Abstract
Purpose
Inconsistency exists among reported studies on the composition of human ocular surface microbiome (OSM). The roles of OSM in ocular diseases remain uncertain. In this study, we aimed to determine the composition of OSM and to evaluate its potential roles and functions from multiple cohorts.
Methods
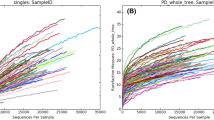
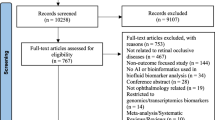
Raw 16 s sequencing data were obtainable from publicly available repositories, sourced from 17 published studies. Employing a standardized method, we processed the data and conducted a cross-cohort analysis. Through bioinformatics pipelines QIIME2 and PICRUSt2, we processed a total of 1875 ocular surface samples. Core microbiome analyses, genera comparisons, and MetaCyc pathway analyses were performed within each cohort independently. The results were then combined to identify shared patterns across different datasets.
Results
The core OSM comprised seven genera: Corynebacterium, Staphylococcus, Acinetobacter, Streptococcus, Pseudomonas, Cutibacterium and Bacillus. Corynebacterium and Staphylococcus are the most abundant genera on ocular surface. Most ocular diseases showed OSM alterations and eight genera demonstrated a non-specific, shared response among two or more ocular diseases. Moreover, changes in various metabolic pathways were predicted following OSM alteration, indicating potential roles of OSM in biological processes.
Conclusion
We refined the core OSM candidates combining multiple cohorts. The common pattern shared by different cohorts is worth further investigation. Changes in metabolic pathways based on bioinformatic analysis indicated a role of OSM on ocular diseases. Our results help extend the knowledge and encourage further investigations on the associations between OSM and ocular diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 18 print issues and online access
269,00 € per year
only 14,94 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Raw sequencing data for each study is accessible as described in Supplementary Table 1. Our re-analysed OTU/ASV tables are available at: https://github.com/ficion1/meta-analysis-of-OSM. Our study can be reproduced using these files. Supplementary files include tables showing the prevalence rates of core microbiomes and the q-values of univariate comparisons for each dataset. All other relevant data supporting the study findings are available in this article and its supplementary files, as well as from the corresponding author upon request.
References
Petrillo F, Pignataro D, Lavano MA, Santella B, Folliero V, Zannella C, et al. Current Evidence on the Ocular Surface Microbiota and Related Diseases. Microorganisms. 2020;8:1033.
Aragona P, Baudouin C, Benitez Del Castillo JM, Messmer E, Barabino S, Merayo-Lloves J, et al. The ocular microbiome and microbiota and their effects on ocular surface pathophysiology and disorders. Surv Ophthalmol. 2021;66:907–25.
Cavuoto KM, Banerjee S, Galor A. Relationship between the microbiome and ocular health. Ocul Surf. 2019;17:384–92.
St Leger AJ, Desai JV, Drummond RA, Kugadas A, Almaghrabi F, Silver P, et al. An Ocular Commensal Protects against Corneal Infection by Driving an Interleukin-17 Response from Mucosal gammadelta T Cells. Immunity. 2017;47:148–58e145.
Iwase T, Uehara Y, Shinji H, Tajima A, Seo H, Takada K, et al. Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature. 2010;465:346–9.
Kugadas A, Christiansen SH, Sankaranarayanan S, Surana NK, Gauguet S, Kunz R, et al. Impact of Microbiota on Resistance to Ocular Pseudomonas aeruginosa-Induced Keratitis. PLoS Pathog. 2016;12:e1005855.
Momose Y, Hirayama K, Itoh K. Competition for proline between indigenous Escherichia coli and E. coli O157:H7 in gnotobiotic mice associated with infant intestinal microbiota and its contribution to the colonization resistance against E. coli O157:H7. Antonie Van Leeuwenhoek. 2008;94:165–71.
Molloy MJ, Bouladoux N, Belkaid Y. Intestinal microbiota: shaping local and systemic immune responses. Semin Immunol. 2012;24:58–66.
Graham JE, Moore JE, Jiru X, Moore JE, Goodall EA, Dooley JS, et al. Ocular pathogen or commensal: a PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci. 2007;48:5616–23.
Liborio AM, Nishiwaki-Dantas MC, Mimica LM, Dantas PE, Lima AL. [Conjunctival microbiota in patients with ocular allergy]. Arq Bras Oftalmol. 2005;68:824–7.
Tuzhikov A, Dong Q, Panchin A, Thanathanee O, Shalabi N, Nelson D, et al. Keratitis-induced changes to the homeostatic microbiome at the human cornea. Investigative Ophthalmol Vis Sci. 2013;54:2891–91.
Zhou Y, Holland MJ, Makalo P, Joof H, Roberts CH, Mabey DC, et al. The conjunctival microbiome in health and trachomatous disease: a case control study. Genome Med. 2014;6:99.
Martins EN, Alvarenga LS, Hofling-Lima AL, Freitas D, Zorat-Yu MC, Farah ME, et al. Aerobic bacterial conjunctival flora in diabetic patients. Cornea. 2004;23:136–42.
Ozkan J, Nielsen S, Diez-Vives C, Coroneo M, Thomas T, Willcox M. Temporal Stability and Composition of the Ocular Surface Microbiome. Sci Rep. 2017;7:9880.
Huang Y, Yang B, Li W. Defining the normal core microbiome of conjunctival microbial communities. Clin Microbiol Infect. 2016;22:643.e7–643.e12.
Zhang Z, Zou X, Xue W, Zhang P, Wang S, Zou H. Ocular Surface Microbiota in Diabetic Patients With Dry Eye Disease. Invest Ophthalmol Vis Sci. 2021;62:13.
Ozkan J, Willcox MD. The Ocular Microbiome: Molecular Characterisation of a Unique and Low Microbial Environment. Curr Eye Res. 2019;44:685–94.
Johnson JS, Spakowicz DJ, Hong BY, Petersen LM, Demkowicz P, Chen L, et al. Evaluation of 16S rRNA gene sequencing for species and strain-level microbiome analysis. Nat Commun. 2019;10:5029.
Wen X, Miao L, Deng Y, Bible PW, Hu X, Zou Y, et al. The Influence of Age and Sex on Ocular Surface Microbiota in Healthy Adults. Invest Ophthalmol Vis Sci. 2017;58:6030–7.
Zhang Y, Liu ZR, Chen H, Dong WJ, Fan YC, Yu H, et al. Comparative study of bacterial status from conjunctival sac of the elder Qiang minority and Han people with dry eye in Sichuan, China. Int J Ophthalmol. 2012;5:343–7.
Delbeke H, Younas S, Casteels I, Joossens M. Current knowledge on the human eye microbiome: a systematic review of available amplicon and metagenomic sequencing data. Acta Ophthalmol. 2021;99:16–25.
Kugadas A, Gadjeva M. Impact of Microbiome on Ocular Health. Ocul Surf. 2016;14:342–9.
Baim AD, Movahedan A, Farooq AV, Skondra D. The microbiome and ophthalmic disease. Exp Biol Med (Maywood). 2019;244:419–29.
Willcox MD. Characterization of the normal microbiota of the ocular surface. Exp Eye Res. 2013;117:99–105.
Chong J, Liu P, Zhou G, Xia J. Using MicrobiomeAnalyst for comprehensive statistical, functional, and meta-analysis of microbiome data. Nat Protoc. 2020;15:799–821.
Pickering H, Ramadhani AM, Massae P, Mafuru E, Malisa A, Mbuya K, et al. The conjunctival microbiome before and after azithromycin mass drug administration for trachoma control in a cohort of Tanzanian children. Front Public Health. 2022;10:1015714.
Ozkan J, Majzoub ME, Coroneo M, Thomas T, Willcox M. Ocular microbiome changes in dry eye disease and meibomian gland dysfunction. Exp Eye Res. 2023;235:109615.
An N, Wang C, Dou X, Liu X, Wu J, Cheng Y. Comparison of 16S rDNA Amplicon Sequencing With the Culture Method for Diagnosing Causative Pathogens in Bacterial Corneal Infections. Transl Vis Sci Technol. 2022;11:29.
Ren Z, Liu Q, Li W, Wu X, Dong Y, Huang Y. Profiling of Diagnostic Information of and Latent Susceptibility to Bacterial Keratitis From the Perspective of Ocular Bacterial Microbiota. Front Cell Infect Microbiol. 2021;11:645907.
Ren Z, Li W, Liu Q, Dong Y, Huang Y. Profiling of the Conjunctival Bacterial Microbiota Reveals the Feasibility of Utilizing a Microbiome-Based Machine Learning Model to Differentially Diagnose Microbial Keratitis and the Core Components of the Conjunctival Bacterial Interaction Network. Front Cell Infect Microbiol. 2022;12:860370.
Ueta M, Hosomi K, Park J, Mizuguchi K, Sotozono C, Kinoshita S, et al. Categorization of the Ocular Microbiome in Japanese Stevens-Johnson Syndrome Patients With Severe Ocular Complications. Front Cell Infect Microbiol. 2021;11:741654.
Dong X, Wang Y, Wang W, Lin P, Huang Y. Composition and Diversity of Bacterial Community on the Ocular Surface of Patients With Meibomian Gland Dysfunction. Invest Ophthalmol Vis Sci. 2019;60:4774–83.
Willis KA, Postnikoff CK, Freeman A, Rezonzew G, Nichols K, Gaggar A, et al. The closed eye harbours a unique microbiome in dry eye disease. Sci Rep. 2020;10:12035.
Song H, Xiao K, Chen Z, Long Q. Analysis of Conjunctival Sac Microbiome in Dry Eye Patients With and Without Sjogren’s Syndrome. Front Med (Lausanne). 2022;9:841112.
Ali SM, Abdel-Gawad MM, Azab M, Hamed S, Emara M, Shawky RM. Comparative analysis of the ocular surface microbiome in type-1, type-2 diabetes mellitus and healthy individuals. J Appl Microbiol. 2023;134.
Ji X, Dong K, Pu J, Yang J, Zhang Z, Ning X, et al. Comparison of the ocular surface microbiota between thyroid-associated ophthalmopathy patients and healthy subjects. Front Cell Infect Microbiol. 2022;12:914749.
Wilkins LJ, Monga M, Miller AW. Defining Dysbiosis for a Cluster of Chronic Diseases. Sci Rep. 2019;9:12918.
Duvallet C, Gibbons SM, Gurry T, Irizarry RA, Alm EJ. Meta-analysis of gut microbiome studies identifies disease-specific and shared responses. Nat Commun. 2017;8:1784.
Yu S, Balasubramanian I, Laubitz D, Tong K, Bandyopadhyay S, Lin X, et al. Paneth Cell-Derived Lysozyme Defines the Composition of Mucolytic Microbiota and the Inflammatory Tone of the Intestine. Immunity. 2020;53:398–416.e398.
Yoon CH, Ryu JS, Moon J, Kim MK. Association between aging-dependent gut microbiome dysbiosis and dry eye severity in C57BL/6 male mouse model: a pilot study. BMC Microbiol. 2021;21:106.
Zhou Y, Sidhu GS, Whitlock JA, Abdelmalik B, Mayer Z, Li Y, et al. Effects of Carboxymethylcellulose Artificial Tears on Ocular Surface Microbiome Diversity and Composition, A Randomized Controlled Trial. Transl Vis Sci Technol. 2023;12:5.
Bloom AH, Perry HD, Donnenfeld ED, Davis RG. Chryseobacterium meningosepticum keratitis. Am J Ophthalmol. 2003;136:356–7.
Kalogeropoulos D, Holla A, Gupta B, Sutton J, Sepetis A, Rezq H, et al. An Unusual Encounter: Endophthalmitis Associated with Flavobacterium lindanitolerans. Klin Monbl Augenheilkd 2023.
Mirzayi C, Renson A, Genomic Standards C, Massive A, Quality Control S, Zohra F, et al. Reporting guidelines for human microbiome research: the STORMS checklist. Nat Med. 2021;27:1885–92.
Spragge F, Bakkeren E, Jahn MT, Araujo EBN, Pearson CF, Wang X, et al. Microbiome diversity protects against pathogens by nutrient blocking. Science. 2023;382:eadj3502.
Janda JM, Abbott SL. 16S rRNA gene sequencing for bacterial identification in the diagnostic laboratory: pluses, perils, and pitfalls. J Clin Microbiol. 2007;45:2761–4.
Abellan-Schneyder I, Matchado MS, Reitmeier S, Sommer A, Sewald Z, Baumbach J, et al. Primer, Pipelines, Parameters: Issues in 16S rRNA Gene Sequencing. mSphere 2021;6.
Wang C, Dou X, Li J, Wu J, Cheng Y, An N. Composition and Diversity of the Ocular Surface Microbiota in Patients With Blepharitis in Northwestern China. Front Med (Lausanne). 2021;8:768849.
Ozkan J, Willcox M, Wemheuer B, Wilcsek G, Coroneo M, Thomas T. Biogeography of the human ocular microbiota. Ocul Surf. 2019;17:111–8.
Shin H, Price K, Albert L, Dodick J, Park L, Dominguez-Bello MG. Changes in the Eye Microbiota Associated with Contact Lens Wearing. mBio. 2016;7:e00198.
Yan Y, Yao Q, Lu Y, Shao C, Sun H, Li Y, et al. Association Between Demodex Infestation and Ocular Surface Microbiota in Patients With Demodex Blepharitis. Front Med (Lausanne). 2020;7:592759.
Yau JW, Hou J, Tsui SKW, Leung TF, Cheng NS, Yam JC, et al. Characterization of ocular and nasopharyngeal microbiome in allergic rhinoconjunctivitis. Pediatr Allergy Immunol. 2019;30:624–31.
Zhang H, Zhao F, Hutchinson DS, Sun W, Ajami NJ, Lai S, et al. Conjunctival Microbiome Changes Associated With Soft Contact Lens and Orthokeratology Lens Wearing. Invest Ophthalmol Vis Sci. 2017;58:128–36.
Zhong Y, Fang X, Wang X, Lin YA, Wu H, Li C. Effects of Sodium Hyaluronate Eye Drops With or Without Preservatives on Ocular Surface Bacterial Microbiota. Front Med (Lausanne). 2022;9:793565.
Zhu X, Wei L, Rong X, Zhang Y, Zhang Q, Wen X, et al. Conjunctival Microbiota in Patients With Type 2 Diabetes Mellitus and Influences of Perioperative Use of Topical Levofloxacin in Ocular Surgery. Front Med (Lausanne). 2021;8:605639.
Acknowledgements
We thank all the authors who made their data available as well as those who provided data through personal communications.
Funding
The authors have no proprietary or commercial interest in any materials disclosed in this article. This study was supported in part by National Natural Science Foundation of China (82171089 [JCY]); the General Research Fund (GRF), Research Grants Council, Hong Kong (14111515 and 14103419 [JCY]); Collaborative Research Fund (C7149-20G [JCY]); Health and Medical Research Fund (HMRF), Hong Kong (5160836 [LJC], 07180826 [XJZ] and 21220251 [PCP]),), and the Direct Grants of the Chinese University of Hong Kong, (4054193 [LJC] and 4054121 & 4054199 [JCY] and 178662514 and 4054634 [XJZ] and 2015.1.056); the Innovation and Technology Fund (7010590 [JCY]), the UBS Optimus Foundation Grant 8984 (JCY); the Centaline Myopia Fund [JCY]; the CUHK Jockey Club Children’s Eye Care Programme, and the CUHK Jockey Club Myopia Prevention Programme.
Author information
Authors and Affiliations
Contributions
XL, XZ, HNC, and JCY conceived of the research. XL and XZ identified and downloaded the datasets. XL and JWY processed the data. CHTB and XL interpreted the results and prepared the manuscript. LJC and JCY supervised the work. All authors discussed and revised the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests. Alvin Young is a member of the Eye editorial board.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ling, X., Zhang, X.J., Bui, C.H.T. et al. Multi-cohort analysis identifying core ocular surface microbiome and bacterial alterations in eye diseases. Eye 39, 1276–1285 (2025). https://doi.org/10.1038/s41433-024-03589-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03589-x