Abstract
Objectives
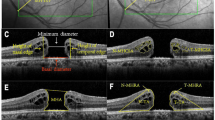
To reassess the definition of a large macular hole, factors predicting hole closure and post-surgery visual recovery.
Design
Database study of 1483 primary macular hole operations. Eligible operations were primary MH operations treated with a vitrectomy and a gas or air tamponade. Excluded were eyes with a history of retinal detachment, high myopia, previous vitrectomy or trauma.
Results
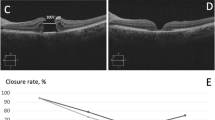
A higher proportion of operations were performed in eyes from females (71.1%) who were ‘on average’ younger (p < 0.001), with slightly larger holes (p < 0.001) than male patients. Sulfur hexafluoride gas was generally used for smaller holes (p < 0.001). From 1253 operations with a known surgical outcome, successful hole closure was achieved in 1199 (96%) and influenced by smaller holes and complete ILM peeling (p < 0.001), but not post-surgery positioning (p = 0.072). A minimum linear diameter of ~500 μm marked the threshold where the success rate started to decline. From the 1056 successfully closed operations eligible for visual outcome analysis, visual success (defined as visual acuity of 0.30 or better logMAR) was achieved in 488 (46.2%) eyes. At the multivariate level, the factors predicting visual success were better pre-operative VA, smaller hole size, shorter duration of symptoms and the absence of AMD.
Conclusions
Females undergoing primary macular hole surgery tend to be younger and have larger holes than male patients. The definition of a large hole should be changed to around 500 μm, and patients should be operated on early to help achieve a good post-operative VA.
Similar content being viewed by others
Login or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Meuer SM, Myers CE, Klein BE, Swift MK, Huang Y, Gangaputra S, et al. The epidemiology of vitreoretinal interface abnormalities as detected by spectral-___domain optical coherence tomography: the beaver dam eye study. Ophthalmology. 2015;122:787–95.
Kelly NE, Wendel RT. Vitreous surgery for idiopathic macular holes. Results of a pilot study. Arch Ophthalmol. 1991;109:654–9.
Madi HA, Masri I, Steel DH. Optimal management of idiopathic macular holes. Clin Ophthalmol. 2016;10:97–116.
Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology. 2010;117:2018–25.
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology. 2013;120:629–34.
BEAVRS datasets system. http://outcomes.beavrs.org/. Accessed 8 Jun 2019.
Royal College of Ophthalmologists macular hole surgery dataset https://www.rcophth.ac.uk/wp-content/uploads/2015/02/2015_PROF_311_Macular-hole-surgery-dataset.pdf. Accessed 8 Jun 2019.
Steel DH, Downey L, Greiner K, Heimann H, Jackson TL, Koshy Z, et al. The design and validation of an optical coherence tomography-based classification system for focal vitreomacular traction. Eye. 2016;30:314–24.
Lange C, Felten N, Junker B, Schulze-Bonsel K, Bach M. Resolving the clinical acuity categories “hand motion” and “counting fingers” using the Freiburg Visual Acuity Test (FrACT). Graefes Arch Clin Exp Ophthalmol. 2009;247:137–42.
Schulze-Bonsel K, Felten N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the Feiburg visual acuity test. Invest Ophthalmol Vis Sci. 2006;47:1236–40.
Vaziri K, Schwartz SG, Kishor KS, Fortun JA, Moshfeghi AA, Smiddy WE, et al. Rates of reoperation and retinal detachment after macular hole surgery. Ophthalmology. 2016;123:26–31.
Essex RW, Hunyor AP, Moreno-Betancur M, Yek JTO, Kingston ZS, Campbell WG. Australian and New Zealand Society of Retinal Specialists Macular Hole Study Group,et al. The visual outcomes of macular hole surgery: a registry-based study by the Australian and New Zealand Society of Retinal Specialists. Ophthalmol Retin. 2018;2:1143–51.
Essex RW, Kingston ZS, Moreno-Betancur M, Shadbolt B, Hunyor AP, Campbell WG. Australian and New Zealand Society of Retinal Specialists Macular Hole Study Group,et al. The effect of postoperative face-down positioning and of long- versus short-acting gas in macular hole surgery: results of a registry-based study. Ophthalmology . 2016;123:1129–36.
Tognetto D, Grandin R, Sanguinetti G, Minutola D, Di Nicola M, Di Mascio R, et al. Internal limiting membrane removal during macular hole surgery: results of a multicenter retrospective study. Ophthalmology. 2006;113:1401–10.
Philippakis E, Amouyal F, Couturier A, Boulanger-Scemama E, Gaudric A, Tadayoni R. Size and vitreomacular attachment of primary full-thickness macular holes. Br J Ophthalmol. 2017;101:951–4.
Spiteri Cornish K, Lois N, Scott N, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane (ILM) peeling versus vitrectomy with no peeling for idiopathic full-thickness macular hole (FTMH). Cochrane Database Syst Rev. 2013:CD009306.
Johnson RN, Gass JD. Idiopathic macular holes. Observations, stages of formation, and implications for surgical intervention. Ophthalmology. 1988;95:917–24.
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013;120:2611–9.
Williamson TH, Lee E. Idiopathic macular hole: analysis of visual outcomes and the use of indocyanine green or brilliant blue for internal limiting membrane peel. Graefes Arch Clin Exp Ophthalmol. 2014;252:395–400.
Ch’ng SW, Patton N, Ahmed M, Ivanova T, Baumann C, Charles S, et al. The manchester large macular hole study: is it time to reclassify large macular holes? Am J Ophthalmol. 2018;195:36–42.
Gupta B, Laidlaw DA, Williamson TH, Shah SP, Wong R, Wren S. Predicting visual success in macular hole surgery. Br J Ophthalmol. 2009;93:1488–91.
Salter AB, Folgar FA, Weissbrot J, Wald KJ. Macular hole surgery prognostic success rates based on macular hole size. Ophthalmic Surg Lasers Imaging. 2012;43:184–9.
Ohana O, Barak A, Schwartz S. Internal aspiration under perfluorocarbon liquid for the management of large macular holes. Retina. 2017;37:2145–50.
Paques M, Chastang C, Mathis A, Sahel J, Massin P, Dosquet C. Platelets in Macular Hole Surgery Group,et al. Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double-masked, randomized trial. Ophthalmology. 1999;106:932–8.
Grewal DS, Mahmoud TH. Autologous neurosensory retinal free flap for closure of refractory myopic macular holes. JAMA Ophthalmol. 2016;134:229–30.
Rizzo S, Caporossi T, Tartaro R, Finocchio L, Franco F, Barca F, et al. A human amniotic membrane plug to promote retinal breaks repair and recurrent macular hole closure. Retina. 2018. https://doi.org/10.1097/IAE.0000000000002320.
Wong R, Howard C, Orobona GD. Retina expansion technique for macular hole apposition report 2: efficacy, closure rate, and risks of a macular detachment technique to close large full-thickness macular holes. Retina. 2018;38:660–3.
Charles S, Randolph JC, Neekhra A, Salisbury CD, Littlejohn N, Calzada JI. Arcuate retinotomy for the repair of large macular holes. Ophthalmic Surg Lasers Imaging Retin. 2013;44:69–72.
Forsaa VA, Lindtjørn B, Kvaløy JT, Frøystein T, Krohn J. Epidemiology and morphology of full-thickness macular holes. Acta Ophthalmol. 2018;96:397–404.
Shin JY, Chu YK, Hong YT, Kwon OW, Byeon SH. Determination of macular hole size in relation to individual variabilities of fovea morphology. Eye. 2015;29:1051–9.
Ghassemi F, Mirshahi R, Bazvand F, Fadakar K, Faghihi H, Sabour S. The quantitative measurements of foveal avascular zone using optical coherence tomography angiography in normal volunteers. J Curr Ophthalmol. 2017;29:293–9.
Chui TY, Van Nasdale DA, Elsner AE, Burns SA. The association between the foveal avascular zone and retinal thickness. Investig Ophthalmol Vis Sci. 2014;55:6870–6787.
Wu LZ, Huang ZS, Wu DZ, Chan E. Characteristics of the capillary-free zone in the normal human macula. Jpn J Ophthalmol. 1985;29:406–11.
Shahlaee A, Pefkianaki M, Hsu J, Ho AC. Measurement of foveal avascular zone dimensions and its reliability in healthy eyes using optical coherence tomography angiography. Am J Ophthalmol. 2016;16:50–5.
Tick S, Rossant F, Ghorbel I, Gaudric A, Sahel JA, Chaumet-Riffaud P, et al. Foveal shape and structure in a normal population. Investig Ophthalmol Vis Sci. 2011;52:5105–10.
Issa SA, Connor A, Habib M, Steel DH. Comparison of retinal breaks observed during 23 gauge transconjunctival vitrectomy versus conventional 20 gauge surgery for proliferative diabetic retinopathy. Clin Ophthalmol. 2011;5:109–14.
Jalil A, Ho WO, Charles S, Dhawahir-Scala F, Patton N. Iatrogenic retinal breaks in 20-G versus 23-G pars plana vitrectomy. Graefes Arch Clin Exp Ophthalmol. 2013;251:1463–7.
Kanovský R, Jurecka T, Gelnarová E. Analysis of prognostic factors of anatomical and functional results of idiopathic macular hole surgery. Cesk Slov Oftalmol. 2009;65:91–6.
Chang E, Garg P, Capone A Jr. Outcomes and predictive factors in bilateral macular holes. Ophthalmology 2013;120:1814–9.
Jaycock PD, Bunce C, Xing W, Thomas D, Poon W, Gazzard G, et al. Outcomes of macular hole surgery: implications for surgical management and clinical governance. Eye. 2005;19:879–84.
Simcock PR, Scalia S. Phacovitrectomy without prone posture for full thickness macular holes. Br J Ophthalmol. 2001;85:1316–9.
Steel DH. Phacovitrectomy: expanding indications. J Cataract Refract Surg. 2007;33:933–6.
Acknowledgements
It is with deep regret that we note the death of our friend and colleague Robert Johnston, who sadly died in September 2016. Without his inspirational vision, determination and career long commitment to quality improvement in ophthalmology this work would not have been possible.
Funding
The database set up and running has been made possible by funding support from the British and Eire Association of Vitreo-retinal Surgeons, and Euretina.
Members of the BEAVRS Macular hole outcome group
Abdallah A. Ellabban7, Andrew H. C. Morris8, Ashraf Khan9, Atiq R. Babar10, Craig Goldsmith11, Deepak Vayalambrone12, Diego Sanchez-Chicharro13, Ed Hughes14, George Turner15, Huw Jenkins16, Imran J. Khan17, Izabela Mitrut18, Jonathan Smith1, Kamaljit S. Balaggan19, Kurt Spiteri Cornish20, Laura Wakeley21, Luke Membrey22, Mark Costen10, E. N. Herbert22, Assad Jalil15, Sandro di Simplicio23, Sonali Tarafdar24, Timothy Cochrane21, Tsveta Ivanova15, Vaughan Tanner25
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
DS has received fees as a consultant for Alcon, Orbit Biomedical and Novartis, and research funding from Alcon and Bayer. TW has received consultancy, author or lecturing fees from or has a financial relationship with Valeant Bausch and Lomb, Kingston upon Thames, UK, Alcon Laboratories, Camberley, UK, Oxular Biotech, Oxford, UK, Galecto Biotech, Copenhagen, Denmark, Axsys Technologies, Glasgow, UK, Springer Publishers, Berlin, Germany, CRC Press, Boca Raton, Florida, USA and Daybreak Medical, London, UK. AL, DY, PD and GA declare no conflicts of interest
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the BEAVRS Macular hole outcome group are listed below Acknowledgements
Supplementary information
Rights and permissions
About this article
Cite this article
Steel, D.H., Donachie, P.H.J., Aylward, G.W. et al. Factors affecting anatomical and visual outcome after macular hole surgery: findings from a large prospective UK cohort. Eye 35, 316–325 (2021). https://doi.org/10.1038/s41433-020-0844-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0844-x
This article is cited by
-
Retinal atrophy and eccentric macular hole after internal limiting membrane peeling: a case report
BMC Ophthalmology (2025)
-
Supervised machine learning statistical models for visual outcome prediction in macular hole surgery: a single-surgeon, standardized surgery study
International Journal of Retina and Vitreous (2025)
-
Macular hole surgery in times of the COVID-19 pandemic
Scientific Reports (2025)
-
Internal limiting membrane peel size and macular hole surgery outcome: a systematic review and individual participant data study of randomized controlled trials
Eye (2025)
-
Comparison of the use of internal limiting membrane flaps versus conventional ILM peeling on post-operative anatomical and visual outcomes in large macular holes
Eye (2024)