Abstract
Purpose
To explore the use of autologous platelet-rich plasma (PRP) as a potential therapeutic adjuvant strategy for treating degenerative lamellar macular holes (LMHs).
Design
A prospective interventional case series.
Methods
Seven consecutive patients (8 eyes) with a diagnosis of LMH underwent a pars-plana vitrectomy with PRP injection under air tamponade. Anatomical results based on spectral ___domain optical coherence tomography (SD-OCT) and functional results, in terms of best corrected visual acuity (BCVA) and reading performance, were analyzed.
Results
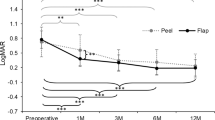
At 12 months postoperatively, 7 out of 8 eyes (88%) presented a complete closure of the LMH. The ellipsoid zone (EZ) was restored in 3 eyes (37.5%). The mean (±SD) postoperative BCVA was 0.39 (±0.56) LogMAR, resulting in a statistically significant visual acuity improvement (p = 0.007). The mean (±SD) maximum reading speed (MaxRS) improved to 133.48 (±41.47) wpm, with a significant increase compared to the baseline (p = 0.029). The mean (±SD) reading acuity score (RA score) resulted in 0.44 (±0.04) LogRAD, with an improvement in reading acuity that did not reach statistical significance (p = 0.129).
Conclusions
The utilization of the PRP technique with a no-retina-touch approach safeguards the delicate retinal tissues, minimizing the possibility of iatrogenic trauma or post-operative complications, while maintaining a high rate of efficacy in enabling the improvement of the foveal defect in lamellar macular holes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
269,00 € per year
only 14,94 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request. Data are located in controlled access data storage at the University of Turin.
References
Gass JDM. Lamellar macular hole: a complication of cystoid macular edema after cataract extraction. Arch Ophthalmol 1976;94:793.
Theodossiadis PG, Grigoropoulos VG, Emfietzoglou I, Nikolaidis P, Vergados I, Apostolopoulos M, et al. Evolution of lamellar macular hole studied by optical coherence tomography. Graefes Arch Clin Exp Ophthalmol 2009;247:13–20.
Bottoni F, Deiro AP, Giani A, Orini C, Cigada M, Staurenghi G. The natural history of lamellar macular holes: a spectral ___domain optical coherence tomography study. Graefes Arch Clin Exp Ophthalmol 2013;251:467–475.
Hubschman JP, Govetto A, Spaide RF, Schumann R, Steel D, Figueroa MS, et al. Optical coherence tomography-based consensus definition for lamellar macular hole. Br J Ophthalmol 2020;104:1741–1747.
Coassin M, Mastrofilippo V, Stewart JM, Fanti A, Belpoliti M, Cimino L, et al. Lamellar macular holes: surgical outcome of 106 patients with long-term follow-up. Graefes Arch Clin Exp Ophthalmol 2018;256:1265–1273.
Chehaibou I, Philippakis E, Mané V, Lavia C, Couturier A, Gaudric A, et al. Surgical outcomes in patients with lamellar macular holes selected based on the optical coherence tomography consensus definition. Int J Retin Vitr 2021;7:31.
Parisi G, Fallico M, Maugeri A, Barchitta M, Agodi A, Russo A, et al. Primary vitrectomy for degenerative and tractional lamellar macular holes: A systematic review and meta-analysis Tsai D-C (ed). PLOS ONE. 2021; 16: e0246667.
Omoto T, Asahina Y, Zhou HP, Fujino R, Takao M, Obata R, et al. Visual outcomes and prognostic factors of vitrectomy for lamellar macular holes and epiretinal membrane foveoschisis Vavvas DG (ed). PLOS ONE. 2021; 16: e0247509.
Figueroa MS, Noval S, Contreras I. Macular structure on optical coherence tomography after lamellar macular hole surgery and its correlation with visual outcome. Can J Ophthalmol 2011;46:491–497.
Jackson TL, Donachie PHJ, Sparrow JM, Johnston RL. United Kingdom National Ophthalmology Database study of vitreoretinal surgery: report 2, macular hole. Ophthalmology 2013;120:629–634.
Lois N, Burr J, Norrie J, Vale L, Cook J, McDonald A, et al. Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial. Invest Ophthalmol Vis Sci 2011;52:1586–1592.
Spiteri Cornish K, Lois N, Scott N, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane (ILM) peeling versus vitrectomy with no peeling for idiopathic full-thickness macular hole (FTMH). Cochrane Database Syst. Rev. 2013; CD009306.
Gonzalez A, Amin S, Iqbal O, Potter SM, Khurshid SG. Use of autologous platelets for lamellar macular hole repair. Case Rep. Ophthalmol Med 2019;2019:1–4.
Hagenau F, Nobl M, Vogt D, Schworm B, Siedlecki J, Kreutzer T, et al. Highly concentrated autologous platelet-rich plasma restores foveal anatomy in lamellar macular hole surgery. Klin Monatsbl Augenheilkd 2021;238:885–892.
Hagenau F, Osterode EV, Klaas JE, Vogt D, Keidel LF, Schworm B, et al. Long-term results of adjunct autologous platelet-rich plasma in lamellar macular hole surgery showing lasting restoration of foveal anatomy. Int J Mol Sci 2023;24:4589.
Huang Y, Gangaputra S, Lee KE, Narkar AR, Klein R, Klein BEK, et al. Signal quality assessment of retinal optical coherence tomography images. Invest Ophthalmol Vis Sci 2012;53:2133–2141.
Calossi A, Boccardo L, Fossetti A, Radner W. Design of short Italian sentences to assess near vision performance. J Optom 2014;7:203–209.
Radner W, Willinger U, Obermayer W, Mudrich C, Velikay-Parel M, Eisenwort B. Eine neue Lesetafel* zur gleichzeitigen Bestimmung von Lesevisus und Lesegeschwindigkeit [A new reading chart for simultaneous determination of reading vision and reading speed]. Klin Monatsblätter Für Augenheilkd 1998;213:174–181.
Catania F, Romano MR, Crincoli E, Allegrini D, Miere A, Chehaibou I, et al. Phenomenology of spontaneous closure in degenerative and mixed type lamellar macular hole. Eye Lond Engl 2024;38:315–320.
Catania F, Allegrini D, Nembri A, Confalonieri F, Zollet P, Crincoli E, et al. Macular microvascular modifications in progressive lamellar macular holes. Diagn Basel Switz 2021;11:1717.
Gaudric A, Massin P, Paques M, Santiago P-Y, Guez J-E, Le Gargasson J-F, et al. Autologous platelet concentrate for the treatment of full-thickness macular holes. Graefes Arch Clin Exp Ophthalmol 1995;233:549–554.
Ruzafa N, Pereiro X, Fonollosa A, Araiz J, Acera A, Vecino E. Plasma Rich in Growth Factors (PRGF) increases the number of retinal müller glia in culture but not the survival of retinal neurons. Front Pharmacol 2021;12:606275.
Wu A-L, Liu Y-T, Chou H-D, Chuang L-H, Chen K-J, Chen Y-P, et al. Role of growth factors and internal limiting membrane constituents in müller cell migration. Exp Eye Res 2021;202:108352.
Dohan Ehrenfest DM, Bielecki T, Mishra A, Borzini P, Inchingolo F, Sammartino G, et al. In search of a consensus terminology in the field of platelet concentrates for surgical use: Platelet-Rich Plasma (PRP), Platelet-Rich Fibrin (PRF), fibrin gel polymerization and leukocytes. Curr Pharm Biotechnol 2012;13:1131–1137.
Hagenau F, Luft N, Nobl M, Vogt D, Klaas JE, Schworm B, et al. Improving morphological outcome in lamellar macular hole surgery by using highly concentrated autologous platelet-rich plasma. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol 2022;260:1517–1524.
Gelormini F, D'antico S, Ricardi F, Parisi G, Borrelli E, Marolo P et al. Platelet concentrates in macular hole surgery. A journey through the labyrinth of terminology, preparation, and application: a comprehensive review. Graefes Arch Clin Exp Ophthalmol. 2024;262:2365–2388.
Xu H, Qin L, Zhang Y, Xiao Y, Zhang M. Surgery outcomes of lamellar macular eyes with or without lamellar hole-associated epiretinal proliferation: a meta-analysis. BMC Ophthalmol 2020;20:345.
Burmeister SL, Hartwig D, Limb GA, Kremling C, Hoerauf H, Müller M, et al. Effect of various platelet preparations on retinal muller cells. Invest Ophthalmol Vis Sci 2009;50:4881–4886.
Bringmann A, Unterlauft JD, Wiedemann R, Rehak M, Wiedemann P. Morphology of partial-thickness macular defects: presumed roles of Müller cells and tissue layer interfaces of low mechanical stability. Int J Retin Vitr 2020;6:28.
Nguyen JH, Yee KMP, Nguyen-Cuu J, Sebag J. Structural and functional characteristics of lamellar macular holes. Retina 2019;39:2084–2089.
Reibaldi M, Parravano M, Varano M, Longo A, Avitabile T, Uva MG, et al. Foveal microstructure and functional parameters in lamellar macular hole. Am J Ophthalmol 2012;154:974–980.e1.
Takahashi K, Morizane Y, Kimura S, Shiode Y, Doi S, Okanouchi T, et al. Results of lamellar macular hole-associated epiretinal proliferation embedding technique for the treatment of degenerative lamellar macular hole. Graefes Arch Clin Exp Ophthalmol 2019;257:2147–2154.
Ho T-C, Ho AY-L, Chen M-S. Reconstructing foveola by foveolar internal limiting membrane non-peeling and tissue repositioning for lamellar hole-related epiretinal Proliferation. Sci Rep. 2019;9:16030.
Purtskhvanidze K, Balken L, Hamann T, Wöster L, Von Der Burchard C, Roider J, et al. Long-term follow-up of lamellar macular holes and pseudoholes over at least 5 years. Graefes Arch Clin Exp Ophthalmol 2018;256:1067–1078.
Garretson BR, Pollack JS, Ruby AJ, Drenser KA, Williams GA, Sarrafizadeh R. Vitrectomy for a symptomatic lamellar macular hole. Ophthalmology 2008;115:884–886.e1.
Sun J-P, Chen S-N, Chuang C-C, Lin C-W, Lin C-J, Huang J-Y, et al. Surgical treatment of lamellar macular hole secondary to epiretinal membrane. Graefes Arch Clin Exp Ophthalmol Albrecht Von Graefes Arch Klin Exp Ophthalmol 2013;251:2681–2688.
Haave H, Petrovski BÉ, Zając M, Lumi X, Melekidou W, Lytvynchuk L, et al. Outcomes from the retrospective multicenter cross-sectional study on lamellar macular hole surgery. Clin Ophthalmol Auckl Nz 2022;16:1847–1860.
Legge GE, Ross JA, Isenberg LM, LaMay JM. Psychophysics of reading. Clinical predictors of low-vision reading speed. Invest Ophthalmol Vis Sci. 1992;33:677–687.
Bailey IL, Lovie-Kitchin JE. Visual acuity testing. From the laboratory to the clinic. Vis Res 2013;90:2–9.
Flom MC, Weymouth FW, Kahneman D. Visual resolution and contour interaction*. J. Opt. Soc. Am. 1963; 53: 1026.
Author information
Authors and Affiliations
Contributions
Michele Reibaldi had the idea for the article. Federico Ricardi, Francesco Gelormini, Guglielmo Parisi, Veronica Vallino, Enrico Borrelli, Paola Marolo, and Michele Reibaldi equally contributed to the literature search, study design, and implementation, as well as participated in the writing of the paper. Sergio D’Antico and Marika Salafia have been contributing to the critical revision of the PRP preparation and the conclusions. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ricardi, F., Gelormini, F., Parisi, G. et al. The no-retina-touch technique: vitrectomy and platelet-rich plasma in the treatment of lamellar macular hole. New insights into pathogenesis. Eye 39, 300–306 (2025). https://doi.org/10.1038/s41433-024-03414-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03414-5