Abstract
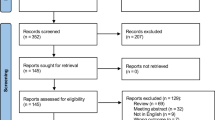
Vacuum erection device (VED) as one of the approved therapies for erectile dysfunction (ED) is widely used. However, available evidence of VED efficacy on refractory ED, a condition often unresponsive to phosphodiesterase type 5 (PDE5) inhibitors, is limited. A literature search was performed using PubMed, EMBASE, and the Cochrane Library to identify all clinical trials up to December 2024. The primary outcome was efficacy defined as successful intercourse or intercourse satisfaction after VED intervention, and the secondary outcome was the incidence of most common side effects. The pooled rate with 95% confidence intervals (CI) was selected as the effect size. Heterogeneity was assessed by Cochran’s Q test and the I2 test. Sensitivity analyses, subgroup analyses and meta-regression were used to explore the sources of heterogeneity. Publication bias was assessed by funnel plots and Egger’s test. Data from 1065 patients across 18 studies were analyzed in this meta-analysis. The pooled effect size of VED efficacy was 0.80 (95% CI: 0.76–0.84). Among the different subgroups, the efficacy of VED in ED patients with mixed etiologies, diabetes mellitus, spinal cord injury and radical prostatectomy were 82.9, 73.0, 71.8 and 84.5%, respectively. The most common side effect was penile bruising with a pooled incidence of 24.3%. ED patients with spinal cord injury may have a higher risk of penile bruising (31.4%). Meta-regression suggested that the publication date and patients’ age may affect the outcome. No significant publication bias was detected. In conclusion, VED is an effective adjunct for improving the intercourse success rate and patient satisfaction in refractory ED. Future large randomized controlled trials with standardized objective measurements and longer follow-up durations are warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
269,00 € per year
only 22,42 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: results of the Massachusetts Male Aging Study. J Urol. 1994;151:54–61.
Montorsi F, McDermott TE, Morgan R, Olsson A, Schultz A, Kirkeby HJ, et al. Efficacy and safety of fixed-dose oral sildenafil in the treatment of erectile dysfunction of various etiologies. Urology. 1999;53:1011–8.
McMahon CG. Current diagnosis and management of erectile dysfunction. Med J Aust. 2019;210:469–76.
Barbonetti A, D’Andrea S, Francavilla S. Testosterone replacement therapy. Andrology. 2020;8:1551–66.
Bearelly P, Phillips EA, Pan S, O’Brien K, Asher K, Martinez D, et al. Long-term intracavernosal injection therapy: treatment efficacy and patient satisfaction. Int J Impot Res. 2020;32:345–51.
Goldstein I, Lue TF, Padma-Nathan H, Rosen RC, Steers WD, Wicker PA. Oral sildenafil in the treatment of erectile dysfunction. Sildenafil Study Group. N Engl J Med. 1998;338:1397–404.
Abdelrahman IFS, Raheem AA, Elkhiat Y, Aburahma AA, Abdel-Raheem T, Ghanem H. Safety and efficacy of botulinum neurotoxin in the treatment of erectile dysfunction refractory to phosphodiesterase inhibitors: results of a Randomized Controlled Trial. Andrology. 2022;10:254–61.
Vinay J, Moreno D, Rajmil O, Ruiz-Castañe E, Sanchez-Curbelo J. Penile low intensity shock wave treatment for PDE5I refractory erectile dysfunction: a Randomized Double-Blind Sham-Controlled Clinical Trial. World J Urol. 2021;39:2217–22.
Wang R, Martins FE, Ralph D, Hatzichristodoulou G, Osmonov D, Parker J, et al. Vacuum erectile devices for erectile dysfunction: recommendations from the 5th international consultation on sexual medicine. Sex Med Rev. 2025;13:172–83.
Korenman SG, Viosca SP, Kaiser FE, Mooradian AD, Morley JE. Use of a vacuum tumescence device in the management of impotence. J Am Geriatr Soc. 1990;38:217–20.
Pirola GM, Naselli A, Maggi M, Gubbiotti M, Rubilotta E, Jeremy Yuen-Chun T, et al. Vacuum erection device for erectile function rehabilitation after radical prostatectomy: which is the correct schedule? Results from a systematic, scoping review. Int J Impot Res. 2024;36:194–200.
Tan HL. Economic cost of male erectile dysfunction using a decision analytic model: for a hypothetical managed-care plan of 100,000 members. Pharmacoeconomics. 2000;17:77–107.
Sultana A, Grice P, Vukina J, Pearce I, Modgil V. Indications and characteristics of penile traction and vacuum erection devices. Nat Rev Urol. 2022;19:84–100.
Wylie KR, Jones RH, Walters S. The potential benefit of vacuum devices augmenting psychosexual therapy for erectile dysfunction: a Randomized Controlled Trial. J Sex Marital Ther. 2003;29:227–36.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Rosen RC, Cappelleri JC, Smith MD, Lipsky J, Peña BM. Development and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunction. Int J Impot Res. 1999;11:319–26.
Shoji M, Hamatani T, Ishikawa S, Kuji N, Ohta H, Matsui H, et al. Sexual satisfaction of infertile couples assessed using the Golombok-Rust Inventory of Sexual Satisfaction (GRISS). Sci Rep. 2014;4:5203.
Goldstein I, Tseng LJ, Creanga D, Stecher V, Kaminetsky JC. Efficacy and safety of sildenafil by age in men with erectile dysfunction. J Sex Med. 2014;13:852–9.
Cappelleri JC, Tseng LJ, Stecher V, Goldstein I. Enriching the interpretation of the erectile dysfunction inventory of treatment satisfaction: characterizing success in treatment satisfaction. J Sex Med. 2018;15:732–40.
Yamagishi M, Ogushi Y, Niikura A, Ohta T, Ichimura Y, Hashimoto Y, et al. Erectile dysfunction in young patients and elderly patients by sexual encounter profile: A comparative study. Int J Urol. 2022;29:566–70.
Porst H, Gilbert C, Collins S, Huang X, Symonds T, Stecher V, et al. Development and validation of the quality of erection questionnaire. J Sex Med. 2007;4:372–81.
Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in Randomised Trials. BMJ. 2011;343:d5928.
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Price DE, Cooksey G, Jehu D, Bentley S, Hearnshaw JR, Osborn DE. The management of impotence in diabetic men by vacuum tumescence therapy. Diabet Med. 1991;8:964–7.
Sidi AA, Lewis JH. Clinical trial of a simplified vacuum erection device for impotence treatment. Urology. 1992;39:526–8.
Cookson MS, Nadig PW. Long-term results with vacuum constriction device. J Urol. 1993;149:290–4.
Vrijhof HJ, Delaere KP. Vacuum constriction devices in erectile dysfunction: acceptance and effectiveness in patients with impotence of organic or mixed aetiology. Br J Urol. 1994;74:102–5.
Segenreich E, Israilov SR, Shmueli J, Servadio C. Vacuum therapy combined with psychotherapy for management of severe erectile dysfunction. Eur Urol. 1995;28:47–50.
el-Bahrawy M, el-Baz MA, Emam A, el-Magd MA. Noninvasive vacuum constriction device in the management of erectile dysfunction. Int Urol Nephrol. 1995;27:331–3.
Denil J, Ohl DA, Smythe C. Vacuum erection device in spinal cord injured men: patient and partner satisfaction. Arch Phys Med Rehabil. 1996;77:750–3.
Seckin B, Atmaca I, Ozgok Y, Gokalp A, Harmankaya C. External vacuum device therapy for spinal cord injured males with erectile dysfunction. Int Urol Nephrol. 1996;28:235–40.
Chen J, Sofer M, Kaver I, Matzkin H, Greenstein A. Concomitant use of sildenafil and a vacuum entrapment device for the treatment of erectile dysfunction. J Urol. 2004;171:292–5.
Raina R, Agarwal A, Ausmundson S, Lakin M, Nandipati KC, Montague DK, et al. Early use of vacuum constriction device following radical prostatectomy facilitates early sexual activity and potentially earlier return of erectile function. Int J Impot Res. 2006;18:77–81.
Moemen MN, Fahmy I, AbdelAal M, Kamel I, Mansour M, Arafa MM. Erectile dysfunction in spinal cord-injured men: different treatment options. Int J Impot Res. 2008;20:181–7.
Hassan A, El-Hadidy M, El-Deeck BS, Mostafa T. Couple satisfaction to different therapeutic modalities for organic erectile dysfunction. J Sex Med. 2008;5:2381–91.
Engel JD. Effect on sexual function of a vacuum erection device post-prostatectomy. Can J Urol. 2011;18:5721–5.
Sun L, Peng FL, Yu ZL, Liu CL, Chen J. Combined sildenafil with vacuum erection device therapy in the management of diabetic men with erectile dysfunction after failure of first-line sildenafil monotherapy. Int J Urol. 2014;21:1263–7.
Zhang DL, Chen Z, Wang FX, Zhang J, Xie H, Wang ZY, et al. Adding a vacuum erection device to regular use of Tadalafil improves penile rehabilitation after posterior urethroplasty. Asian J Androl. 2019;21:582–6.
Zhang M, Che JZ, Liu YD, Wang HX, Huang YP, Lv XG, et al. A prospective randomized controlled study on scheduled PDE5i and vacuum erectile devices in the treatment of erectile dysfunction after nerve sparing prostatectomy. Asian J Androl. 2022;24:473–7.
Cayetano-Alcaraz AA, Tharakan T, Chen R, Sofikitis N, Minhas S. The management of erectile dysfunction in men with diabetes mellitus unresponsive to phosphodiesterase type 5 inhibitors. Andrology. 2023;11:257–69.
Katz PG, Haden HT, Mulligan T, Zasler ND. The effect of vacuum devices on penile hemodynamics. J Urol. 1990;143:55–6.
Miranda EP, Taniguchi H, Cao DL, Hald GM, Jannini EA, Mulhall JP. Application of sex aids in men with sexual dysfunction: a review. J Sex Med. 2019;16:767–80.
Bock M, Burns RT, Pereira TA, Bernie HL. A contemporary review of the treatments and challenges associated with penile rehabilitation after radical prostatectomy including a proposed optimal approach. Int J Impot Res. 2024;36:480–5.
Köhler TS, Pedro R, Hendlin K, Utz W, Ugarte R, Reddy P, et al. A pilot study on the early use of the vacuum erection device after radical retropubic prostatectomy. BJU Int. 2007;100:858–62.
Yin GN, Kim DK, Kang JI, Im Y, Lee DS, Han AR, et al. Latrophilin-2 is a novel receptor of LRG1 that rescues vascular and neurological abnormalities and restores diabetic erectile function. Exp Mol Med. 2022;54:626–38.
Musicki B, Hannan JL, Lagoda G, Bivalacqua TJ, Burnett AL. Mechanistic link between erectile dysfunction and systemic endothelial dysfunction in type 2 diabetic rats. Andrology. 2016;4:977–83.
Soni SD, Song W, West JL, Khera M. Nitric oxide-releasing polymeric microspheres improve diabetes-related erectile dysfunction. J Sex Med. 2013;10:1915–25.
Mulhall JP, Klein EA, Slawin K, Henning AK, Scardino PT. A randomized, double-blind, placebo-controlled trial to assess the utility of tacrolimus (FK506) for the prevention of erectile dysfunction following bilateral nerve-sparing radical prostatectomy. J Sex Med. 2018;15:1293–9.
Di Bello F, Creta M, Napolitano L, Califano G, Passaro F, Morra S, et al. Male sexual dysfunction and infertility in spinal cord injury patients: state-of-the-art and future perspectives. J Pers Med. 2022;12:873.
Zhang F, Xiong Y, Qin F, Yuan J. Short sleep duration and erectile dysfunction: a review of the literature. Nat Sci Sleep. 2022;14:1945–61.
Trost LW, Munarriz R, Wang R, Morey A, Levine L. External mechanical devices and vascular surgery for erectile dysfunction. J Sex Med. 2016;13:1579–617.
Acknowledgements
Authors appreciate all investigators and researchers of included studies, and thank the assistance of Ruicheng Wu of West China Hospital.
Funding
This work was supported by the Natural Science Foundation of China (No. 824B2017).
Author information
Authors and Affiliations
Contributions
(I)Conception and design: FZ; YJ; (II)Administrative support: GZ; YJ; (III)Provision of study materials or patients: FZ; ZL; QX; XG; (IV)Collection and assembly of data: FZ; ZL; QX; YX; XG; (V)Data analysis and interpretation: FZ; ZL; QX; WZ; YX; (VI) Manuscript writing: FZ; UAO; YJ; (VII)Final approval of manuscript: FZ; ZL; QX; XG; WZ; YX; UAO; GZ; YJ. All named authors meet the ICMJE criteria for authorship in this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, F., Luo, Z., Xue, Q. et al. Efficacy of vacuum erectile device in refractory erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res (2025). https://doi.org/10.1038/s41443-025-01102-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-025-01102-w