cavitated pits and fissures than in sealed pits and fissures having no or enamel carious lesions at baseline over a period of four years.
Results Epidemiological survey identified no enamel carious lesions (code 0), enamel carious lesions (code 1), and micro-cavitated dentine carious lesions (code 2), in pits/fissures of occlusal surfaces of first permanent molars at baseline. Using block randomisation, 405 children (mean age of eight years) were allocated to high-viscosity glass-ionomer, atraumatic restorative treatment method (HVGIC/ART), thermo-cured HVGIC/ART, glass-carbomer, and resin composite groups, receiving 1,344 sealants. Evaluation was performed after six months and annually. Carious lesion progression for baseline code 0 (n = 784) and code 1 (n = 481) was determined by scoring code 2, and that for baseline code 2 (n = 79) by scoring code 3 or 4 (frank cavitation). Tests were performed using a proportional hazard model with frailty correction.
Discussion and conclusion There was neither an effect for sealant group nor between baseline codes 0 and 1. A total of 19 baseline code 0, and 20 code 1 developed a cavitated dentine carious lesion; while 5% of the sealed over micro-cavitated dentine carious lesions developed frank cavitation. The progression of carious lesions in the group baseline code (0 + 1) was not statistically significantly different from the group of baseline code 2 (p = 0.29). Progression of micro-cavities sealed over with HVGIC according to the ART method, a glass-carbomer or a resin composite over a period of four years is low. Dentine lesions with a small orifice (Ø <0.5 mm) in pits/fissures of occlusal surfaces in permanent molars have a high chance of surviving four years if they are sealed over.
Similar content being viewed by others
Key points
-
Provides information on the extension of the indication for placing a sealant.
-
Highlights the CPI instrument as an easy to use measuring instrument in the decision to seal or to restore.
-
Further supports the concept of minimal intervention dentistry.
Introduction
Current management of dental caries is guided by the minimal intervention (MI) concept.1 The concept includes maintaining healthy, functional teeth through sealing high-caries risk pits and fissures systems that may contain enamel carious lesions. MI also deals with minimally invasive operative interventions for treating cavitated dentine carious lesions. In the past, such interventions were based on Black's principles of cavity design, removing sound and remineralisable tooth tissues in the process unnecessarily. In conjunction with adhesive restorative materials, MI based interventions have the potential for keeping cavitated dentine carious lesions relatively small, which maintains a high level of tooth integrity and increases the life of a restored tooth.
The stage at which a dentine carious lesion should be intervened invasively has shifted gradually from cavitation that is clearly visible to ambiguous micro-cavitation, with a very small opening.2,3 Instead of being restored, micro-cavities with a diameter of the orifice of < 0.9 mm were sealed.4,5 By sealing over the micro-cavity opening, plaque is prevented from penetrating the cavity and this stops the caries process from functioning, provided the sealant is well placed. This argument is accepted from a cariological point of view,6 but intervention success is also dependent on the mechanical properties of the sealant material used and level of oral hygiene of the patient.
According to an in vitro study, small cavitated dentine carious lesions in pits and fissures showed a higher level of microleakage and insufficient penetration of resin sealant material into the cavity, compared to sound pits and fissures.7 Furthermore, it is known that the retention of sealants deteriorates over time, which may lead to the re-exposure of the micro-cavity and may ignite the caries process again. However, it is also possible that the small cavity opening stays blocked with remnants of the sealant material, as shown for glass-ionomer cement.8,9
Few studies have reported the effectiveness of sealing micro-cavities in pits and fissures systems. The present secondary analysis, using data from a sealant trial in China,10 contributes to the understanding of the potential for sealing micro-cavities with a high-viscosity glass-ionomer (HVGIC) placed according to the ART method, a glass-carbomer and a resin composite sealant. The hypothesis tested was that dentine carious lesion progression is higher in sealed micro-cavitated pits and fissures than in sealed pits and fissures with no or enamel carious lesions at baseline over a period of four years.
Materials and methods
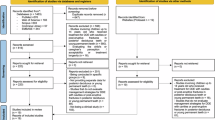
The main trial study was approved by the research ethics committee of Wuhan University, Reference No. 200,704, and was registered at the Dutch Trial Registration Centre, with Reference No. 1411. Children's parents or guardians received and signed individual informed consent forms that contained information about the aim of the study and the treatment procedures. Children whose parents declined to sign the consent form were excluded from the study. The methodology of the main trial, including the CONSORT diagram, has been published previously.10,11 Therefore, only a summary is presented in this article.
Study population and treatment allocation
The study was conducted in Wuhan, China in 2008. Prior to the study, an oral health epidemiological survey of grade two children attending five primary schools was conducted using the caries criteria described in Table 1. A follow-up survey was performed four years later. The inclusion criteria for the main trial enrolment were: a fully erupted first permanent molar, no dentine carious lesion in pits and fissures of these molars, deep and/or intermediate pits or fissures,12 and a mean dmft ≥2. However, at the four year data analyses, it was discovered that 102 occlusal surfaces had been sealed, against protocol, that contained a small dentine lesion with a cavity opening that the CPI probe (diameter of 0.5 mm) could not penetrate (caries code 2), at baseline.11
The main trial was randomised controlled. Per school, the principal investigator randomly allocated each child to one of the four sealant groups, using a list obtained after block-randomisation (12 children per block for three operators) that was prepared by a statistician who did not do the analyses. A four-week laboratory and field training programme in a primary school was carried out before the trial began as the sealant procedures were new to the three operating dentists and the two dental ancillaries who assisted them.
The sealants were placed in first permanent molars on the school premises using portable equipment over two months. Children received instructions about good oral health behaviour and how to clean their teeth. The operators provided emergency treatment at baseline. Teeth with failed sealants, dentine carious lesion in re-exposed pits and fissures with a cavity opening that the CPI probe could penetrate (caries code 3), were restored. Lost sealant material was not replaced.
Sealant procedures
HVGIC/ART group
The high-viscosity glass-ionomer Ketac Molar Easymix (3MESPE, Seefeld, Germany) was used. Sealant application followed the atraumatic restorative treatment (ART) sealant procedure.5
Thermo-cured HVGIC/ART group
The Ketac Molar Easymix was thermo-cured using the LED high-intensity curing light, Elipar Freelight 2 (3MESPE, Seefeld, Germany), producing 850 mW/cm2. The sealant application described for the HVGIC/ART group was followed, except that the sealant was cured for 60 seconds after burnishing.
Glass-carbomer group
A glass-ionomer-based material containing fluorapatite and powder particles reduced to nano size, Glass Carbomer (First Scientific Dental, Elmshorn, Germany), was used. Surface cleaning was done under cotton wool isolation as described for the HVGIC/ART group, followed by applying Glass Carbomer Tooth Cleaner over the tooth surface for 20 seconds and washing and drying the surface with two wet and dry cotton pellets respectively. The Glass Carbomer capsule was mixed for 15 seconds in Rotomix (3MESPE, Seefeld, Germany), extruded onto the tooth surface, spread into a thin film, covered with Glass Carbomer Surface Gloss (First Scientific Dental, Elmshorn, Germany) and held under finger pressure for 5-10 seconds. After bite adjustment, the material was light-cured for 75 seconds with the same LED lamp as used in the thermo-cured HVGIC/ART group.
Resin C Group
A resin composite, Clinpro (3MESPE, Minneapolis, USA), was used. The pits and fissures were cleaned with a rotating brush, Prophy Angle (3MESPE, Wuhan, China), and a no. 6 explorer, acid-etched with Scotchbond etchant (3MESPE, St. Pauls, Minneapolis, USA) for 20 seconds, and rinsed and dried using a portable suction machine. The sealant material was placed in the pits and fissures, manipulated with an explorer to free potential air bubbles and cured for 20 seconds with the LED curing light 1 mm above the surface. Carbon paper and rotary instruments were used in bite adjustment.
Evaluation
The coverage of the pits and fissures with sealant material was recorded at baseline. A dentine carious lesion was recorded clinically if the enamel surface appeared cavitated and the carious lesion judged to have involved the dentine (codes 2, 3, 4). The CPI probe was used as an aid for determining codes 2 and 3 (Table 1). Before examination, the sealed tooth surface was dried with a piece of cotton tightly attached to the end of a stick. The examination site was well illuminated by an intraoral light with attached disposable mirrors (Mirrorlight, Kudos, Hong Kong).
Four independent evaluators (dentists) were trained and calibrated by a senior epidemiologist (two at years 0.5, 1, and 2, and two at years 3 and 4). Training and calibration was performed by first explaining the evaluation criteria through the use of a PowerPoint presentation. Examining children by the two evaluators and the epidemiologist together at the school compound followed this. Thereafter, evaluators examined batches of three children independently. Assessment scores were compared after each batch and differences discussed until a consensus was reached. This process continued until evaluators were truly calibrated. Before and during the morning of the first day of each evaluation year, evaluators were recalibrated by examining the first arriving children twice. In the presence of the senior epidemiologist, differences in scores were discussed and consensus was reached. Final year dental students trained in recording data assisted the evaluators.
The children's caries status was reassessed one and a half years after sealants had been placed according to the caries assessment criteria used at baseline by two examiners, one of whom participated in the oral health epidemiological survey at baseline, and after three and a half years by other examiners, all trained and calibrated by the senior epidemiologist. The kappa-coefficient for inter-evaluator consistency for assessing caries lesions on tooth sections for evaluation years 0.5, 1, and 2, combined and evaluation years three and four combined were 0.63 and 0.86 respectively.
Statistical analyses
Data were analysed by a biostatistician (JM) using SAS software (version 9.2). All tests were carried out using a proportional hazard model with frailty correction (PHREG). The independent variables were 'baseline caries code' (0, 1, 2) and 'sealant procedure' (HVGIC/ART, thermo-cured HVGIC/ART, glass-carbomer, resin C). Background variables were gender, age and caries status in the primary dentition at baseline. Failure over four years (dependent variable) was defined as caries code ≥ 2 for baseline caries codes 0 and 1, and caries code 3 or 4 for baseline caries code 2. In this analysis, baseline caries codes 0 and 1 were tested against baseline caries code 2. A secondary analysis was performed in which caries code ≥2 for all three baseline caries codes was considered a failure. The difference between baseline caries codes 0 and 1 was ascertained using all data and all four sealant procedures in the model. Differences between D2MFS and D3MFS counts at baseline and four years for the four sealant procedures were tested using ANOVA. Statistical significance level was set at p = 0.05.
Results
Disposition of subjects
A total of 405 children, 215 boys and 190 girls, with an average age of 8.0 years (range 7.0-9.1 years) participated in the trial. In total, 1,344 first permanent molars were sealed divided over HVGIC/ART (312), thermo-cured HVGIC/ART (351), glass-carbomer (324) and resin C (357) groups. The trial number of children and sealants that dropped out over the four years was 12.3% and 15.4% respectively.
The mean d2mft (± SD) scores at baseline were 6.2 (± 2.8) for HVGIC/ART, 6.3 (± 2.9) for thermo-cured HVGIC/ART, 6.3 (± 2.8) for glass-carbomer and 6.4 (± 2.7) for resin C. The mean D2MFS and D3MFS scores and standard deviations by sealant group after four years are presented in Table 2.11 No difference in caries experience in the permanent dentition was observed between the four groups at baseline (D2MFS: p = 0.62; D3MFS: p = 0.59) and at the four-year evaluation (D2MFS: p = 0.45; D3MFS: p = 0.39).
There was a gender effect (p = 0.03) observed. Proportionally more cavitated dentine carious lesions were observed in girls than in boys. No age (p = 0.71), mean d2mft (p = 0.11) and mean d3mft (p = 0.17) effect on cavitated dentine carious lesion development in sealed occlusal surfaces of first permanent molars was observed at baseline.
Progression of dentine carious lesions over four years
The number of failed sealants (expressed as caries codes 3 and 4 = frank cavitation) for baseline caries code 2 over four years was: two (HVGIC/ART), one (Thermo-cured HVGIC/ART), 0 (glass-carbomer) and one (resin C). Progression of carious lesions was determined for baseline caries code 0 + 1 as the development of caries code ≥2 (failure); for baseline caries code 2 it was caries codes 3 and 4. The progression of carious lesions over the 4 years in the group baseline caries code 0 + 1 combined was not statistically significantly different from that in the group of baseline caries code 2 (p = 0.29). The hazard ratio was 0.57 (SE: 0.99).
Presence of cavitated dentine carious lesion by sealant procedure over four years
The number of survived and failed sealants over four years by sealant procedure and baseline caries score is presented in Table 3. A total of 47 sealed occlusal surfaces in first permanent molars (including eight sealants with baseline caries code 2) developed a cavitated dentine carious lesion over the four-year period. Using the PHREG model for determining the survival percentages of sealants with caries code ≥2 as failure, and baseline caries codes 0, 1 and 2 and sealant procedures as independent variables, showed no statistically significant difference between baseline caries codes 0 and 1 (p = 0.07). This outcome allowed combining the data of both baseline caries codes. Further analyses (PHREG) with the baseline caries code (0 + 1 and 2) and sealant procedure showed no statistically significant difference for the sealant procedure (p = 0.38). However, an effect of the baseline caries code (0 + 1) and baseline caries code 2 was observed (p = 0.002). The chance of developing a cavitated dentine carious lesion in the group baseline caries code (0 + 1) was 3% and in the group baseline caries code 2 it was 10%. The hazard ratio between the two groups of baseline caries codes was 0.276 (SE: 1.047), meaning that the risk for developing a cavitated dentine carious lesion (failure) over four years in occlusal surfaces of first permanent molars was about three times higher for the group baseline caries code 2 than for the group baseline caries code (0 + 1).
Discussion
The hypothesis was rejected. No significant difference in dentine carious lesion progression was found between sealed micro-cavitated pits and fissures at baseline and sealed pits and fissures with no or enamel carious lesions at baseline over a period of four years. The fact that only four of the 79 sealed micro-cavitated dentine carious lesions progressed from a small dentine carious lesion to frank cavitation over a four-year period supports the view that such dentine carious lesions do not necessarily need to be restored, as has been advocated.13 The type of sealant material did not influence the study finding. Progression of enamel/dentine carious lesions depends very much on the caries risk of the individual. In the present trial, caries experience of the, on average, 12-year-olds (four years after baseline epidemiological survey) was very low, showing that this child population had moved from a high-caries risk status at baseline to a low-caries risk status after four years. Carious lesion preventive instructions only were presented to the school children at the start of the trial and during each of the evaluation exercises. The schools had not instigated collective toothbrushing programmes. We are not aware of the toothbrushing pattern of the children nor the composition of their diet.
The number of studies that have investigated the effectiveness of sealing over micro-cavitated dentine carious lesions appears to be low. Comparing the findings of the present study with those of other studies is difficult because of differences in subject age, caries risk level, maximum opening of the orifice of the cavity, type of dentition and materials used, some of which are currently considered outdated.4,5,14,15 Compared to a failure rate of 12.6% after three years4 and 31.8% after five years5 of sealed over cavities with a diameter of the orifice of <0.9 mm in permanent molars, the result of the present study (5% of the micro-cavities sealed over progressed into a frank cavity after four years) is low. A major difference between these studies is the size of the orifice of the cavity, which was lowest in the present study. Further studies should investigate the effect of size of the cavity opening.
The present study also showed that the risk for developing a cavitated dentine carious lesion over four years in occlusal surfaces of first permanent molars is about three times (10% vs 3%) higher in occlusal surfaces with a cavitated dentine carious lesion at baseline than in those with no or an enamel carious lesion at baseline. This finding should be considered obvious, as a failed cavitated dentine carious lesion sealed over will re-expose such a dentine carious lesion in the occlusal surface. But it also implies that many of the cavitated dentine carious lesions sealed over remained unchanged with respect to its caries lesion level over four years. It means that the sealant intervention has contained the progression of cavitated dentine carious lesions (code 2) and made a more invasive restoration unnecessary. However, it is not known if the cavitated dentine carious lesions diagnosed are the same as those sealed over or whether they have been developed on the same surface but at a different spot. The present analysis did not distinguish the actual site of carious lesions, whether in enamel or in dentine and whether they were cavitated or non-cavitated. Therefore, in future studies colour photographs should accompany the clinical carious lesion assessment of occlusal surfaces.16,17,18
In the present study, no significant difference was observed in cavitated dentine carious lesion development over the four-year period between sealants with no and those with enamel carious lesions in occlusal surfaces sealed over at baseline. This finding corroborates the conclusion of a systematic review on this topic19 and implies that cutting away the signs of enamel carious lesions (enameloplasty) appears to be unnecessary20 and is considered overtreatment.21 The latter consideration has received support from a three-year long study among initially six- to seven-year-old high-caries risk children who had their high-caries risk occlusal surfaces either sealed with a resin composite or with a high-viscosity glass-ionomer according to the ART method in comparison with supervised toothbrushing during school time. The behavioural management of the occlusal surfaces by the child was as good as sealing these in preventing the development of cavitated dentine carious lesions.22
Conclusions
It is concluded that, in this child population, which moved from a high- to a low-caries risk status, the progression of micro-cavities sealed over with a high-viscosity glass-ionomer cement according to the ART method, a glass-carbomer or a resin composite, over a four-year period was low. It shows that sealants placed over micro-cavities have the ability to stop carious lesion progression. The type of sealant material appears less relevant.
References
Frencken J E, Peters M C, Manton D J, Leal S C, Gordan V V, Eden E. Minimal intervention dentistry for managing dental caries - a review: report of a FDI task group. Int Dent J 2012; 62: 223-243.
Mertz-Fairhurst E J, Curtis JW Jr, Ergle J W, Rueggeberg F A, Adair S M. Ultraconservative and cariostatic sealed restorations: results at year 10. J Am Dent Assoc 1998; 129: 55-66.
Bakhshandeh A, Qvist V, Ekstrand K R. Sealing occlusal carious lesions in adults referred for restorative treatment: 2-3 years of follow-up. Clin Oral Investig 2012; 16: 521-529.
Frencken J E, Makoni F, Sithole W D, Hackenitz E. Three-year survival of one-surface ART restorations and glass-ionomer sealants in a school oral health programme in Zimbabwe. Caries Res 1998; 32: 119-126.
Beiruti N, Frencken J E, van't Hof M A, Taifour D, van Palenstein Helderman W H. Caries-preventive effect of a one-time application of composite resin and glass ionomer sealants after 5 years. Caries Res 2006; 40: 52-59.
Kidd E A. How 'clean' must a cavity be before restoration? Caries Res 2004; 38: 305-313.
Hevinga MA, Opdam N J, Frencken JE, Bronkhorst E M, Truin G J. Can caries fissures be sealed as adequately as sound fissures? J Dent Res 2008; 87: 495-498.
Mejàre I, Mjör I A. Glass ionomer and resin-based fissure sealants: a clinical study. Scand J Dent Res 1990; 98: 345-350.
Frencken J E, Wolke J. Clinical and SEM assessment of ART high-viscosity glass-ionomer sealants after 8-13 years in 4 teeth. J Dent 2010; 38: 59-64.
Chen X, Du M Q, Fan M W, Mulder J, Huysmans M C, Frencken J E. Caries preventive effect of sealants produced with altered glass-ionomer materials after 2 years. Dent Mater 2012; 28: 554-560.
Zhang W, Chen X, Fan M W, Mulder J, Huysmans M C, Frencken J E. Do light cured ART conventional high-viscosity glass-ionomer sealants perform better than resin-composite sealants: a 4 year randomized clinical trial. Dent Mater 2014; 30: 487-492.
Symons A L, Chu C Y, Meyers I A. The effect of fissure morphology and pretreatment of the enamel surface on penetration and adhesion of fissure sealants. J Oral Rehabil 1996; 23: 791-798.
Ismail A I, Tellez M, Pitts N B et al. Caries management pathways preserve dental tissues and promote oral health. Community Dent Oral Epidemiol 2013; 41: e12-e40.
Mertz-Fairhurst E J, Schuster G S, Fairhurst C W. Arresting caries by sealants: results of a clinical study. J Am Dent Assoc 1986; 112: 194-197.
Fontana M, Platt J A, Eckert G J et al. Monitoring of sound and carious surfaces under sealants over 44 months. J Dent Res 2014; 93: 1070-1075.
Boye U, Walsh T, Pretty I A, Tickle M. Comparison of photographic and visual assessment of occlusal caries with histology as the reference standard. BMC Oral Health 2012; 12: 10.
Boye U, Willasey A, Walsh T, Tickle M, Pretty I A. Comparison of an intra-oral photographic caries assessment with an established visual caries assessment method for use in dental epidemiological studies of children. Community Dent Oral Epidemiol 2013; 41: 526-533.
Hu X, Fan M, Mulder J, Frencken J E. Are carious lesions in previously sealed occlusal surfaces detected as well from colour photographs as through visual clinical examination? Oral Health Prev Dent 2016; 14: 275-281.
Griffin S O, Oong E, Kohn W et al. The effectiveness of sealants in managing caries lesions. J Dent Res 2008; 87: 169-174.
Oong EM, Griffin S O, Kohn W G, Gooch B F, Caufield P W. The effect of dental sealants on bacteria levels in caries lesions: a review of the evidence. J Am Dent Assoc 2008; 139: 271-278.
Holmgren C, Gaucher C, Decerle N, Doméjean S. Minimal intervention dentistry II: part 3. Management of non-cavitated (initial) occlusal caries lesions - non-invasive approaches through remineralisation and therapeutic sealants. Br Dent J 2014; 216: 237-243.
Hilgert L A, Leal S C, Mulder J, Creugers N H, Frencken J E. Caries-preventive effect of supervised toothbrushing and sealants. J Dent Res 2015; 94: 1218-1224.
Author contributions , Acknowledgements and Declaration of conflict of interests
Author contributions
W. W. Zhang contributed to conception and interpretation and drafted the manuscript; J. Mulder contributed to data analysis and drafted the manuscript; J.E. Frencken contributed to conception, data analysis and interpretation, and drafted the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Acknowledgements
We thank Dr Ye Lu, Dr Li Jiqi and Dr Hu Xuan, the dental assistants, final-year students and evaluators for their pleasant and valuable contribution to the implementation and evaluation phases of the main trial. We appreciate the donation of dental materials from 3MESPE, China and Glass-Carbomer N.V., The Netherlands. The main trial was financed by grants from the Ministry of Science and Technology, China (2007BA128B00), the Netherlands Academy of Science (08CDP011) and the Radboud University Nijmegen (RL000045), The Netherlands.
Declaration of conflict of interests
The authors declare no potential conflict of interests with respect to the authorship and/or publication of this article. We thank Mrs. S. van Tonder for editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, W., Mulder, J. & Frencken, J. Is preventing micro-cavities in dentine from progressing with a sealant successful?. Br Dent J 226, 590–594 (2019). https://doi.org/10.1038/s41415-019-0195-9
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0195-9
This article is cited by
-
Advances in knowledge and practice benefiting the health and management of first permanent molars in children
British Dental Journal (2025)
-
Knowledge and opinions of French dental students related to caries risk assessment and dental sealants (preventive and therapeutic)
Odontology (2021)
-
Managing dental caries against the backdrop of COVID-19: approaches to reduce aerosol generation
British Dental Journal (2020)