Abstract
Floods are becoming more frequent and severe in the context of climate change, with major impacts on human health. However, their effect on infant mortality remains unknown, particularly in low- and middle-income countries. We conducted a sibling-matched case-control study using individual-level data from Demographic and Health Surveys in Africa during 1990–2020. Individual flood experience was determined by matching the residential coordinates with flood events from the Dartmouth Flood Observatory database. Using data from 514,760 newborns, we found increased risks of infant mortality associated with flood exposure across multiple periods, with the risks remaining elevated for up to four years after the flood event. Overall, flood exposure was associated with 3.42 infant deaths per 1000 births in Africa from 2000 to 2020, approximately 1.7 times the burden associated with life-period exposure. This multi-country study in Africa provides novel evidence that flood events may increase infant mortality risk and burden, even over years after exposure.
Similar content being viewed by others
Introduction
Flood has been identified as one of the most frequent and destructive natural hazards, with massive health and economic losses. According to the Centre for Research on the Epidemiology of Disasters (CRED), flood events accounted for 43.4% of total natural disasters globally with 2.0 billion people affected, causing 0.14 million deaths, and 656 billion U.S. dollar in economic losses during 1998–20171. Due to global climate change, flood events are expected to become more frequent and severe in the upcoming decades2,3,4. If no actions are taken, the absolute damage to the global economy due to flood events may increase up to 20-fold by the end of the century5. Floods could cause severe health consequences, including injuries, waterborne diseases, vector-borne diseases, and mortality6.
Children suffered higher risks of mortality during natural disasters, especially flood events7. Most flood-related deaths are caused by drowning, which accounts for 75% of all direct deaths for children affected8. Additionally, flash floods could contaminate water source by chemicals, bacteria, and parasites, thereby increasing the risk of infectious diseases, particularly among children9,10. However, the previous estimations of flood-related child mortality are limited and focused on single flood events or were conducted in small regions11,12. In addition to these short-term consequences, flood events may further damage local food production, economic development, and infrastructure, which may impair the nutritional status of local children and further result in higher morbidity or mortality risks13,14. The potential mid- and long-term impact of flood events on child mortality, however, remain unclear.
Despite having the lowest contribution to global greenhouse gas emissions, low- and middle-income countries (LMICs) in Africa are experiencing more frequent and severe extreme climatic events due to climate change. The Emergency Events Database (EM-DAT) indicates reported a 180% increase in occurrences of floods in Africa during 2002–2021, compared to the previous two decades (1982–2001)14. This is particularly concerning since African countries have limited economic development and poor infrastructure, leaving them more susceptible to the adverse effects of floods15,16. In the period of 2009 to 2020, 12% of the African population that experienced floods was threatened by the food crisis, constituting long-run influences on well-being17. Additionally, despite notable progress towards the Sustainable Development Goals, African countries still face the highest child mortality in the world. However, no studies have examined the association between flood events and child mortality in Africa from a multi-country perspective.
Using a large-scale database of births and deaths for infants (under one year age) in Africa from 1990 to 2020, we conducted this case-control study to test the hypothesis that flood exposures may be associated with infant mortality. By matching flood events across various exposure windows (from months to years) and with varied intensity for the same mothers, we further examined the hypothesis that the excess infant deaths could vary significantly by exposure windows and intensities.
Results
Descriptive data
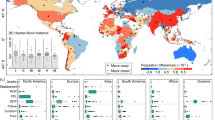
This analysis includes 813 flood events in Africa between 1990 and 2020 (Fig. 1A). Flood hotspots were mainly distributed along with the surface water (e.g., Upper Nile River, Lake Victoria, Lake Chad) in inland areas of the continent, while the East Coast of the continent (e.g., Somalia, Mozambique) and Madagascar also experienced frequent flood events. Over the years, both the frequency and severity of flood events in Africa have increased, particularly in the past five years (Fig. S2).
The geographical distribution of studied clusters was presented in Fig. 1B. The overall infant mortality rate in Africa between 1990 and 2020 was 9.06%, and the rate were decreasing over the study period (Fig. S3). The analysis identified a total of 514,760 newborns from 37 African countries, with 115,053 infant deaths and 399,707 matched surviving infants (Table S3). On average, 3.5 controls were matched per case. Of these cases, almost half were from Western Africa (47.8%), and the majority of cases occurred in rural areas (75.8%). More detailed characteristics of the deceased infants and their matched living infants were shown in Table S4.
Regression results
There were significant and positive associations between flood exposure and infant mortality. Each flood event during the infant’s life time was associated with an increase of 5.35 (95% confidence intervals [CI]: 2.54, 8.34) deaths per 1000 live births (odds ratio [OR] = 1.059, 95% CI: 1.028, 1.092; Fig. 2; Table S5). For short- and mid-term flood exposures, the association of flood events with infant mortality was present in the following month (i.e., lag 1 m), attenuated and became insignificant in the following 8 months (i.e., lag 2–9 m) (Fig. 2A); however, the association turned to statistically significant at lags of 10, 11 and 12 m. For the long-term flood exposure, the association was present in the concurrent year (lag 0 y), increased in the following year (lag 1 y), attenuated in lag 3 y and became insignificant in lag 5 y (Fig. 2B). For the average of lag 0–4 years, a flood event was associated with an increase of 9.69 infant deaths (95% CI: 7.70, 11.69) per 1000 births (OR = 1.107, 95% CI: 1.085, 1.130; Table S5).
Changes and 95% confidence intervals in infant mortality (per 1000 births) associated with flood exposures at different months (A) or years (B), and classified by the severity of flood (C) and regions (D). Estimates in (C, D) were based on exposures at lag 0–4 year, which is the average of flood exposures at the concurrent year and preceding 4 years. Black solid circles indicate the point estimates of the effect, and the black vertical lines represent the 95% confidence intervals.
For floods of different severity levels (Fig. 2C), extreme or very large flood events were associated with a more prominent increase in infant mortality [14.77 infant deaths (95% CI: 11.51, 18.12) per 1000 births], compared to large flood events [6.98 infant deaths (95% CI: 4.62, 9.24) per 1000 births]. As illustrated in Fig. 2D, infants in West Africa and Central Africa experienced higher mortality risk related to flood exposure (16.04 and 12.23 infant deaths per 1000 births, respectively) than in East Africa (10.78 infant deaths per 1000 births), whereas there is no significant risk in North Africa and South Africa.
In stratified analyses, the associations between 5-year flood exposure (lag 0–4 y) and infant mortality were more pronounced for female infants or for mothers with lower education levels (Fig. 3). Infants living in rural areas, and in houses with basic water or sanitation infrastructures, or natural roofs may suffer higher flood-related mortality risk.
In sensitivity analyses, the estimated effects of 5-year flood exposure on infant mortality were robust across models after controlling for the selected covariates one by one (including mother’s age at the time of child, death the year of child death, month of child death, annual mean temperature, annual cumulative precipitation and country-level factors), excluding different covariates from the Main model, using generalized linear mixed models (GLMMs) with country or mother ID a random-effect term or leaving each country out of the analysis individually (Figs. S4 and S5).
Infant mortality burden associated with flood exposure
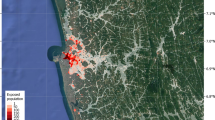
According to the associations between flood events and infant mortality, we estimated that flood exposure from the current year to the following 4 years was associated with 3.42 infant deaths (95% CI: 2.79, 3.93) per 1000 births in Africa from 2000 to 2020; and this estimate was 1.7 times the infant mortality burden associated with life-span flood exposure (2.00 deaths per 1000 births, 95% CI: 1.02, 2.82) (Fig. 4B, Table S6). Similar to the distribution of flood hotspots, the areas with high infant mortality burden related to flood exposures were located in Western Africa, Eastern Africa, and East Coast of the continent (Fig. 4A). Infants in South Sudan (Western Africa), Niger (Eastern Africa), and Somalia (East Coast of the continent) suffered the highest mortality burden associated with flood exposures, with 5.91, 6.37, 6.62 excess infant deaths per 1000 births, respectively. The distribution of total excess infant deaths was also spatially consistent with the distribution of flood hotspots (Fig. S6). In addition, we observed a generally increasing trend for the number of excess infant deaths (per 1000 births) associated with flood exposure in Africa between 2000 and 2020, with a sharp rise in the last five years (Fig. 5 and Table S7).
The results were presented as excess deaths per 1000 liveborn births associated with 5-year average flood events, and illustrated in map (A, grids of 10 km × 10 km) and histograms (B, the country level). Estimates of flood-related infant mortality burden were based on exposures at lag 0–4 year, which is the average of flood exposures at the concurrent year and preceding 4 years.
Discussion
To our knowledge, this investigation conducted in 37 LIMCs of Africa is the first epidemiological study to estimate the association between flood events and infant deaths. By examining the short-, mid- and long-term associations, this study first sheds light on the overall burden of infant mortality associated with flood events. We estimated that 3.42 excess infant deaths per 1000 births may be associated with 5-year average flood exposure from 2000 to 2020, which was about 1.7 times higher than the burdens associated with life-span flood exposure. This study highlights the mid- to long-term disease burden associated with flood exposure, suggesting critical windows for disaster response. Local governments should provide social resources when encountering flood disasters, not only to safeguard child health during flood events but also to develop sustainable interventions aimed at supporting affected children in the aftermath, thereby mitigating potential long-term impacts.
In comparison, the findings from our study align with prior research linking flood exposure to child mortality. For instance, in Nepal, a severe flood led to a nearly sixfold increase in mortality rates among children (relative risk = 5.9, 95% CI: 5.0–6.8)18. Similarly, the tsunami disaster in Sri Lanka in 2004 resulted in significantly elevated mortality among children under 5 years old (OR = 5.87, 95% CI: 4.03, 8.55)19. Another study conducted in Fiji demonstrated that children residing in floodplains experienced a mortality rate as high as 16.5 per 1000 children20. However, these previous studies primarily focused on flood-related child mortality in single countries or for single flood events, which could have overestimated the risk of infant mortality related to floods in a region. Our study strengthened previous findings on the impact of flood events on children mortality using a more advanced methodology and the most representative dataset from 37 LMICs in Africa. Furthermore, previous studies only examined the immediate effect of flood exposure on child mortality, potentially underestimating the long-term risk and delayed effects of flood events. In contrast, this study identified acute effect of floods on infant death within one month, which are likely associated with the direct injuries. The association weakened and became insignificant in the following 8 months, possibly due to a “harvesting effect,” a phenomenon often observed in environmental epidemiology21,22. In other words, flood exposure could immediately pose excess premature death risk for infants in LIMCs with high baseline infant mortality rates; and thereafter the pool of vulnerable infants could be diminished, and thus there appears to be some insignificant even negative effects of flood. Subsequently, the adverse impact of flood events turned to be statistically significant at a lag of 10 month and lasted until to lag 3 year. The present study considered multiple exposure windows in months and years, providing a comprehensive assessment of the risk of infant mortality resulting from floods, spanning from the occurrence of the event to the regional recovery phase (in years).
The short-term association of the flood with infant mortality could be interpreted by several pathways. First, drowning and severe trauma are the most common causes of acute deaths during flood disasters, with children being particularly vulnerable to drowning incidents8,23,24. Second, floods potentially contaminate water sources and floodplain soil with various toxic chemical pollutants, including pesticides, organic toxins, and heavy metals25,26. The contaminants contributes to an increased risk of waterborne diseases like cholera and dysentery, as well as vector-borne diseases such as malaria and yellow fever during the flood flash27,28. Foods in storage could have become damp and started getting moldy during the flood. The consumption of corn contaminated with fumonisins was associated with an epidemic of neural tube defects29. Third, flood events potentially give rise to mental health issues, including posttraumatic stress disorder (PTSD) and depression, which can subsequently hinder the mother’s ability to provide care30, and consequently elevate the risk of infant mortality.
Another notable contribution is the identification of long-term association of flood events with infant mortality, which was also reasonable in terms of the following mechanisms. Firstly, floods can attenuate agricultural productivity and disrupt food supplies, potentially resulting in maternal and childhood malnutrition that weakens the immune system and increases susceptibility to infections or other external stressors31. Hurricane Gilbert, which struck Jamaica in 1989, was reported to have decreased the mean intake of dietary folate in the periconceptual period, and consequently increasing the incidence of live-birth neural tube defects32. The shock of crop failure may result in childhood stunting, and even death in a prolonged period, which is consistent with the mid- and long-term associations observed in this study33. Secondly, the damage inflicted by floods on household wealth and infrastructure can lead to prolonged disruptions in daily life, making the reconstruction of homes, businesses, and other structures a protracted process. Displacement from destroyed homes to temporary shelters with poor hygiene conditions increases the risk of infectious diseases among children34. Third, floods can damage roads, infrastructure, and healthcare facilities, making it challenging to access medical care, when children need it35.
Subgroup analyses revealed that female infants and those born to mothers with lower education levels were at a higher risk of mortality associated with flood exposure. A similar finding was reported in Nepal in 1993, where girls exhibited a higher flood-related mortality rate18. While infant mortality rate is typically higher in boys worldwide due to genetic and biological factors36, female infants may experience a greater mortality risk during floods, potentially due to societal discrimination against girls during such difficult situations37. Mothers with limited education may face challenges in providing adequate care for their children during extreme weather conditions38, while they also experience higher levels of stress and mental health problems during flood events39,40. Furthermore, our findings indicate that infants living in houses with basic water or sanitation infrastructures and natural roofs were more vulnerable to floods. Inadequate sanitation facilities increase the likelihood of infants being exposed to contaminated water sources and vector-borne diseases during flash floods41. Housing quality plays a crucial role in determining a household’s capacity to withstand and recover from flooding42. Homes constructed with concrete or brick could provide a safer shelter for children during flood events. In addition, homes with flood-resistant materials are less prone to become contaminated with molds after the floods. Moldy homes may contain mycotoxins that can be inhaled by babies, resulting in acute pulmonary hemorrhage and death in babies under 1 year of age43.
The burden of child mortality associated with flood exposures remains unknown. Burden of infant mortality associated with flood generally increased from 2000 to 2020 in Africa, with a steep rise over the recent five years. This rise could be associated with the more frequent and severe floods in Africa in recent years. Tramblay et al. reported significant upward trends in annual maximum discharge for rivers in Africa44. The population affected by floods have been on the rise since 1950, while the number of flood-related deaths has been consistently increasing since 199044. In the context of climate change, the projected rise in both frequency and intensity of flood events is expected to cause greater loss of life and property, particularly among individuals with lower educational attainment, substandard housing conditions, and limited financial resources5. Meanwhile, vulnerable populations in Africa usually have lesser capacity and fewer resources to recover from the shock of disasters, as governments may failed to provide adequate human security for impoverished African residents45. Pre-existing socioeconomic inequality could further hinder the ability of vulnerable households to respond effectively to floods and recover from their consequences46. Areas with high burdens of flood-related infant mortality align with flood hotspots are located in Western Africa, Eastern Africa, and the East Coast of the continent. The Niger River and the Senegal River in Western Africa, as well as the Nile River and its tributaries in Eastern Africa, are prone to flooding during the rainy season47. Additionally, the densely populated low-lying areas along the East Coast of Africa are frequently affected by tropical cyclones accompanied by heavy rainfalls, while rising sea levels further erode these coastal areas48.
This study has several notable implications. First, as a quintessential acute climate phenomenon, flood could have a long-lasting impact on human well-being that has been overlooked for decades. Policymakers should prioritize comprehensive, long-term disaster preparedness and resilience. Establishing sustained disaster recovery services, including rebuilding efforts and health assistance, is crucial for helping households recover, providing secure shelter for children, and mitigating the long-term health risks associated with flood events49. Second, this study identified several flood-vulnerable regions in Africa and reported an increasing burden of infant mortality associated with flood events in recent years. The heightened frequency and severity of floods underscore the importance of implementing effective mitigation and adaptation strategies for flood events. For example, it is imperative to establish flood forecasting systems with high temporal and spatial resolutions in flood-prone regions to enhance preparedness and response capabilities. Third, given the vulnerability associated with low education levels, flood-fragile housing materials, and inadequate sanitation facilities, local governments should provide resources to promote awareness of post-disaster child healthcare and disease prevention for vulnerable women in affected communities. Climate adaptation measures, including improvements to infrastructure, land use planning and medical resource allocation50,51, are crucial in climate-sensitive regions in response to the escalating frequency and severity of flood events in the context of climate change52.
Our study also has several limitations. First, we only utilized the DHS (Demographic and Health Survey) dataset collected in African countries, so generalizability of the findings to other regions of the world was restricted. Second, the small sample size for matched flood events and infant deaths prevented us from estimating country-specific ORs, so we had to use uniform ORs across different countries in estimating the infant mortality burden, which may introduce some degree of uncertainty. Third, disaster reporting has improved significantly in recent years due to advancements in communication technology. Therefore, floods from earlier years were more likely to be underreported. The increased burden of infant deaths related to floods may be partly associated with the rise in flood reporting rate, potentially leading to an underestimation of the associated with mortality burden in earlier years. Forth, there is a potential gap between multiple births for a mother, despite the fact that we compared flood exposures within the same mother, there are still some individual-level factors that could have changed between births. Fifth, our study only included deceased infants with surviving siblings, which may lead to an overestimation the risk and burden of infant death associated with floods. This is because infants with siblings may receive fewer resources from their families and face higher mortality risks from flood exposure compared to those without siblings. Finally, due to the inaccessibility of data on the governmental specific response to floods, we could not include mitigations or adaptations as covariates or possible modifiers in the statistical analyses.
In conclusion, this present study in 37 African countries provides novel and compelling evidence that flood events may increase infant mortality risks over the short and long terms. For the first time, we quantified the infant mortality burden associated with flood events, which had increased in Africa from 2000 to 2020 and was disproportionately distributed. Our findings emphasize the necessity of developing sustainable intervention and adaptation strategies to continuously support affected women and children in the aftermath of floods, especially for susceptible subpopulations and regions.
Methods
Study population
We utilized individual-level data of infant and their household from DHSs in African LMICs. The DHS were routinely conducted (about 3- to 5-year intervals) in over 90 LMICs53. Using a stratified two-stage cluster sampling design, the surveys collected health, behavior and sociodemographic data, covering a series of topics such as maternal and child health, malaria, environmental health. Details are provided in eMethod.
To identify eligible cases, we applied the following inclusion criteria (Fig. S1): (1) available information on whether infants were alive or dead; (2) infants’ mothers have lived in the current residence for over 10 years without relocating, and the residence have complete GPS coordinates; (3) valid records of birth date and death age. We finally used individual-level data from 114 separate surveys conducted in 37 LMICs in Africa during 1990–2020, which contained data collected from 37,808 clusters (Fig. 1). Details of the included DHSs are provided in Table S1. The publicly available population data used in this study has been reviewed and approved by ICF Institutional Review Board.
Based on the data of birth date, survival status, and death age for each infant, we created an indicator of whether the infant survived in their first year of life to estimate the mortality rate of infants. Furthermore, we collected data on various characteristics of infants and households from the DHS database, including gender, residence type (urban and rural), mother’s age, mother’s highest education, water and sanitation infrastructures, roof and floor materials.
Flood and population data
Flood data was derived from the Dartmouth Flood Observatory (DFO) database, which recorded flood events since 1985 from local news, governmental sources, or the FloodList (http://floodlist.com/). The database contains dates and affected areas of the 4712 flood events that have occurred worldwide since 1985. Information of flood events, including geographic distribution and duration, were applied to estimate individual exposures to flood events. Additionally, based on the recurrence interval and affected region, floods were divided into three grades in terms of severity: large flood events, very large events and extreme events (Table S2). We matched the experience of flood events (a binary variable) for each infant and his or her mother according to the birth date, death age (month), and household coordinates with the flood-prone periods and areas. We evaluated multiple periods of flood experience: life span for infants; monthly periods from the concurrent month (lag 0 m) of death to previous 12 months, which included single lags of 0 m to 1 m defined as short-term exposure and single lags of 2 m to 12 m defined as mid-term exposure; and yearly periods from the concurrent year (moving 12 months) of death to the previous 5 years (i.e., single lags of 0 y to 5 y defined as long-term exposure). To estimate the flood exposure for alive siblings (controls), we calculated their (or mothers’) experience of flood events in the same exposure windows starting from the date when their ages were same as the decedent sibling’s death age.
We obtained meteorological data (ambient temperature and precipitation) from ERA-5, a global reanalysis dataset on latitude-longitude grids at a spatial resolution of ~0.25° × 0.25° and up to 1-h temporal frequency54. Based on the available geocoded coordinates for each household, we assigned daily mean temperature and daily cumulative precipitation from Jan 1, 1980, to Dec 31, 2020, and then computed the corresponding annual/monthly average temperature and cumulative precipitation for each infant in the same time windows as the flood experience.
We further collected country-specific infant mortality for the survey year from the United Nations Children’s Fund (UNICEF) Data Warehouse (https://data.unicef.org/dv_index/). The population of infant during 2000–2020 was obtained from the Gridded Population of the World (WorldPop, version 4) at a spatial resolution of 1 km, and further aggregated into a regular grid by 10 × 10 km. The Gross Domestic Product (GDP) per capita with a resolution of 30 arc-s was obtained from a gridded global dataset for GDP55. The Crop Production Index (CPI) for each African country in the survey year were derived from the World Bank.
Statistical analyses
Association of flood and infant mortality
This study employed a sibling-matched, case-control design to investigate the potential relationship between flood exposure and infant mortality. Specifically, the study included the deceased infant (case) who has at least one alive child (control) born from the same mother. By matching cases and controls from the same mother, the design could account for individual-level or household-level confounders that were time-invariant (e.g., genetic factors) or did not change considerably with time (e.g., socioeconomic status, lifestyles). This study design may facilitate the statistical inference by examining the association between temporal changes in environmental exposure and health outcomes within the same household.
We applied a conditional logistic regression model to quantitatively estimate the associations between flood exposure during multiple periods and infant mortality. To control for time trends in the risk of infant mortality, we adjusted for mother’s age at the time of infant death (or the counterpart controls), as well as two categorical terms for the year and month of infant death (or the counterpart controls). There is an observed increase in mortality with higher birth orders, so the model was further adjusted for birth order for each infant. To control for the confounding effects of meteorological factors, the model was adjusted by a smoothing function with natural cubic splines for mean temperature (6 degrees of freedom) and for cumulative precipitation (3 degrees of freedom) during the corresponding exposure windows. In addition, we incorporated gridded GDP per capita and country-level CPI into the model to account for local economic conditions and food insecurity. ID of mother was included as a stratum-level intercept in the main model.
The effect estimates were presented as odds ratios (ORs) and their 95% confidence intervals (CI) of infant mortality associated with each flood event. To better facilitate risk communications, ORs were converted into changes in the number of infant deaths associated with a flood event per 1000 births (briefed as change of infant mortality) using the following Eqs. (1–3):
where β is the regression coefficient and SE is the standard error of the estimation. \({{IM}}_{{cy}}\) was the infant mortality for each African country c in the survey year y.
We estimated the change of infant mortality associated with flood exposure in various periods. Same regression models were separately applied for floods of varied severity (large event, and very large or extreme event).
Additionally, we conducted stratified analyses to explore how the associations varied by residential type, infant gender, mother’s highest education level, water infrastructure, sanitation infrastructure, roof material and floor material.
To test the robustness of the associations, we conducted four separate sensitivity analyses. First, we fitted four separate models by adjusting for covariates one by one in the models. Second, we excluded different covariates from the Main model. Third, we used a GLMM with the same covariates as the Main model, except that “country” or “mother ID” was adjusted as a random-effect term. Finally, we tested the sensitivity of the main estimates by leaving each country out of the analysis individually, in turn (Details of the sensitivity analyses were shown in the eMethod).
Estimation of infant mortality burden associated with flood events
We calculated the excess deaths of infants associated with flood exposure using the following Eq. (4):
Here, i represents grid i, y represents the survey year y, and RR is the relative risk of infant mortality related to flood exposure from the current year to the following 4 years (lag 0–4 y). \({{ED}}_{{iy}}\) denotes the excess deaths of infants in grid i over the year y. \({F}_{{iy}}\) is the identified total number of flood events in corresponding grid and survey year. \({D}_{{iy}}\) represents the number of infant deaths, which was calculated using the total number of infants in grid i and infant mortality rate of the country that includes the grid i during the year y. We then calculated the excess deaths of infants per 1000 births associated with flood exposure at the grid level. Based on the gridded infant mortality burden for each year between 2000 and 2020, we mapped the spatial distribution and temporal trends of the infant mortality burden associated with flood.
We conducted all statistical analyses in R (Version 4.0.5). The function clogit in package “survival” was applied to fit conditional logistic regression. All statistical tests were two-sided and a p-value < 0.05 was considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The individual and household data for each infant generated in this study have been deposited in the Demographic and Health Surveys (DHS) database (https://dhsprogram.com/). The DHS data are under a data-sharing agreement and were publicly available upon request. The data generated in this study are provided in the Source Data file. Flood data are also publicly available from The Flood Observatory (https://floodobservatory.colorado.edu/). The number of infants at a spatial resolution of 1 km for each country was obtained from the WorldPop database (https://hub.worldpop.org/geodata/listing?id=19). Source data are provided with this paper.
Code availability
R codes for statistical analysis are available from the corresponding authors, Renjie Chen ([email protected]). We will respond to the requests within 2 weeks.
References
CRED UNISDR. The human cost of natural disasters: a global perspective (2015).
Alfieri, L. et al. Global projections of river flood risk in a warmer world. Earth’s Future 5, 171–182 (2017).
Arnell, N. W. & Gosling, S. N. The impacts of climate change on river flood risk at the global scale. Clim. Change 134, 387–401 (2016).
Hirabayashi, Y. et al. Global flood risk under climate change. Nat. Clim. Change 3, 816–821 (2013).
Winsemius, H. C. et al. Global drivers of future river flood risk. Nat. Clim. Change 6, 381–385 (2016).
Alderman, K., Turner, L. R. & Tong, S. Floods and human health: a systematic review. Environ. Int. 47, 37–47 (2012).
Mallett, L. H. & Etzel, R. A. Flooding: what is the impact on pregnancy and child health? Disasters 42, 432–458 (2018).
Tan, H. et al. Change in global burden of unintentional drowning from 1990 to 2019 and its association with social determinants of health: findings from the Global Burden of Disease Study 2019. BMJ Open 13, e070772 (2023).
Koelle, K., Rodó, X., Pascual, M., Yunus, M. & Mostafa, G. Refractory periods and climate forcing in cholera dynamics. Nature 436, 696–700 (2005).
The Lancet, M. Climate change: fires, floods, and infectious diseases. Lancet Microbe 2, e415 (2021).
Warraich, H., Zaidi, A. K. & Patel, K. Floods in Pakistan: a public health crisis. Bull. World Health Organ. 89, 236–237 (2011).
Rodriguez-Llanes, J. M., Ranjan-Dash, S., Degomme, O., Mukhopadhyay, A. & Guha-Sapir, D. Child malnutrition and recurrent flooding in rural eastern India: a community-based survey. BMJ Open 1, e000109 (2011).
Rodriguez-Llanes, J. M., Ranjan-Dash, S., Mukhopadhyay, A. & Guha-Sapir, D. Flood-exposure is associated with higher prevalence of child undernutrition in rural eastern India. Int. J. Environ. Res. Public Health 13, 210 (2016).
Datar, A., Liu, J., Linnemayr, S. & Stecher, C. The impact of natural disasters on child health and investments in rural India. Soc. Sci. Med. 76, 83–91 (2013).
Reed, C. et al. The impact of flooding on food security across Africa. Proc. Natl Acad. Sci. 119, e2119399119 (2022).
Kakinuma, K. et al. Flood-induced population displacements in the world. Environ. Res. Lett. 15, 124029 (2020).
Godber, O. F. & Wall, R. Livestock and food security: vulnerability to population growth and climate change. Glob. Change Biol. 20, 3092–3102 (2014).
Pradhan, E. K. et al. Risk of flood‐related mortality in Nepal. Disasters 31, 57–70 (2007).
Nishikiori, N. et al. Who died as a result of the tsunami?–Risk factors of mortality among internally displaced persons in Sri Lanka: a retrospective cohort analysis. BMC Public Health 6, 1–8 (2006).
Yeo, S. W. & Blong, R. J. Fiji’s worst natural disaster: the 1931 hurricane and flood. Disasters 34, 657–683 (2010).
Schwartz, J. Harvesting and long term exposure effects in the relation between air pollution and mortality. Am. J. Epidemiol. 151, 440–448 (2000).
Saha, M. V., Davis, R. E. & Hondula, D. M. Mortality displacement as a function of heat event strength in 7 US cities. Am. J. Epidemiol. 179, 467–474 (2014).
Ragan, P., Schulte, J., Nelson, S. J. & Jones, K. T. Mortality surveillance: 2004 to 2005 Florida hurricane-related deaths. Am. J. Forensic Med. Pathol. 29, 148–153 (2008).
Haines, A., Kovats, R. S., Campbell-Lendrum, D. & Corvalán, C. Climate change and human health: impacts, vulnerability and public health. Public Health 120, 585–596 (2006).
Crawford, S. E. et al. Remobilization of pollutants during extreme flood events poses severe risks to human and environmental health. J. Hazard Mater. 421, 126691 (2022).
Ponting, J., Kelly, T. J., Verhoef, A., Watts, M. J. & Sizmur, T. The impact of increased flooding occurrence on the mobility of potentially toxic elements in floodplain soil–A review. Sci. Total Environ. 754, 142040 (2021).
Levy, K., Woster, A. P., Goldstein, R. S. & Carlton, E. J. Untangling the impacts of climate change on waterborne diseases: a systematic review of relationships between diarrheal diseases and temperature, rainfall, flooding, and drought. Environ. Sci. Technol. 50, 4905–4922 (2016).
Hunter, P. R. Climate change and waterborne and vector‐borne disease. J. Appl. Microbiol. 94, 37–46 (2003).
Missmer, S. A. et al. Exposure to fumonisins and the occurrence of neural tube defects along the Texas-Mexico border. Environ. Health Perspect. 114, 237–241 (2006).
Neria, Y. & Shultz, J. M. Mental health effects of Hurricane Sandy: characteristics, potential aftermath, and response. JAMA 308, 2571–2572 (2012).
Phalkey, R. K., Aranda-Jan, C., Marx, S., Höfle, B. & Sauerborn, R. Systematic review of current efforts to quantify the impacts of climate change on undernutrition. Proc. Natl Acad. Sci. 112, E4522–E4529 (2015).
Duff, E. M. & Cooper, E. S. Neural tube defects in Jamaica following Hurricane Gilbert. Am. J. Public Health 84, 473–476 (1994).
Yamano, T., Alderman, H. & Christiaensen, L. J. A. Jo. A. E. Child growth, shocks, and food aid in rural Ethiopia. Am. J. Agr. Econ. 87, 273–288 (2005).
Doocy, S., Daniels, A., Murray, S. & Kirsch, T. D. The human impact of floods: a historical review of events 1980-2009 and systematic literature review. PLoS Curr. 5 (2013).
Ohl, C. A. & Tapsell, S. Flooding and human health: the dangers posed are not always obvious. BMJ 321, 1167–1168 (2000).
Pongou, R. Why is infant mortality higher in boys than in girls? A new hypothesis based on preconception environment and evidence from a large sample of twins. Demography 50, 421–444 (2013).
Guilmoto, C. Z., Saikia, N., Tamrakar, V. & Bora, J. K. Excess under-5 female mortality across India: a spatial analysis using 2011 census data. Lancet Glob. Health 6, e650–e658 (2018).
Dimitrova, A. & Muttarak, R. After the floods: differential impacts of rainfall anomalies on child stunting in India. Glob. Environ. Change 64, 102130 (2020).
Munro, A. et al. Effect of evacuation and displacement on the association between flooding and mental health outcomes: a cross-sectional analysis of UK survey data. Lancet Planet Health 1, e134–e141 (2017).
Abass, K., Gyasi, R. M., Katey, D., Frempong, F. & Garsonu, E. K. Flood exposure and psychological distress among Ghanaian adults in flood-prone settings. Sci. Total Environ. 835, 155481 (2022).
Paterson, D. L., Wright, H. & Harris, P. N. Health risks of flood disasters. Clin. Infect. Dis. 67, 1450–1454 (2018).
Anderson, S. E. et al. The dangers of disaster-driven responses to climate change. Nat. Clim. Change 8, 651–653 (2018).
Budolfson, K. C. & Etzel, R. A. Climate change and child health equity. Pediatr. Clin. N. Am. 70, 837–853 (2023).
Tramblay, Y., Villarini, G. & Zhang, W. Observed changes in flood hazard in Africa. Environ. Res. Lett. 15, 1040b1045 (2020).
Douglas, I. Flooding in African cities, scales of causes, teleconnections, risks, vulnerability and impacts. Int. J. Disaster Risk Reduct. 26, 34–42 (2017).
Masozera, M., Bailey, M. & Kerchner, C. Distribution of impacts of natural disasters across income groups: a case study of New Orleans. Ecol. Econ. 63, 299–306 (2007).
Nicholson, S. E. & Yin, X. Rainfall conditions in equatorial East Africa during the nineteenth century as inferred from the record of Lake Victoria. Clim. Change 48, 387–398 (2001).
Magadza, C. H. Climate change impacts and human settlements in Africa: prospects for adaptation. Environ. Monit. Assess. 61, 193–205 (2000).
Azad, A. K., Hossain, K. M. & Nasreen, M. Flood-induced vulnerabilities and problems encountered by women in northern Bangladesh. Int. J. Disaster Risk Sci. 4, 190–199 (2013).
Shah, A. A. et al. Reconnoitering school children vulnerability and its determinants: evidence from flood disaster-hit rural communities of Pakistan. Int. J. Disaster Risk Reduct. 70, 102735 (2022).
Yang, Z. et al. Mortality risks associated with floods in 761 communities worldwide: time series study. BMJ 383, e075081 (2023).
Tellman, B. et al. Satellite imaging reveals increased proportion of population exposed to floods. Nature 596, 80–86 (2021).
https://www.dhprogram.com ICF international. Demographic and Health Surveys Program. Accessed Dec 1, 2022.
Hersbach, H. et al. The ERA5 global reanalysis. Q. J. R. Meteorol. Soc. 146, 1999–2049 (2020).
Kummu, M., Taka, M. & Guillaume, J. H. Gridded global datasets for gross domestic product and Human Development Index over 1990–2015. Sci. Data 5, 1–15 (2018).
Acknowledgements
This work was supported by National Natural Science Foundation of China (82430105) (Dr Kan), Shanghai Municipal Science and Technology Major Project (2023SHZDZX02) (Dr Kan), Shanghai B&R Joint Laboratory Project (22230750300) (Dr Kan), Shanghai International Science and Technology Partnership Project (21230780200) (Drs Chen and Kan), and a grant from the Alexander von Humboldt Foundation for the Humboldt Research Fellowship (Dr He).
Author information
Authors and Affiliations
Contributions
H.K. and R.C. are the joint corresponding authors and contributed to the conceptualization, funding acquisition, project administration, and supervision of the study. Y.Z. and C.H. coordinated the work, conducted the statistical analysis, and took the lead in drafting the manuscript and interpreting the results. Y.Z. and L.Z. contributed to data collection. Y.Z., C.H., J.B., Z.F., J.L., C.L., and R.C. contributed to interpretation of the results and to drafting the manuscript. All authors contributed to the development of the manuscript and approved the final draft.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Debarati Guha, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, Y., He, C., Bachwenkizi, J. et al. Burden of infant mortality associated with flood in 37 African countries. Nat Commun 15, 10171 (2024). https://doi.org/10.1038/s41467-024-54561-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-54561-y
This article is cited by
-
Adaptive capacity for multimodal transport network resilience to extreme floods
Nature Sustainability (2025)