Abstract
Survival outcomes of patients with heart failure (HF) based on their disease etiology are not well described. Here, we provide one-year mortality outcomes of 10850 patients with HF (mean age = 59.9 years, 31% women) in India. Ischemic heart disease (71.9%), dilated cardiomyopathy (17.3), rheumatic heart disease (5.4), non-rheumatic valvular heart disease (1.9), hypertrophic cardiomyopathy (0.8), congenital heart disease (0.7), peri-partum cardiomyopathy (0.5), restrictive cardiomyopathy (0.4), and infective endocarditis (0.1) were the main disease etiologies. Mortality rate per 100-person years of follow-up varied from 13.8 (95% CI: 6.2–30.7) in peri-partum cardiomyopathy to 92.9 (46.5–185.9) in infective endocarditis. Compared to ischemic heart disease, the mortality was two to five times higher in rheumatic heart disease (HR = 2.0; 95% CI: 1.6–2.4), congenital heart disease (2.9; 1.9–4.2), and infective endocarditis (4.8; 2.4–9.8). The wide variations in mortality rate in HF patients may bring possible clinical applicability of risk stratification.
Similar content being viewed by others
Introduction
Globally, heart failure (HF) is a significant public health problem with rising prevalence and high mortality rates1,2,3. The high incidence of premature coronary artery disease and type II diabetes, along with environmental factors like air pollution, contribute to the high burden of HF in regions like South Asia3. Despite the availability of guideline-directed medical therapies in subgroups of HF patients and improvements in survival over the last one to two decades4,5, the mortality rate, especially in low and middle-income countries (LMICs)6,7,8,9,10,11, remains very high. The prognostic significance of left ventricular ejection fraction and risk stratification of HF patients into three difference groups (heart failure with reduced ejection fraction-HFrEF, heart failure with mildly reduced ejection fraction-HFmrEF, and heart failure with preserved ejection fraction-HFpEF) are well known12. Global epidemiology of HF over the last two decades has improved our understanding of the complexity of this condition. However, the causes, incidence, progress in the presentation, and outcomes of HF have not been studied in detail in LMICs. Although HF is a multimorbid condition, it is often associated with a predominant primary disease etiology. Data on the prognostic significance of the disease etiology of HF and survival outcomes stratified by different etiologies are scarce in LMICs.
Ischemic heart disease (IHD) is the predominant disease etiology in both high-income and LMICs2,3,6,8,13. A relatively higher mortality rate in HF among individuals with IHD etiology than other disease etiologies is noted in several studies14,15,16. Given the predominance of IHD and a relatively small number of participants with other disease etiologies in most previous studies, an etiology-based meaningful comparison of mortality event rates was not possible.
Heart failure registries are often restricted to selected geographical areas in LMICs3,6,10,17. In countries like India, with wide heterogeneity in epidemiological transition, access to acute care, and health system readiness to manage patients with chronic conditions across different states and districts, extrapolating data from regional studies has severe limitations. Our understanding of HF in India is limited concerning the variations in risk factors, disease etiology, and etiology-specific outcomes. Hence, we set up the National Heart Failure Registry in 53 centers with representations from all different regions of India based on various stages of epidemiological transition. A deeper understanding of the disease etiology-specific outcomes may aid in therapeutic progress, resource allocation, and the development of holistic care models to manage HF. This article describes the one-year mortality in HF patients from India by the predominant disease etiology.
Results
Demographic and clinical characteristics
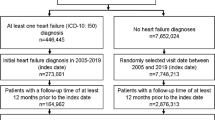
A total of 10850 participants were enrolled in the NHFR. More than two-thirds of the participants were men (68.9%). Nearly half of the population had education beyond primary school or more than four years of formal education. Sixty-five percent and 13% of participants had HF with reduced ejection fraction and HF with preserved ejection fraction, respectively. The rest of them had HFmrEF (HF with mildly reduced EF).
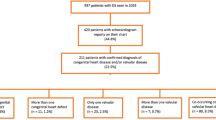
Of the 10850 patients, the primary disease etiology was identified in 10845 patients. Subsequent data presented in this paper are restricted to this population with disease etiology. Ischemic heart disease (IHD) was the most common etiology in 7800 (71.9%) patients (Table 1). It was the predominant etiology in men and women (Table S1A and S1B). Dilated cardiomyopathy was the primary disease etiology in 1877 (17.3%) patients. Rheumatic valvular heart disease and non-rheumatic valvular heart disease were the primary etiology in 586 (5.4%) and 211 (1.9%) patients, respectively. Congenital heart disease was the disease etiology in 78 (0.7%) patients. Hypertrophic, peripartum, and restrictive cardiomyopathies were the predominant disease etiologies in 92 (0.8%), 49 (0.5%), and 38 (0.4%) patients, respectively. Among 16 patients, the disease etiology was noted as infective endocarditis.
The mean age ranged from 29.2 years (SD = 6.1) in peripartum cardiomyopathy patients to 61.9 years (SD = 11.9) in patients with ischemic heart disease etiology. Overall, women comprised one-third of the total population. However, the proportion of women was more than 50% when the disease etiology was rheumatic valvular heart disease or congenital heart disease. Heart failure patients with disease etiologies of non-rheumatic valvular heart disease, hypertrophic cardiomyopathy, and restrictive cardiomyopathy also showed disproportionally higher women.
The prevalence of hypertension ranged from 14.2% in peripartum cardiomyopathy to 68.5% in hypertrophic cardiomyopathy. Diabetes prevalence was 49.1% in patients with ischemic heart disease etiology. In comparison, it was less than 25% in patients with disease etiologies of rheumatic heart disease, congenital heart disease, restrictive cardiomyopathy, and infective endocarditis. Chronic obstructive pulmonary disease (COPD) and chronic kidney disease (CKD) prevalence did not vary substantially between patients with different disease etiologies. Stroke and atrial fibrillation were prevalent in 2.9% and 9.5% of the study population.
One-year mortality and re-admission outcomes
Of the 10850 participants recruited into NHFR, 4.8% (n = 524) participants were lost to follow-up, resulting in a one-year follow-up rate of 95.2%. During the index hospitalization, 728 participants died, and another 1674 participants died during the one-year follow-up period, resulting in a cumulative one-year all-cause mortality rate of 22.1% (n = 2402). The all-cause mortality rate was 26.3 and 28.9 per 100-person year in men and women, respectively (Table S2A and S2B). The re-admission rate was 17.2% in one year.
The mortality rate was high in infective endocarditis (50.0%), congenital heart disease (34.6%), and restrictive cardiomyopathy (36.8%) as compared to other disease etiologies (Table 2). Mortality rate per 100-person years of follow-up varied from 13.8 (95% CI: 6.2–30.7) in peripartum cardiomyopathy to 92.9 (46.5–185.9) in infective endocarditis. The mortality rate in HF patients with ischemic heart disease etiology was 25.7 per 100 person-years (Fig. 1). In the Kaplan–Meier survival curve analysis, HF patients with congenital heart disease, dilated cardiomyopathy or peripartum cardiomyopathy, and non-rheumatic or rheumatic valvular heart disease, or infective endocarditis showed higher mortality rate (log-rank p < 0.001) than those with other disease etiologies (Fig. 2). In the Cox-proportional hazard model, the mortality rate was twice as high in rheumatic heart disease (HR = 2.0; 95% CI: 1.6–2.4), thrice in congenital heart disease (2.9; 1.9–4.2), and five-times higher in infective endocarditis (4.8; 2.4–9.8) compared to ischemic heart disease (Fig. 3 and Table 3).
Adjusted mortality rates per 100 person-years and their 95% confidence interval. The error bars indicate the 95% Confidence Interval (n = 10,845). IHD ischemic heart disease, CHD=congenital heart disease, DCM dilated cardiomyopathy, RHD rheumatic heart disease, Other CM other cardiomyopathy, NRHD=non-rheumatic valvular heart disease, IE infective endocarditis.
IHD ischemic heart disease, CHD congenital heart disease, DCM dilated cardiomyopathy, PPCM peri-partum cardiomyopathy, HCM hypertrophic cardiomyopathy, RCM restrictive cardiomyopathy, RHD rheumatic heart disease, NRHD non-rheumatic valvular heart disease, IE infective endocarditis. The Kaplan–Meier survival curves are compared using the log-rank test.
Results from multi-variable proportional hazard model. The error bars indicate the 95% Confidence Interval (n = 10,845). IHD=ischemic heart disease, CHD congenital heart disease, DCM dilated cardiomyopathy, RHD rheumatic heart disease, Other CM other cardiomyopathy, NRHD non-rheumatic valvular heart disease, IE infective endocarditis.
Readmissions to hospitals during the study period were highest in cases of infective endocarditis (25.0%, n = 4), restrictive cardiomyopathy (21.1%, n = 8), congenital heart disease (21.8%, n = 17), and others (24.5%, n = 24). A low rate of readmissions was observed among patients with peripartum cardiomyopathy (12.2%, n = 6) and those with non-rheumatic valvular heart disease (13.7%, n = 29). The re-admission rate in HF patients with ischemic heart disease etiology was 16.7% (n = 1301). There were 353 (18.8%) and 101 (17.2%) re-admission events in HF patients with dilated cardiomyopathy and rheumatic heart diseases, respectively. The re-admission rate was 19.6% (n = 18) in HF patients with hypertrophic cardiomyopathy.
Discussion
The NHFR is India’s first nationally representative HF registry with prospective follow-up data. Our study population was almost ten years younger than HF patients in registries from high-income settings. Ischaemic heart disease is the predominant disease etiology in two-thirds of HF patients in the NHFR. We report a one-year mortality rate of 22.1% and a re-admission rate of 17.2% in the NHFR cohort. However, the prognosis and survival rate depend primarily on the underlying disease etiology. In contrast to the reports from HF registries in high-income regions, NHFR showed substantially higher mortality rates in HF patients with rheumatic heart disease, congenital heart disease, and infective endocarditis compared to ischemic heart disease.
In our cohort, the lowest mortality was among patients with peripartum and hypertrophic cardiomyopathy (12–13%). A one-year mortality rate of 8.4% was reported in the recent European Society of Cardiology peripartum cardiomyopathy registry18. The relatively lower mortality risk in hypertrophic cardiomyopathy, as observed in our cohort, is well documented, with low-risk HCM patients experiencing a survival rate like the general population19. Infective endocarditis was a disease with high mortality (50%) in the NHFR registry. The in-hospital and one-year mortality reported from the Brandenburg endocarditis registry was 28.4% and 40.9%, respectively20. Late diagnosis and lack of adequate bacterial/fungal culture facilities, lack of early surgical intervention may be contributing to the high mortality in infective endocarditis. The mortality rate of patients with dilated cardiomyopathy in the NHFR was moderately higher than patients with ischemic heart disease etiology. However, the mortality rate in dilated cardiomyopathy in NHFR was substantially higher than reported from high-income countries21,22.
The high mortality associated with rheumatic heart disease and congenital heart disease in the NHFR cohort has important implications, especially in the LMIC context. Untreated congenital heart disease is a risk factor for the development of irreversible pulmonary hypertension, and subsequent ventricular dysfunction leading to HF. In one of the largest registries of pulmonary hypertension in adult patients (n = 2003) from India, 291/424 (69%) patients with group 1 pulmonary hypertension were due to untreated congenital heart disease23. Furthermore, many of them had a repairable defect (by catheter interventions or by surgery), which could have been easily managed in early life. Screening of newborns, screening during vaccination visits, and regular school health check-ups help detect congenital heart disease at an early stage. Appropriate management of congenital heart disease early in life prevents pulmonary hypertension development and progression to HF.
Unlike the other HF registries in the high-income regions, the mortality rate in the NHFR was relatively higher in individuals with rheumatic heart disease etiology. Rheumatic heart disease is still common in LMICs like India and causes significant morbidity and mortality24. Lack of awareness about acute rheumatic fever, poor compliance with penicillin prophylaxis, and late presentation contribute to the high prevalence of rheumatic heart disease in LMICs. Lack of timely corrective therapies due to accessibility, availability, and affordability issues leads to complications such as HF in several such patients25. Improvement in secondary prophylaxis, echocardiography-based screening of school children, and subsidized surgical and interventional strategies may help to reduce the burden of rheumatic heart disease and prevent the development of complications such as HF.
In contrast to the findings from NHFR, there were no mortality differences between patients in the PARADIGM-HF trial16 according to their disease etiology after adjustment for other prognostic variables, including natriuretic peptides. However, natriuretic peptides are not routinely estimated in the Indian context. In the NHFR, only a tiny fraction of patients have natriuretic peptide levels measured at the initial admission.
The NHFR is the first registry from India with pan-India representation. The follow-up rate of 95.2% is one of the study’s main strengths. Detailed clinical assessment by a trained clinical cardiologist and availability of echocardiography in all the patients before enrollment are other strengths. Limitations include the lack of in-person clinical follow-up, as telephonic follow-up needs to be done for many patients, primarily due to the COVID-19 pandemic during the data collection period. The cause of death could not be ascertained in all patients. We did not recruit patients attending outpatient departments and those who could not access hospitals for HF management.
Heart failure-specific registries serve several purposes in LMICs. It helps recognize individual presentation and outcome variations. Furthermore, it also helps refine patient groups for personalized interventions. The heterogeneous pathophysiology of HF is known, as it is greatly affected by the nature of the underlying cardiac disease26. Heart failure patients with different underlying cardiac diseases may respond best to distinct treatment strategies. The differential outcomes by disease etiology may help probe HF’s underlying pathophysiological and molecular mechanisms.
In conclusion, one in four HF patients in India die within one year of follow-up during their productive life years. There is wide variation in the one-year mortality rate in HF patients according to the predominant disease etiology. Risk stratification and targeted management should focus on disease etiology in HF patients.
Methods
Study settings
The design and detailed methods of NHFR have already been published8,27. In short, NHFR is a hospital-based registry of acute decompensated HF (ADHF) patients admitted to 53 hospitals in 21 states and four union territories in India. The recruitment was done from January 2019 to July 2020. The nine nodal centres located in different regions in India recruited five participating centres under each of them. This process ensured adequate representation of India’s other geographical regions and ethnicities in the NHFR. All consecutive ADHF patients >18 years who satisfied the ESC (European Society of Cardiology) 2016 diagnostic criteria(16) were enrolled in the registry. We obtained the necessary institutional ethics committee approval from all participating sites. The study was registered in the Clinical Trial Registry of India (CTRI/2019/01/017053). A written informed consent was obtained from all participants before recruitment into the registry. The Institute Ethics Committee of Sree Chitra Tirunal Institute for Medical Sciences and Technology, Trivandrum approved the study (IEC/1167).
We defined the predominant disease etiology by standard criteria as follows. An experienced cardiologist described the disease etiology by using the usual clinical criteria.
-
1.
Ischemic heart disease (IHD): All patients with a history of prior myocardial infarction or coronary intervention, either coronary angioplasty or coronary artery bypass graft surgery. This group also included patients with a history of chest pain and had ECG or echocardiographic or angiographic evidence of obstructive coronary artery disease.
-
2.
Dilated cardiomyopathy (DCM): All patients with impaired ventricular function when another distinct etiology could not be ascertained.
-
3.
Hypertrophic cardiomyopathy (HCM): Defined as a diastolic left ventricular wall thickness of more than 15 mm in one or more segments without hypertension and aortic stenosis.
-
4.
Restrictive cardiomyopathy (RCM): Defined as diastolic dysfunction with preserved systolic function, non-dilated ventricles associated with atrial dilatation, and ± ventricular hypertrophy.
-
5.
Peripartum cardiomyopathy (PPCM): Unexplained heart failure with reduced ejection fraction in young women toward the end of pregnancy or in the first six months following delivery.
-
6.
Rheumatic heart disease (RHD): Diagnosis was based on the World Heart Federation criteria28.
-
7.
Non-RHD Valve disease: Patients with significant valvular heart disease without features of RHD. IHD-associated valve involvement was excluded from this group.
-
8.
Congenital Heart Disease (CHD): Defined as a hemodynamic abnormality present at birth and contributing as the primary reason for HF.
Follow-up
We conducted follow-up of all patients enrolled in the NHFR at regular intervals. The primary follow-up time points were three months, six months, and one year. Vital status and hospital readmission history were assessed at the follow-up visits. The follow-up visits are mainly conducted over the telephone. Information on death, date of death, and cause of death (if available) were gathered during the follow-up visits.
Outcome measures
The primary outcome variable was all-cause mortality. We also collected hospital readmissions. All outcome data were right censored for one year. We used the time to mortality data in the survival analysis as the primary outcome variable.
Statistical analysis
We provided summary statistics (mean, standard deviation, and proportion with numerator and denominator) of baseline sociodemographic and clinical variables stratified by predominant disease etiology. We reported a one-year cumulative mortality rate and mortality rate per 100 person-years of follow-up with their 95% confidence interval. Mortality and readmission data were stratified by disease etiology. Kaplan–Meier survival models were performed initially after checking the proportional hazards assumption using log-minus-log plots, and groups based on disease etiologies were compared using log-rank tests. Further, we employed a multivariate Cox-proportional hazard model. We presented the adjusted hazard ratio (adjusted for age, gender, epidemiological transition levels, education, type of heart failure, hypertension, diabetes, COPD, and CKD) with their 95% confidence interval for different etiological conditions compared to ischemic heart disease etiology. All analyzes were carried out using Stata 16.1 Stata Corp LLC.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Data supporting the findings of this study are available in the article, its supplementary information, the source data file, and from the corresponding author upon request. Source data are provided with this paper.
References
Roger, V. L. Epidemiology of heart failure: a contemporary perspective. Circ. Res. 128, 1421–1434 (2021).
Bozkurt, B. et al. Heart failure epidemiology and outcomes statistics: a report of the Heart Failure Society of America. J. Card. Fail. 29, 1412–1451 (2023).
Martinez-Amezcua, P. et al. The upcoming epidemic of Heart Failure in South Asia. Circ. Heart Fail. 13, e007218 (2020).
Taylor, C. J. et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study. BMJ 364, l223 (2019).
Conrad, N. et al. Temporal trends and patterns in mortality after incident heart failure: a longitudinal analysis of 86000 individuals. JAMA Cardiol. 4, 1102–1111 (2019).
Dokainish, H. et al. Global mortality variations in patients with heart failure: results from the International Congestive Heart Failure (INTER-CHF) prospective cohort study. Lancet Glob. Health 5, e665–e672 (2017).
Ganapathi, S. et al. Early and long-term outcomes of decompensated heart failure patients in a tertiary-care centre in India. ESC Heart Fail. 7, 467–473 (2020).
Harikrishnan, S. et al. Clinical profile and 90 day outcomes of 10 851 heart failure patients across India: National Heart Failure Registry. ESC Heart Fail. 9, 3898–3908 (2022).
Harikrishnan, S. et al. Five-year mortality and readmission rates in patients with heart failure in India: results from the Trivandrum heart failure registry. Int J. Cardiol. 326, 139–143 (2021).
Joseph, S., et al. The Cardiology Society of India-Kerala Acute Heart Failure Registry: poor adherence to guideline-directed medical therapy. Eur. Heart J. 43, 908–915 (2021).
Sanjay, G. et al. In-hospital and three-year outcomes of heart failure patients in South India: the Trivandrum Heart failure registry. J. Card. Fail. 24, 842–848 (2018).
McDonagh T. A., et al. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. J. Heart Fail. 44, 3627–3639 (2024).
Vedin, O. et al. Significance of ischemic heart disease in patients with heart failure and preserved, midrange, and reduced ejection fraction: a nationwide cohort study. Circ. Heart Fail. 10, e003875 (2017).
Spitaleri, G. et al. Cause of death in heart failure based on etiology: long-term cohort study of all-cause and cardiovascular mortality. J. Clin. Med. 11, 784 (2022).
Kajimoto, K., Minami, Y., Sato, N. & Kasanuki, H. Investigators of the Acute Decompensated Heart Failure Syndromes Registry Etiology of heart failure and outcomes in patients hospitalized for acute decompensated heart failure with preserved or reduced ejection fraction. Am. J. Cardiol. 118, 1881–1887 (2016).
Balmforth, C. et al. Outcomes and effect of treatment according to etiology in HFrEF. JACC Heart Fail. 7, 457–465 (2019).
Harikrishnan, S. et al. Clinical presentation, management, in-hospital and 90-day outcomes of heart failure patients in Trivandrum, Kerala, India: the Trivandrum heart failure registry. Eur. J. Heart Fail. 17, 794–800 (2015).
Jackson, A. M., et al. Outcomes at 1 year in women with peripartum cardiomyopathy: findings from the ESC EORP PPCM Registry. Eur. J. Heart Fail. 26, 34–42 (2023).
Maron, B. J. et al. Management of hypertrophic cardiomyopathy: JACC state-of-the-Art review. J. Am. Coll. Cardiol. 79, 390–414 (2022).
Ostovar, R., et al. Mortality related risk factors: results from the Brandenburg Endocarditis Register. Thorac. Cardiovasc. Surg. 72, 587–594 (2023).
Dziewiecka, E. et al. Mortality risk in dilated cardiomyopathy: the accuracy of heart failure prognostic models and dilated cardiomyopathy-tailored prognostic model. ESC Heart Fail. 7, 2455–2467 (2020).
Silverdal, J. et al. Prognostic differences in long-standing vs. recent-onset dilated cardiomyopathy. ESC Heart Fail. 9, 1294–1303 (2022).
Harikrishnan, S. et al. Pulmonary Hypertension Registry of Kerala (PROKERALA)—rationale, design and methods. Indian Heart J. 68, 709–715 (2016).
Negi, P. C. et al. Long term outcomes in patients with RF/RHD: eight-year follow-up of HP-RF/RHD (Himachal Pradesh Rheumatic Fever/Rheumatic Heart Disease) registry in a Northern Indian state. Int. J. Cardiol. 343, 149–155 (2021).
Vervoort, D. et al. Tertiary prevention and treatment of rheumatic heart disease: a National Heart, Lung, and Blood Institute working group summary. BMJ Glob. Health 8, e012355 (2023).
Schwinger, R. H. G. Pathophysiology of heart failure. Cardiovasc Diagn. Ther. 11, 263–276 (2021).
Harikrishnan, S. et al. National Heart Failure Registry, India: design and methods. Indian Heart J. 71, 488–491 (2019).
Rwebembera, J. et al. 2023 World Heart Federation guidelines for the echocardiographic diagnosis of rheumatic heart disease. Nat. Rev. Cardiol. 21, 250–263(2023).
Acknowledgements
We received a research grant from the Indian Council of Medical Research (ICMR), Department of Health Research, Government of India for the conduct of this study. P.J. is supported by the DBT-Wellcome Trust Indian Alliance Senior Clinical and Public Health Fellowship (IA/CPHS/20/1/505229). The National Heart Failure Registry was funded by the Indian Council of Medical Research (50/1(9)/TF-CVD/17-NCD-II).
Author information
Authors and Affiliations
Contributions
H.S., A.B., A.R., A.M., J.P., C.M., R.S., S.G., S.S., R.D., M.S., S.G1, and P.J. (Design and protocol development). H.S., A.B., A.R., A.M., J.P., C.M., R.S., S.G., S.S., S.G1, and P.J. (Funding Acquisition). P.J., H.S., and S.G1 (Statistical analysis). P.J. (First draft of the paper). H.S., A.B., A.R., A.M., J.P., C.M., R.S., S.G., S.S., R.D., M.S., S.G1, and P.J. (Reviewed and approved the final manuscript). S.G1 is Sanjay Ganapathy.
Corresponding author
Ethics declarations
Competing interests
P.J. is supported by a Wellcome Trust/DBT India Alliance Clinical and Public Health Senior Fellowship (IA/CPHS/20/1/505229). P.J. received research funding from the National Health and Medical Research Council—Australia (1160283 and 1169766), the Medical Research Council—UK (MR/T037822/1), the National Institute for Health and Care Research (NIHR 204871 and 201815), and the Indian Council of Medical Research.
Peer review
Peer review information
Nature Communications thanks Vijay Chopra, Maarten Leening, Anita Saxena and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Harikrishnan, S., Bahl, A., Roy, A. et al. One-year mortality and re-admission rate by disease etiology in National Heart Failure Registry of India. Nat Commun 16, 275 (2025). https://doi.org/10.1038/s41467-024-55362-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-55362-z