Abstract
The presence of lymph node (LN) metastases guides cancer staging and worsens prognoses. Incomplete lymphadenectomy of metastatic LNs may end up with disease recurrence, while excessive resection can result in increased postoperative complications with even no survival benefit. Thus, effective non-invasive methods to treat metastatic LNs would be highly desirable. Here, we develop an enzyme-responsive formulation of small-sized doxorubicin-loaded mesoporous silica nanoparticles (DMSN, 40 nm) encapsulated in nanoliposomes (DMSN@Pla-Lipo, 160 nm). The liposomal membrane contains 1,2-dipalmitoyl-sn-glycero-3-phospho-rac-(1-glycerol) (DPPG) and 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC), two phospholipids sensitive to secreted phospholipase A2 in human colorectal tumors. In an orthotopic colorectal murine tumor model, phospholipase-induced membrane permeabilization triggers the liberation of DMSN from liposomes for enhanced tumor penetration, conferring an enhanced suppression for the primary tumor. Furthermore, through translocation into metastatic LNs via tumor lymphatics, metastatic tumor cells in LNs are eradicated. Metastases to other major organs are also suppressed, which can be ascribed to the inhibition of colorectal cancer metastasis-associated TGF-β, Wnt, and Hippo signaling pathways in metastatic LNs. The treatment confers an 80% 90-day survival rate in this aggressive tumor model. Taken together, this study demonstrates a deliberate treatment approach for management of both primary tumors and metastatic LNs through multistage drug delivery.
Similar content being viewed by others
Introduction
Cancer progression usually proceeds with lymph node (LN) metastasis, which leads to a poor prognosis1,2. Surgical resection is the dominant method for simultaneously removing primary tumor and metastatic LNs in cancer clinic. However, due to the lack of reliable method for lymphatic imaging and metastasis identification3,4,5, precise removal of metastatic LNs remains a big challenge. Incomplete lymphadenectomy of metastatic LNs may end up with disease recurrence, and excessive resection can damage lymphatic structures around tumor sites to a greater extent, leading to a malfunction of immune system6,7 and an increased risk of postoperative complications8,9, such as lymph cysts, lymphedema and infection, with even no survival benefits in some clinical settings3,8,10. There is an urgent need for generating new methods to deal with both primary cancer and metastatic LNs.
Nanoparticulate drug delivery systems (nano-DDSs) can specifically deliver therapeutics to primary tumor sites via the enhanced permeation and retention (EPR) effect11. This rationale has led to the clinical translations of several nanomedicines, including Doxil, a liposomal doxorubicin formulation that was the first cancer nanomedicine approved by the United States Food and Drug Administration12,13. However, the distribution of these nano-DDSs in metastatic LNs is usually poor14. Currently, most of the preclinical reports on metastatic LN targeted drug delivery is achieved by locally injecting nanoparticles in intradermal15 or subcutaneous16,17,18 tumor model, typically a xenograft model in the mouse footpad, which is an administration route that lacks clinical relevance in most cases. In general, there have been few efforts to effectively deliver drugs to metastatic LNs through systemic injection19,20. Recently, sub-50 nm nanoparticles were found to deliver cargos to LN metastases via extravasating from the blood vasculature in LN metastases after systemic administration14. One investigation from our lab further showed that the tumor cell-targeted, sub-50 nm nanoparticles accumulated more in LN metastases than the non-targeted counterparts5.
One strategy to improve drug delivery is via design of advanced DDSs that become smaller within the tumor microenvironment. Stimulus-sensitive “multistage” nanoparticles have been designed for this purpose21,22,23. A recent report showed that by tumor acidity- triggered size shrinkage from 100 nm to 5 nm and enhanced primary tumor penetration, nanoparticle draining into metastatic LNs via tumor lymphatics can thus be achieved24. While metastasis inhibition was obtained using this method, the therapeutic effect on primary tumor was not reported. It is worth noting that too small nanoparticles (< 20 nm) would be quickly cleared from primary tumors with overall low tumor retention and restricted therapeutic outcome25. In another report, small micelles (25 nm) were used to deliver drugs to metastatic LNs; meanwhile, copper-catalyzed azide-alkyne cycloaddition (CuAAC) between the micelles led to particle aggregation (100 nm) for increased accumulation in primary tumors26. Yet, intratumor injection of the catalytic agent copper (I) is an invasive operation with limited application.
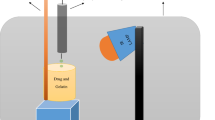
Here, we develop an enzyme-responsive nanosystem for the simultaneous treatment of primary site and metastatic LNs in an orthotopic colorectal tumor model (Fig. 1). Doxorubicin (DOX)-loaded small-sized mesoporous silica nanoparticles (DMSN, ~ 40 nm) are fabricated and then encapsulated in the liposomal aqueous cavity through thin-film hydration method, resulting in DMSN@Pla-Lipo (160 nm). The liposome membrane components contain 1,2-dipalmitoyl-sn-glycero-3-phospho-rac-(1-glycerol) (DPPG)27 and 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC)28, which are representative lipids sensitive to secreted phospholipase A2 (sPLA2), an overexpressed enzyme in various cancers including colon, breast, lung, ovarian, and prostate cancers29,30,31,32. sPLA2 can hydrolyze the ester linkage of glycerophospholipids in DPPG and DPPC, a property used to trigger the cargo release from the liposomes27,33. DMSN@Pla-Lipo is expected to accumulate in primary tumors (orthotopic COLO205 colorectal tumor in this study) via EPR effect after systemic injection. Then, phospholipase in tumor tissue hydrolyzes the lipid membrane, leading to the liberation of the encapsulated DMSN. With smaller particle size, DMSN can penetrate the primary tumor site to suppress tumor growth. Meanwhile, a portion of the particles further penetrate and drain into metastatic LNs via tumor lymphatics to eradicate the LN metastasis. This study demonstrates a paradigm for management of both primary cancer and metastatic LNs through multistage drug delivery.
1 DMSN@Pla-Lipo (160 nm) accumulates in primary COLO205 colorectal tumors via enhanced permeation and retention (EPR) effect after systemic injection. 2 Phospholipases (sPLA2) in tumors disrupt liposomal membranes and liberate small-sized DMSN (40 nm), which can penetrate tumor tissues and drain into metastatic LNs via tumor lymphatics for enhanced suppression of both primary tumors and metastatic LNs.
Results
Preparation and characterization of DMSN@Pla-Lipo
We retrospectively analyzed 230 colorectal cancer patients who underwent radical surgery in Tongren Hospital (SJTU-SM, China) (Table S1). Compared with the patients without LN metastasis, patients with one or more metastatic LNs had much shorter disease-free survival (DFS), even radical surgery was performed (Fig. 2A). This observation was consistent with previous reports34,35. A main cause for disease recurrence and progression would be the incomplete lymphadenectomy of metastatic LNs, partially due to the lack of reliable technique for lymphatic imaging3,4,5. It is an unmet clinical need to effectively suppress LN metastasis while dealing with primary diseases.
A Disease-free survival curve of colorectal cancer patients with or without metastatic LNs. All the 230 patients were treated with radical surgery. Statistical significance was determined using log-rank (Mantel-Cox) test. B Representative immunohistochemical staining of sPLA2 in tumors and adjacent normal tissues from colorectal cancer patients. The test was performed in eleven patients’ samples with similar results. Bar, 50 μm. C Representative TEM images of DMSN and DMSN@Pla-Lipo. The red arrowheads indicate the liposomal membrane. The test was repeated three times with the same results. Bar, 25 nm. D Particle size and zeta potential of the particles (n = 3 independent experiments). Data are presented as mean ± s.d. E Vis-NIR absorbance spectrum of DMSN@Pla-Lipo, in which DOX conferred an absorbance peak at 480 nm, MSN was labeled with iFluor 647 (absorbance peak at 660 nm), and liposomal bilayer was labeled with DiR (absorbance peak at 755 nm). The inset showed the fluorescent images of DOX, iFluor 647, and DiR from the dual-fluorophore-labeled DMSN@Pla-Lipo in a 96-well plate under an IVIS spectrum imaging instrument. F Schematic illustration of the FRET signal in the dual-fluorophore-labeled MSN@Pla-Lipo (iFluor 647, DiR). G Excitation at 650 nm led to a FRET emission at 770 nm for MSN@Pla-Lipo (iFluor 647, DiR). H Super resolution imaging of MSN@Pla-Lipo, in which MSN and lipid bilayer were labeled with iFluor 647 and DiO, respectively. The test was repeated three times with similar results and the representative micrographs were shown. Bar, 1 μm. I Pearson coefficient of correlation (0.8929) indicated the good co-localization of the two fluorophores in panel H. J Nano-flow cytometry assay of the two fluorophore-labeled MSN@Pla-Lipo (iFluor 647, DiO).
Through immunohistochemical assay of the tumor tissues from 11 colorectal cancer patients, we also identified that sPLA2 IIa expression in colorectal tumor tissues was significantly (6.9-fold) higher than that in adjacent normal tissues (Fig. 2B, S1). Information from the Human Protein Atlas demonstrates that RNA expression of sPLA2 IIa encoded by PLA2G2A in human colon and rectal cancer tissues are higher than those in healthy tissues (Fig. S2), confirming the clinical relevance of this enzyme, which may be used as an endogenous stimulus for targeted drug delivery27. Significantly higher sPLA2 IIa expression is also confirmed in COLO205 tumors in contrast to mouse healthy tissues in the assays of western blot (Fig. S3) and activity concentration (Fig. S4). We then developed a sPLA2-responsive nanosystem (DMSN@Pla-Lipo) that can potentially suppress both colorectal primary tumors and LN metastases. DMSN@Pla-Lipo was fabricated by encapsulating small-sized DOX-loaded MSN (DMSN, DOX loading of 8.9%) into the aqueous cavity of sPLA2-sensitive liposomes through thin-film hydration. MSNs were chosen as the model nanocarrier for the proof of concept of this study, as they have been widely used in drug delivery due to their characteristics such as controlled and uniform size, high drug loading efficiency, versatile surface functionality, and good biocompatibility36. It is generally believed that van der Waals forces and hydrogen bonding interactions between drug molecules and silanols of MSN drive the loading of DOX37. Significant progresses have also been made in the clinical translation of silica nanoparticles38,39, confirming their safety and effectiveness as drug delivery carriers in clinical scenarios.
The lipid membrane of DMSN@Pla-Lipo was visible under a transmission electron microscope (TEM) and Cryo-TEM, and there were 2 ~ 3 MSNs encapsulated in the liposomal inner cavity (Fig. 2C, S5). Compared to the smaller size of DMSN (43.4 nm), DMSN@Pla-Lipo was bigger (157.1 nm) (Fig. 2D). The zeta potential of DMSN@Pla-Lipo (-36.5 mV) was higher than that (-24.3 mV) of DMSN (Fig. 2D). The negative charge of the liposomes can be ascribed to the constituted negative-charged DPPG. To characterize the structure of DMSN@Pla-Lipo, MSN was labeled with iFluor 647 and the lipid bilayer was labeled with DiR. DMSN@Pla-Lipo with the dual-fluorophore labeling exhibited three absorbance peaks at 480 nm, 660 nm, and 755 nm in vis-NIR spectrum, corresponding to DOX, iFluor 647, and DiR, respectively (Fig. 2E). A Forster resonance energy transfer (FRET) emission at 770 nm appeared when the liposomes were excited at 650 nm, a wavelength that excited iFluor 647 but not DiR (Fig. 2F, G). In contrast, no FRET emerged in the mixture of Pla-Lipo (DiR) and MSN (iFluor 647). These observations confirmed the structure of DMSN@Pla-Lipo, which afforded a close distance between the two fluorophores. In another test, MSN was labeled with iFluor 647 and the lipid bilayer was labeled with DiO. The resulting dual-fluorophore labeled MSN@Pla-Lipo was observed under a DeltaVision OMX microscope with the capacity of super resolution imaging. The accurate co-localization (yellow) of the signals of iFluor 647 (red) and DiO (green) with 0.89 Pearson’s coefficient of correlation indicated the close distance of MSN and lipid membrane (Fig. 2H, I). Further, nano-flow cytometry assay demonstrated that ~ 97% of the nanoparticles were iFluor 647 and DiO dual-positive, confirming the purity and structure integrity of MSN@Pla-Lipo (Fig. 2J, S6, S7). DMSN@Pla-Lipo had good colloidal stability in PBS with 10% FBS at 37 °C for at least 36 h (Fig. S8), indicating good stability in serum environment.
Examination of DMSN@Pla-Lipo responsiveness to sPLA2
DMSN@Pla-Lipo was assessed for the responsiveness to secreted phospholipase A2 (sPLA2), which is over-expressed in various tumors including colorectal cancer32 (Fig. 2B, S1). sPLA2 can catalyze the hydrolysis of sn-2 ester linkage of glycerophospholipid (typically DPPG and DPPC), yielding equimolar amounts of lyso-lipids and free fatty acids27 (Fig. 3A). This effect may disrupt the liposome structure and lead to cargo release from the inner aqueous cavity. We examined the sPLA2 responsiveness of empty Pla-Lipo, which consisted of DPPG and DPPC. After co-incubation with COLO205 cell conditioned medium (CCM) containing sPLA2 with activity concentration of 144.5 nmol/min/mL, few liposomes were found under TEM, confirming the disruption of liposomes by the enzyme (Fig. 3B). sPLA2-responsive membrane permeation and drug release was assayed using sulforhodamine B (SRB) as the model cargo. SRB with self-quenching concentration (50 mM) was loaded in the liposomal aqueous cavity, resulting in SRB@Pla-Lipo. Disruption of the lipid bilayer leads to fluorescence recovery caused by SRB release and unquenching40,41. After incubation with venom sPLA2 or the enzyme-contained COLO205 CCM, 11.3-fold stronger SRB fluorescence (Ex 490 nm, Em 590 nm) from SRB@Pla-Lipo was detected (Fig. 3C, D). In contrast, no SRB fluorescence was observed for SRB@Pla-Lipo in HT-29 CCM with almost none sPLA2 (activity concentration of 0.9 nmol/min/mL) and enzyme-insensitive SRB@Lipo in COLO205 CCM. The released SRB can be separated from the liposomes through ultracentrifugation (Fig. 3E, F). At different time points, released SRB in the filtrate was detected through fluorescence detection. After 45 min incubation, 90% SRB was released from SRB@Pla-Lipo incubated with sPLA2 or COLO205 CCM (Fig. 3G). In contrast, almost none was released from SRB@Pla-Lipo in HT-29 CCM and SRB@Lipo in COLO205 CCM. These observations were consistent with the above SRB fluorescence unquenching assay.
A Schematic illustration of sPLA2-mediated phospholipid (DPPG as an example) hydration and liposome disruption. B Representative TEM images of Pla-Lipo before and after incubation in sPLA2-contained COLO205 CCM (conditioned culture medium) at 37 °C for 1 h. The sPLA2 activity concentration was 144.5 nmol/min/mL. The test was repeated three times with same results. Bar, 200 μm. C Fluorescence recovery (Ex 490 nm, Em 590 nm) indicated sPLA2-induced SRB leakage from SRB@Pla-Lipo. Bee venom sPLA2 was used in this test. D Fluorescence recovery of SRB-loaded various liposomes after different treatments for 15 min was visualized in an Xenogen IVIS spectrum imaging instrument. E Schematic illustration of the ultrafiltration process for the detection of released SRB. F Photos of the retentate (R) and filtrate (F) in Eppendorf tubes after the liposomes were treated with bee venom sPLA2 or CCM for 15, 30 and 45 min, respectively. G Quantified SRB release in panel F (n = 4 independent experiments). H, J Dynamic light scattering and I, K nanoparticle tracking analysis of the liposomes after incubation in COLO205 CCM for 1 h. L DOX release from DMSN@Pla-Lipo in different media (n = 3 independent experiments). Data in G, L are presented as mean ± s.d. P-values were calculated by one-way ANOVA with Tukey’s multiple comparisons test G, L.
SRB release in the homogenates of mouse normal tissues (heart, liver, spleen, lung, kidney) and COLO205 tumors was also identified (Fig. S9). SRB release from SRB@Pla-Lipo was low (below 20%) after 30 min, 1 h, and 2 h incubation in the homogenates of mouse normal tissues, indicating speculative low contents of sPLA2 in mouse normal tissues like that situation in human, cannot cleave the membrane of SRB@Pla-Lipo. Same observations were obtained for SRB@Lipo. SRB release from SRB@Pla-Lipo in sPLA2-contained homogenate of COLO205 tumors was much faster with release rates of 65.7% at 30 min, and ~ 90% at 1 h and 2 h. However, SRB release from SRB@Lipo in the homogenate of tumor tissues was low, like the levels observed in the homogenate of mouse normal tissues. Further, SRB@Pla-Lipo was incubated in PBS containing mouse sPLA2 IIa with activity concentrations corresponding to those in mouse heart, liver, spleen, lung, kidney, colon, and human COLO205 tumors (Fig. S4) for 2 h. SRB release from SRB@Pla-Lipo was low (below 20%) when activity concentrations of mouse sPLA2 was low in the healthy tissues, but much higher (> 90%) in the condition like the level in COLO205 tumors, demonstrating high mouse sPLA2 content, but not low contents like those in healthy mouse tissues can efficiently cleave the membrane of SRB@Pla-Lipo (Fig. S10).
sPLA2-responsive release of small-molecule cargo has led to the development of liposomal cisplatin (LiPlaCis), which is now in phase III trial42. Nevertheless, whether small particles encapsulated in the liposomes can be liberated upon sPLA2 stimulus remains to be determined. The escape of small particles (DMSN) from the liposomal aqueous cavity was identified using both dynamic light scattering (DLS) and Nanoparticle Tracking Analysis (NTA) technology.
After 1 h incubation of DMSN@Pla-Lipo in COLO205 CCM, a small-sized particle population with comparable dimension to that of free DMSN appeared in the assays of both DLS and NTA (Fig. 3H, I), indicating the disruption of liposome integrity and liberation of the encapsulated DMSN. Furthermore, in NTA assay, the small-sized particles had average zeta potential (~ -20 mV) comparable to that of free DMSN, furtherly confirming the escape of DMSN from Pla-Lipo aqueous cavity. As a control, the size of DMSN@Lipo remained unchanged after incubation in COLO205 CM (Fig. 3J, K). These observations proved the role of sPLA2 in liberating small particles from the aqueous cavity of sPLA2-responsive liposomes.
This sensitivity to sPLA2 also influenced DOX release profile (Fig. 3L). DMSN@Pla-Lipo restrained DOX release (~10%) in pH 7.4 PBS, pH 5.5 PBS (mimicking lysosomal environment), and 10% FBS at 37 °C for at least 24 h. This property can help hinder DOX leakage in circulation before they navigate to tumor sites. Furthermore, such slow release may also decrease the toxicity to major organs (liver, heart, lung, kidney and spleen) with low or none expression of the enzyme, even when the liposomes are trapped there. DMSN@Pla-Lipo exposed to sPLA2 and entering the cells as DMSN (simulated by the release condition pH 5.5 + sPLA2) released 75.3%. DMSN@Pla-Lipo exposed to sPLA2 but not the acidic pH (pH 7.4 + sPLA2) released 37.4%, indicating that at least half of the loaded drug may be released intracellularly. In acid lysosomes (pH 5.5), DOX as a weakly basic drug (pKa = 8.15) is susceptible to be protonated43, which attenuates its adsorption to the silanols of MSN via hydrogen bonding and thus facilitates release. Rapid drug release in disease site usually benefits the therapeutic outcome. In contrast, DOX release from non-responsive DMSN@Lipo was not changed in the different media (Fig. S11).
Cellular uptake, cytotoxicity, and tumor spheroid penetration of DMSN@Pla-Lipo
DMSN escape (from the liposomes)-induced size shrinkage would be favorable for cellular uptake and toxic killing in tumor cells. For the test of cellular uptake, MSN was labeled with iFluor 647. Compared to MSN@Lipo, increased iFluor 647 fluorescence was observed in the cells incubated with MSN@Pla-Lipo for 3 h (Fig. 4A). Flow cytometry assay confirmed this observation with 10.6 fold difference in cell-associated fluorescence intensity (Fig. 4B). Of note, there was no difference between the cellular uptake of free MSN and MSN@Pla-Lipo. Size shrinkage caused by sPLA2 may be responsible for this improved uptake, which would eventually confer an enhanced toxicity to cancer cells.
A CLSM images of COLO205 cells after 3 h incubation with MSN, MSN@Lipo, or MSN@Pla-Lipo. The cell membrane was stained with DiO (green), and MSN was labeled with iFluor 647 (red). Bar, 10 μm. B Quantified cell-associated iFluor 647 fluorescence intensity after cellular uptake in panel A using flow cytometry (n = 3 independent experiments). C Cell viabilities after treatment with DMSN, DMSN@Lipo, or DMSN@Pla-Lipo for 24 h were examined using CCK-8 assay (n = 5 independent experiments). D The cells after the indicated treatments (DOX, 1 μg/mL) for 24 h were stained with calcein-AM and propidium iodide (PI) for simultaneous fluorescence imaging of viable and dead cells. Bar, 50 μm. E Penetration of iFluor 647-labled MSN, MSN@Lipo, or MSN@Pla-Lipo in COLO205 tumor spheroids (iFluor 647, 800 ng/mL). The area marked with blue circles were considered the inside area. Bar, 100 μm. F Quantified fluorescence intensity at the 250 μm cross-section in panel E (n = 3 independent experiments). G Cytotoxicity of the various formulations in COLO205 tumor spheroids, which were stained with calcein-AM and PI. Representative micrographs were shown, and the tests were repeated three times. Bar, 100 μm. H Flow cytometry assay of apoptotic tumor cells in panel G. I Statistical assay of cell apoptosis rate in panel H. Cell apoptosis rate refers to the ratio of annexin V-positive cells to the total analyzed cells (n = 3 independent experiments). Data in B, C, F, I are presented as mean ± s.d. P-values were calculated by one-way ANOVA with Tukey’s multiple comparisons test B, C, F, I.
Concentration-dependent cytotoxicity to COLO205 cells was examined after 24 h incubation. Relative to DMSN@Lipo, DMSN@Pla-Lipo resulted in enhanced cytotoxicity at all tested DOX concentrations, and this effect was comparable to that of free DMSN (Fig. 4C). The empty MSN, MSN@Lipo, MSN@Pla-Lipo, which contained no drugs, were non-toxic to COLO205 cells (Fig. S12), thus excluding the influence of the carrier itself on the cytotoxicity. The cytotoxicity results were consistent with the observation of calcein-AM and propidium iodide (PI) dual staining assay (Fig. 4D).
Size shrinkage can facilitate the penetration of nanocarriers into tumor tissues21. We examined the penetration behavior of MSN@Pla-Lipo in COLO205 tumor spheroid model (Fig. S13). MSN was labeled with iFluor 647 for nanoparticle monitoring. After MSN@Lipo treatment for 36 h, the red fluorescence from iFluor 647 was limited to the periphery of the tumor spheroid. In contrast, MSN@Pla-Lipo distributed more widely and even at each cross-section (50, 100, 150, 200, and 250 µm from the surface) of the tumor spheroid (Fig. 4E). This improved penetration was comparable to that of free MSN. Similar size shift from 150 nm to 40 nm was also found to confer enhanced penetration44. Quantified analysis of the fluorescence intensity at 250 µm cross-section indicated that more than 24.2-fold stronger red fluorescence was detected in MSN@Pla-Lipo-treated tumor spheroids than in MSN@Lipo-treated ones (Fig. 4F). These observations demonstrated that sPLA2-responsitve MSN@Pla-Lipo penetrated better in tumor tissues.
This enhanced tumor penetration would be favorable for the nanosystem to kill more tumor cells located both in the periphery and the interior area of the tumor tissues. After 36 h incubation, more tumor cells died with PI staining (red) in the group of DMSN@Pla-Lipo and DMSN, compared to DMSN@Lipo (Fig. 4G). Apoptosis assay of the tumor spheroids using flow cytometry demonstrated similar results. 73.6% tumor cells in the group of DMSN@Pla-Lipo were in the stage of early and late apoptosis, in contrast to only 24.4% cell apoptosis in the spheroid treated with DMSN@Lipo (Fig. 4H, I). We performed these tests using HT-29 cells, which don’t express sPLA2. There were no differences in cell uptake, cytotoxicity, and tumor spheroid penetration between DMSN@Lipo and DMSN@Pla-Lipo (Fig. S14).
Long circulation and accumulation of the liposomes in orthotopic colorectal tumors and metastatic sentinel LNs
Long circulation in blood is important for the nanosystem to efficiently target to tumor sites. We examined the circulation profile of DOX from DMSN@Pla-Lipo and DMSN@Lipo in female BALB/c nude mice. Compared to a quick clearance of free DOX from the blood, DOX in DMSN@Pla-Lipo or DMSN@Lipo maintained a much higher concentration in blood (Fig. S15). There was no significant difference in the DOX plasma concentrations between the two liposomes at each time point in the systemic circulation. Accordingly, DMSN@Pla-Lipo and DMSN@Lipo possessed comparable pharmacokinetic parameters, including T1/2 (half-life in plasma), AUC (area under the curve), MRT (mean residence time), CI (clearance), and Vz (volume of distribution) (Table S2).
Orthotopic colorectal cancer model is more clinically relevant than commonly used ectopic, subcutaneous ones. We established an orthotopic colorectal cancer model through injecting luciferase and green fluorescent protein (GFP) dual-labeled COLO205-luc-GFP cells into the submucosa of mouse cecum5. Bioluminescence imaging with the sensitivity of the detection of 50 tumor cells (Fig. S16) were used to monitor orthotopic tumor growth and mesenteric sentinel LN (1st LN) metastasis along with the time (Fig. 5A, B, S17A, B, C). On day 21 after tumor cell inoculation, 3 from 5 mice had metastasis in sentinel LNs. On day 28, all the sentinel LNs were positive with bioluminescent metastasis. Meanwhile, no metastasis occurred to the major organs (heart, liver, spleen, lung, and kidney) (Fig. S17D). Therefore, the mice with tumor cell inoculation for 28 days were used in this study. Orthotopic tumor and sentinel LN metastasis were also confirmed by pathological assay and immunohistochemical staining. The pathological section demonstrated the anatomical ___location of the orthotopic tumor inside the cecum submucosa (Fig. 5C) and the detectable solitary metastasis lesion in the sentinel LN (Fig. 5G). We also investigated the sPLA2 expression of the orthotopic COLO205 colorectal tumor and the metastatic LN through immunohistochemical assay. An antibody (ab23705, Abcam) that can recognize sPLA2 from both human and mouse was used45. The sPLA2 expressions in tumor tissues and metastatic LNs were significantly higher compared to those in adjacent normal tissues (Fig. S18) and healthy LNs (Fig. S19).
A Illustration of the primary tumor, the metastatic sentinel LN (1st LN), and the 2nd LN in the mesentery. B Photo and bioluminescence imaging of orthotopic tumor and the 1st LN. C H&E staining of representative orthotopic tumor on day 28 after tumor cell inoculation. The test was repeated three times with similar results. D Fluorescence imaging of time-dependent accumulation of iFluor 647-labeled MSN@Lipo or MSN@Pla-Lipo in primary tumors (iFluor 647, 0.2 mg/kg). E Quantified iFluor 647 fluorescence signals in panel D (n = 3 mice). F Time-dependent DOX contents in primary tumors after i.v. injection of DMSN@ Pla-Lipo (DOX, 7 mg/kg) (n = 3 mice). G Representative Immunohistochemical staining of the 1st LN on day 28 after tumor cell inoculation. The tumor cells were stained with anti-luciferase antibody. The metastasis area was outlined with a red line. The test was repeated three times with similar results. H Fluorescence imaging of time-dependent accumulation of iFluor 647-labeled MSN@Lipo or MSN@Pla-Lipo in the 1st LN (iFluor 647, 0.2 mg/kg). I Quantified iFluor 647 fluorescence signals in panel H (n = 3 mice). J Time-dependent DOX contents in the 1st LN after i.v. injection of DMSN@Pla-Lipo (DOX, 7 mg/kg) (n = 3 mice). K Fluorescence imaging of iFluor 647-labeled MSN@Pla-Lipo in the 2nd LN in the mesentery (iFluor 647, 0.2 mg/kg). The 2nd LNs with or without metastases were displayed, separately. L Quantified iFluor 647 fluorescence signals in panel K (n = 5 mice). Data in E, F, I, J, L are presented as mean ± s.d. Statistical significance was determined using a two-tailed unpaired t test E, F, I, J, L.
MSN was labeled with iFluor 647 for the observation of liposome (MSN@Pla-Lipo and MSN@Lipo) accumulation in primary tumor and metastatic sentinel LNs (1st LN). At pre-determined time points (1, 2, 4, 8, 12, and 24 h) after i.v. injection of the liposomes, primary COLO205 tumors (Fig. 5D, E) and metastatic sentinel LNs (Fig. 5H, I) were excised for ex vivo imaging. MSN@Pla-Lipo and MSN@Lipo showed comparable accumulation at the primary tumor site except that at 8 h post-injection, tumors treated with MSN@Pla-Lipo had lower fluorescence intensity. In contrast, iFluor 647-labeled MSN@Pla-Lipo accumulated more in metastatic sentinel LNs than MSN@Lipo. The improved accumulation of MSN@Pla-Lipo in LNs may be ascribed to the sPLA2-mediated MSN escape from the liposomal aqueous cavity and follow-up enhanced draining to LNs. Meanwhile, the biodistribution of iFlour 647 labeled MSN@Pla-Lipo and MSN@Lipo nanosystems at 8 h after injection was examined. There was no significant difference in their distribution in major organs between the two liposomes (Fig. S20). In a separate study, the contents of the liposomal cargo (DOX) in both primary tumor (Fig. 5F) and sentinel LNs (Fig. 5J) were examined after i.v. injection of DMSN@Pla-Lipo or DMSN@Lipo (DOX, 7 mg/kg). Overall, the accumulation pattern of DOX in the primary tumor and metastatic sentinel LNs with the time was similar to that of iFluor 647-labeled liposomes at the two sites. Less DOX from DMSN@Pla-Lipo was found in the primary tumor at 8 h and 12 h compared to that from DMSN@Lipo. In contrast, much more DOX from DMSN@Pla-Lipo was observed in the metastatic sentinel LNs compared to that from DMSN@Lipo. This improved distribution in metastatic sentinel LNs would contribute an enhanced cytotoxicity to the tumor cells in the metastasis.
The DOX accumulation in the primary tumor and the 1st LN was also compared between DOX@Pla-Lipo and DMSN@Pla-Lipo. Compared to DOX@Pla-Lipo, DMSN@Pla-Lipo conferred more DOX accumulation in the tumor and the 1st LN (Fig. S21). Improved distribution in the tumor site may be ascribed to less cargo leakage in blood circulation due to MSN restriction46,47. It has been demonstrated that conventional nanocarrier-mediated drug delivery, such as Doxil (~ 80 nm), led to limited drug accumulation in metastatic LNs14. As for free drugs, many of them including DOX cannot penetrate efficiently in solid tumor, due to several barriers including the composition and structure of the tumor extracellular matrix, drug binding and metabolism, etc48. Specifically, the poor penetration of DOX in tumor tissue is due to the avid binding to cellular DNA and sequestration in acidic endosomes of cancer cells that are proximal to the tumor vasculature48. Thus, the access of free drugs, after they are delivered to the primary tumor site, to tumor associated lymphatic vessels and metastatic LNs will be commonly restricted. The significantly enhanced penetration of DMSN@Pla-Lipo in tumors compared to free DOX-loaded liposomes (DOX@Pla-Lipo) was confirmed in the COLO205 tumor spheroid model (Fig. S22). We further designed a study to examine intracellular sequestration of DOX in COLO205 cells (Fig. S23A). Much lower fluorescence in the cell medium of DOX@Pla-Lipo group indicated more sequestration of DOX from DOX@Pla-Lipo, but not DMSN@Pla-Lipo, in tumor cells (Fig. S23B, C), conferring the advantage of DMSN@Pla-Lipo over DOX@Pla-Lipo in tumor penetration.
Further, bioluminescence imaging indicated that 2 from 5 mice had metastases in the 2nd LN of the mesentery on day 28 after tumor cell inoculation (Fig. S24). Accumulation of iFluor 647-labeled MSN@Pla-Lipo in the 2nd LN with or without the metastases was characterized. It was demonstrated that 3.9-fold more accumulation reflected from the iFluor 647 fluorescence intensity was obtained in the LNs with metastases compared to the healthy ones (Fig. 5K, L, S25). This property would confer more drug accumulation in the metastatic LNs for more efficient tumor cell killing. The superior accumulation of particles in metastatic LNs over the healthy ones may be related with the increased lymph flow caused by tumor-induced lymphangiogenesis in LNs49,50, which needs to be investigated further.
MSN translocated from orthotopic colorectal tumor to metastatic sentinel LNs via lymphatic vessels
PAMAM nanoparticles (~ 5 nm) can translocate to sentinel LNs via the intratumoral lymphatic vessels24. It is expected that this was also the route for the small-sized MSN to enter and accumulate in the metastatic sentinel LNs. To observe the transportation via the lymphatic vessels, MSN was labeled with iFluor 647 (red) and the lymphatic vessels in primary tumors were stained with anti-mouse LYVE1 (green). In the primary COLO205 tumor at 4 h post-injection, considerable MSN from MSN@Pla-Lipo appeared inside the lymphatic vessels. However, markedly less red fluorescence of MSN in the lymphatic vessels was observed in the group of MSN@Lipo (Fig. 6A). Quantitative analysis demonstrated that MSN signal of MSN@Pla-Lipo in lymphatic vessels was approximately 5.2-fold higher than that of MSN@Lipo (Fig. 6B).
A 4 h after i.v. injection of the liposomes, in which MSN (red) was labeled with iFluor 647 (0.2 mg/kg), primary tumors were processed for frozen section and immunofluorescence staining of lymphatic vessels (LYVE1, Alexa Fluor 488, green). Representative images were shown. Scale bar, 200 μm. B Quantitative analysis of the fluorescence intensity of MSN inside tumor lymphatic vessels in panel A (n = 3 mice). C Representative microdistribution of iFluor 647-labeled MSN (red) in metastatic sentinel LNs (left) at 8 h after i.v. injection of MSN@Pla-Lipo in the presence (middle) or the absence (bottom) of primary tumor. For the group without primary tumor, the tumor-bearing mice were subjected to primary tumor resection before the i.v. injection of MSN@Pla-Lipo. MSN@Lipo with the presence of primary tumor was included as a control (top). The LNs were processed for frozen section and immunofluorescence staining of blood vessels (CD31, Cy3, cyan) and lymphatic vessels (LYVE1, Alexa Fluor 488, green). Scale bar, 200 μm (left) and 50 μm (enlarged view in the middle). The images of MSN, lymphatic vessels, blood vessels, and MSN inside lymphatic vessels were shown in the right, respectively. D Quantitative analysis of the fluorescence intensity of MSN inside lymphatic vessels of metastatic LNs in panel C (n = 3 mice). E Representative tissue classification of blood vessels (red) and lymphatic vessels (green) in metastatic LNs (left) was performed using HALO software. The corresponding heat map of MSN signal intensity (right) was presented independently. Bar, 200 μm. F Quantified MSN fluorescence intensity inside lymphatic vessels in panel E using HALO software (n = 3 mice). Data in B, D, and F are presented as mean ± s.d. P-values were determined using a two-tailed unpaired t test B and one-way ANOVA with Tukey’s multiple comparisons test D, F.
From the comparable bioluminescence signal of the metastatic sentinel LNs (Fig. S26), there would be no significant difference in the metastatic tumor size or tumor cell density across three lymph nodes representing each group. In the metastatic sentinel LNs, compared to MSN@Lipo group, more MSN (red) from MSN@Pla-Lipo were found inside the lymphatic vessels (green), but not the blood vessels (cyan), confirming the superior lymphatic route for MSN translocation (Fig. 6C). However, after resection of the primary tumor, this lymphatic transportation pathway was dramatically blocked. This test confirmed the role of primary tumors as a transit station for the translocation to sentinel LN. Quantified fluorescence assay indicated that MSN signal of MSN@Pla-Lipo in lymphatic vessels of LNs was approximately 4.3-fold higher than that of MSN@Lipo, and this advantage disappeared if the primary tumor was previously resected before the liposome injection (Fig. 6D).
Further, the whole LN frozen sections with immunofluorescence staining were scanned and analyzed using HALO image analysis (Indica Labs)51. Blood vessels (red) and lymphatic vessels (green) in the LNs was outlined using the HALO tissue classifier analysis module and MSN signals was displayed as a heat map (Fig. 6E). Compared to MSN@Lipo, MSN@Pla-Lipo treatment conferred more MSN signals in LNs. Moreover, better co-localization of MSN from MSN@Pla-Lipo and lymphatic vessels can be seen from the images of tissue classification and MSN heat map and the quantified assay (Fig. 6F). However, this enhanced LN accumulation of MSN and co-localization with lymphatic vessels dramatically declined if the primary tumor was resected before the liposome injection. These results demonstrated that sPLA2-responsive MSN@Pla-Lipo, but not MSN@Lipo, entered the metastatic LNs through the tumor drainage lymphatic vessels.
Antitumor effects of DMSN@Pla-Lipo in orthotopic colorectal tumor-bearing mice
We next investigated the anticancer effects of DMSN@Pla-Lipo in the orthotopic COLO205-luc-GFP colorectal tumor model. The evaluation program was illustrated in Fig. 7A. 28 days after orthotopic tumor implantation, mice were divided into six groups according to the bioluminescence intensity. The COLO205-luc-GFP tumor bearing mice were i.v. injected with 1) free DOX, 2) DMSN@Lipo or 3) DMSN@Pla-Lipo (7 mg/kg DOX) with two repetitions (days 0 and 4). The groups of 4) saline, 5) MSN@Lipo (empty) and 6) MSN@Pla-Lipo (empty) were included as controls. Bioluminescence imaging of the mice was performed every week on days 7, 14, 21, 28, 35, 42, and 49, respectively (Fig. 7B). Comparing to rapid tumor growth and early mouse death in the saline group, treatment with DMSN@Lipo and DMSN@Pla-Lipo delayed tumor growth and extended animal survival. The strongest antitumor efficacy was achieved in DMSN@Pla-Lipo with almost complete suppression of tumor growth during the 49-day bioluminescence imaging observation (Fig. 7C, D). As the differences in iFluor 647-labeled MSN and DOX biodistribution in the primary tumor between DMSN@Pla-Lipo and DMSN@Lipo were moderate except two time points at 8 h and 12 h (Fig. 5D–F), the enhanced suppression of the primary tumor by DMSN@Pla-Lipo may be ascribed to the improved DOX release responsive to sPLA2 in tumor sites, increased cellular uptake and cytotoxicity, and enhanced tumor penetration compared to DMSN@Lipo (Fig. 3L, Fig. 4, Fig. S11). The therapeutic efficacy of DOX@Pla-Lipo in tumor-bearing mice was also investigated. DOX@Pla-Lipo cannot effectively inhibit the growth of tumor and extend the survival (Fig. S27). Empty vehicles (MSN@Lipo and MSN@Pla-Lipo) was ineffective in suppressing the tumor growth, and all mice died within 35 days. Slight survival improvement was observed for the groups of free DOX and DMSN@Lipo, while all mice eventually died within 49 days. In contrast, 80% of the mice in DMSN@Pla-Lipo survived up to 90 days, exhibiting a significantly antitumor efficacy compared to all other treatments (Fig. 7E). During the therapy till day 28, the mouse body weight from DMSN@Pla-Lipo and other groups well maintained, indicating the tolerance of the treatment (Fig. 7F).
A Treatment regimen and time points for RNA sequencing and metastasis examination. The DOX dose was 7 mg/kg for each injection for the groups of free DOX, DMSN@Lipo, and DMSN@Pla-Lipo. Saline, MSN@Lipo (empty), and MSN@Pla-Lipo (empty) were included as controls. B Bioluminescence imaging of the tumor growth in mice every week till day 49. Dead mice were not imaged. C Bioluminescence intensity over the time of each mouse in the various treatments. D Fold changes of the bioluminescence intensity compared to that on day 0 were shown as a heat map. E Survival curve of the mice with the indicated treatments. Five mice were included in each group. Statistical significance was determined using log-rank (Mantel-Cox) test. F Mouse body weight monitoring till day 28. The n changed in the groups of saline, MSN@Lipo, MSN@Pla-Lipo, and free DOX, as the mice died during this period. n = 5 mice in all groups on Days 0, 7, and 14. On Day 21, n = 4 mice in the groups of saline, and MSN@Pla-Lipo, 3 mice in the group of MSN@Lipo, and 5 mice in the groups of Free DOX, DMSN@Lipo, and DMSN@Pla-Lipo. On Day 28, n = 2 mice in the groups of saline, and MSN@Lipo, 1 mouse in the group of MSN@Pla-Lipo, 3 mice in the group of Free DOX, and 5 mice in the groups of DMSN@Lipo and DMSN@Pla-Lipo. Data are presented as mean ± s.d.
The role of DMSN@Pla-Lipo in suppressing metastases in mesenteric sentinel LNs (1st LN) was examined. In a separate study, when one mouse in the saline group died (day 19), mice with various treatments were sacrificed and the mesenteric sentinel LNs were excised. Ex vivo bioluminescence imaging was performed to identify the metastases (Fig. 8A, S28). Compared to the visible bioluminescence signals in the LNs treated with DMSN@Lipo and other controls, no signal appeared in the LNs of mice treated with DMSN@Pla-Lipo. Flow cytometry was further used to quantify the proportions of the tumor cells in the LNs (Fig. 8A). Compared to 7% ~ 10% proportion of tumor cells resided in the sentinel LNs of mice treated with DMSN@Lipo, free DOX and other controls, almost none tumor cells in the LNs of mice with DMSN@Pla-Lipo treatment can be detected (Fig. 8B). This anti-metastatic effect in sentinel LNs can be partially ascribed to the improved LN accumulation of DMSN liberated from the sPLA2-responsive DMSN@Pla-Lipo. The suppressive effect on primary tumor growth may also confer the inhibition of metastases in LNs, which needs to be explored further.
A Detection of COLO205-luc-GFP cells in the sentinel LNs using bioluminescence imaging and flow cytometry. Representative bioluminescent images of LNs were shown. The tests were repeated with five independent LNs with similar results. B Statistical comparison of the tumor cell proportions in the sentinel LNs (n = 5 mice). Data are expressed as mean ± s.d. P-values were calculated by one-way ANOVA with Tukey’s multiple comparisons test. C When one mice of the saline group died (day 19), ex vivo bioluminescence imaging was performed to examine the micro-metastasis in the main organs (liver, spleen, lung, kidney, and intestine). Five mice were included in each group. D The metastatic frequencies in the organs after various treatments were summarized in a heat map.
The metastasis profile in major organs (liver, spleen, lung, kidney, and intestine) on day 19 were also characterized (Fig. 8C, D). For the saline group, all the mice had extensive metastases in the intestine and liver. One of the mice had spleen metastases, and one mouse also exhibited lung metastases. The mice in the groups of MSN@Pla-Lipo and MSN@Lipo had similar metastasis pattern to that of the saline group. Free DOX and DMSN@Lipo well inhibited the metastases in spleen, lung, and kidney, but there were multiple metastatic foci in liver and intestine. In sharp contrast, metastases in the major organs (liver, spleen, lung, kidney and intestine) were completely inhibited with the treatment of DMSN@Pla-Lipo, which contributed the enhanced antitumor effect on extending the survival of the tumor-bearing mice.
To further investigate the antimetastatic mechanisms of DMSN@Pla-Lipo treatment, we examined the transcriptomic profiles of the treated sentinel LNs (1st LN) on day 5 by RNA sequencing assay. The heat map of the differentially expressed genes (DEGs) demonstrated the significant changes of the transcripts in the LNs after DMSN@Pla-Lipo treatment compared to those treated with DMSN@Lipo (Fig. 9A). Using the filtering criteria (absolute fold change > 2, p value < 0.05) indicating the markedly different RNA expression, 3592 DEGs were identified. Among these DEGs, 2300 genes (such as Smad6, Sfrp2, Ccl12, etc.) presented as blue dots in the volcano plot were downregulated and 1292 genes (such as Ccl19, Lefty1, Ngfr, etc.) indicated with red dots were upregulated (Fig. 9B). Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis indicated that the DEGs between DMSN@Pla-Lipo and DMSN@Lipo were enriched in specific colorectal cancer metastasis-associated signaling pathways, typically TGF-β signaling52, Wnt signaling pathway53, and Hippo signaling pathways54 (Fig. 9C). These pathway enrichments were also confirmed in the gene set enrichment analysis (GSEA) (Fig. 9D–F). The significant down-regulation of the key metastasis-associated pathways in the LNs treated with DMSN@Pla-Lipo would be ascribed to the superior eradication of the metastatic tumor cells in the LNs (Fig. 8A, B). As tumor cells colonized in the LNs are more prone than parental ones to spread to distant organs55, the multistage drug delivery achieved by DMSN@Pla-Lipo in this study presented a promising strategy to efficiently deplete these more aggressive cells in LNs for better therapeutic outcome.
A Heat map of differentially expressed genes (DEGs) in sentinel LNs (1st LN) from the mice after DMSN@Lipo or DMSN@Pla-Lipo treatment. red, upregulation; blue, downregulation. n = 3 mice in each group. B Volcano plot showed the upregulated (red dots) and downregulated (blue dots) mRNA in the metastatic sentinel LNs treated with DMSN@Pla-Lipo compared to those treated with DMSN@Lipo. Genes with an absolute fold change > 2 and a p value < 0.05 were regarded as DEGs. C Both up- and down-regulated genes in the group of DMSN@Pla-Lipo was included for KEGG enrichment assay. Gene set enrichment analysis (GSEA) was performed for TGF-β signaling D, Wnt signaling E, and Hippo signaling pathways F, which were significantly downregulated in the LNs treated with DMSN@Pla-Lipo relative to DMSN@Lipo.
Therapy-associated toxicity was investigated through pathological examination of major organs, serum biochemistry, and complete blood panel assay. Pathological examination of the major organs (heart, liver, spleen, lung, and kidney) on day 5 in all groups showed no histological toxicity (Fig. S29). Key parameters reflecting liver (alanine aminotransferase/ALT, aspartate aminotransferase/AST, and albumin) and kidney (urea and creatinine) function and hematological toxicity (red blood cells, white blood cells, neutrophils, platelets, etc.) were examined using healthy female BALB/c nude mice (Fig. S30). No difference was observed in the parameters of DMSN@Pla-Lipo, when compared to saline and other controls, demonstrating the low toxicity of the therapeutic regimen.
Further, the influence of the LN-drained DOX on T cells was evaluated in an immune-competent footpad model using a mouse tumor cell line (CT-26 cells)24. Western blot assay indicated sPLA2 expression is absent in CT-26 cells (Fig. S31). Accordingly, sPLA2 activity concentration detected in CT-26 tumors was extremely low, even below those in healthy mouse tissues (Fig. S4). Therefore, DMSN@Pla-Lipo pre-incubated with sPLA2 was included to simulate the situation as DMSN@Pla-Lipo influenced by sPLA2-expressing COLO205 tumors. Like DMSN, DMSN@Pla-Lipo pre-incubated with sPLA2 significantly suppressed CT-26 tumor growth and metastasis in sentinel LNs (Fig. S32A–C). The percentages of live T cells in the sentinel LNs remained unchanged, indicating the limited adverse effects of lymph node-drained DOX on T cells. (Fig. S32D, S33). Meanwhile, increased CD8+ T cells and decreased CD4+ T cells were observed in the sentinel LNs, and CD8+/CD4+ T cell ratios were improved (Fig. S32E–G). These observations demonstrated the immune-enhanced effects of DMSN@Pla-Lipo, which may be related with the inhibition of LN metastases.
Discussion
Precision treatment of metastatic LNs has long been a major challenge in cancer clinic. Incomplete lymphadenectomy will end up with disease recurrence, while excessive resection may damage lymphatic structures with a resultant impairment of antitumor immunity and even no survival benefits56. To avoid the limitations of lymphadenectomy, we here developed a multistage drug delivery approach using DMSN@Pla-Lipo as a proof-of-concept example for the treatment of colorectal primary tumor and LN metastases. A series of in vitro and in vivo experiments demonstrated the multistage drug delivery performance of DMSN@Pla-Lipo. The enhanced penetration in primary tumor site and a follow-up improved translocation of DMSN into metastatic LNs via intratumoral lymphatic vessels ensured high drug exposure in the two disease sites. A recent report indicated that larger (50 nm and 100 nm) gold nanoparticles exit the tumor via intratumoral lymphatic vessels, while the middle-sized (30 nm) particles exit the tumor via both intratumoral and peritumoral lymphatic vessels in comparable quantities57. The translocation of DMSN (40 nm) into intratumoral lymphatic vessels and thereafter the metastatic LNs was consistent with the observations in the literature.
LNs are important sites for adaptive immune production. In addition to the chemotherapy exemplified in this work, through manipulating nanoparticle size58, and delicately programmed cargo release15,59, immune drugs would be delivered to dendritic cells and the resident lymphocyte subpopulations in cortex and paracortex regions of metastatic LNs to trigger antitumor immunotherapy.
One limitation for DMSN@Pla-Lipo is that it relies on intratumoral enzyme to exert its function. However, as an endogenous physiological stimulus, sPLA2 is not expressed in all tumor types, and appreciable heterogeneities of physiological signals among and within individuals affects the therapeutic effect and hinder the translation60. One feasible measure is to utilize exogenous stimuli, such as light, ultrasound, electrical and magnetic fields61,62. These stimulation methods with associated devices have been clinically approved, which can then be used to provide stimulation signals of appropriate intensity on demand by a physician or patient to meet the need for undisturbed and efficient multistage drug delivery and therapy.
Taken together, this study demonstrates a paradigm for deliberate and simultaneous targeting of both primary cancer and metastatic LNs via multistage drug delivery, which would be favorable for more efficient treatment of solid tumors with accompanied metastatic LNs.
Methods
This research complies with all relevant ethical regulations and were approved by the Institutional Animal Care and Use Committee (IACUC) of Shanghai Jiao Tong University School of Medicine (SJTU-SM, ethical approval number: A-2018-026). The maximal tumor burden in bioluminescence intensity permitted is 3×1010 photons/s, and this burden was not exceeded in this study. Informed consent was obtained by the colorectal cancer patients who underwent radical surgery and standard of care in Tongren Hospital (SJTU-SM). The gender of the patients was determined based on self-report.
Materials, cell culture, and animals
1,2-dipalmitoyl-sn-glycero-3-phospho-rac-(1-glycerol) sodium salt (DPPG), 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC), hydrogenated soy phosphatidylcholine (HSPC), cholesterol, and 1,2-distearoyl-sn-glycero-3-phospho-ethanolamine-N-[methoxy(polyethylene glycol)]-2000 (DSPE-PEG2000) were purchased from AVT (Shanghai) Pharmaceutical Tech Co., Ltd. Tetraethylorthosilicate (TEOS, 98%), cetrimonium bromide (CTAC, 98%), 1,1′-dioctadecyl-3,3,3′,3′-tetramethylindotricarbo cyanine iodide (DiR), 3,3′- dioctadecyloxacarbocyanine perchlorate (DiO), and sPLA2 from honey bee venom were purchased from Merck (Darmstadt, Germany). Doxorubicin hydrochloride was purchased from Hvsf United Chemical Materials (Beijing, China). RPMI 1640 medium, fetal bovine serum (FBS), penicillin, and streptomycin were obtained from Thermo Fisher Scientific (Shanghai, China). Double distilled water was purified using a Millipore simplicity system (Millipore, Bedford). All other chemicals were of analytical grade and used without further purification.
COLO205 (ATCC, CL-222) and HT29 (ATCC, HTB-38) human colorectal adenocarcinoma cell line was obtained from National Collection of Authenticated Cell Cultures (Shanghai, China). Luciferase and green fluorescent protein (GFP) dual-labeled COLO205 cells (COLO205-luc-GFP, catalog number: SL005) were purchased from GeneCopoeia (Rockville). Luciferase-labeled mouse CT-26 cells (CT-26-luc, catalog number: NM-S24A-1) were purchased from Shanghai Model Organisms Center. Cells were used without modification after receiving from the supplier and therefore were not authenticated. The cell line was tested routinely to be negative for mycoplasma contamination. No commonly misidentified cell lines were used. The cell lines were cultured in RPMI 1640 medium with 10% FBS, 105 U/L penicillin, and 100 mg/L streptomycin. The culture was maintained at 37 °C in a humidified atmosphere containing 5% CO2.
Female BALB/c nude mice (4 ~ 5 week old) were purchased from Shanghai Lingchang Biotechnology (China). The mice were housed pathogen-free and ventilated cages, and allowed free access to food and autoclaved water in a 12 h light/dark cycle, with room temperature at 20 ~ 22 °C and humidity between 45 and 65%. Sex and/or gender was not considered in the study design, as it is not postulated as a contributing factor in this study.
Preparation of DMSN@Pla-Lipo
Small-sized MSN (40 nm) was synthesized according to the procedures we previously described63. For DOX loading, 5 mg DOX was mixed with 10 ml MSN (5 mg/ml) in PBS for 24 h shaking at room temperature. The resulting DOX-loaded MSN (DMSN) was obtained by centrifugation (16700 × g, 30 min, 4 °C) and rinsed three times with deionized water until supernatant was colorless. DOX loading in MSN was measured by fluorescence method64. Briefly, 3 mg DMSN was dissolved in 2 mL hydrofluoric acid. DOX content was measured by a SpectraMAX M2 microplate reader (Molecular Devices) using a calibration curve of DOX experimentally obtained (Ex 488 nm, Em 590 nm).
DMSN@Pla-Lipo (sPLA2 sensitive) was prepared by thin film hydration. Briefly, 27 mg lipid mixture (10 mg DPPG, 15 mg DPPC, 1 mg cholesterol, 1 mg DSPE-PEG2000) in the mixture of chloroform (4 mL) and methyl alcohol (1 mL) was dried to form the thin film in a round-bottom flask using a rotary evaporator at 55 °C. Then, the film was hydrated with 5 ml of DOX@MSN (containing 5 mg DOX) in HEPES solution. Then the solution was extruded through polycarbonate membranes with pore size of 200 nm using a mini-extruder (Avanti Polar Lipids). The resulted DMSN@Pla-Lipo were obtained through centrifugation (16700 × g, 10 min, 4 °C). As a control, DMSN encapsulated in sPLA2 non- sensitive liposomes (DMSN@Lipo) were prepared using the same method. For this formulation, the lipid mixture was composed of 25 mg HSPC, 1 mg cholesterol, and 1 mg DSPE-PEG2000.
Characterization of DMSN@Pla-Lipo
The shape and structure of the liposomes were observed using TEM (Talos F200X, FEI) and Cryo-TEM (Talos F200C G2, FEI). The size and zeta potential of the liposomes were determined through dynamic light scattering (DLS) using a ZetaSizer Nano ZS instrument (Malvern, UK).
Forster resonance energy transfer (FRET) assay was used to characterize the liposome structure. For this test, MSN was labeled with iFluor 647 as we previously described65, and the liposome membrane was labeled with DiR, generating a dual-fluorophore labeled nanosystem. The distinct structure of the liposomes afforded a short distance between the two fluorescent probes. FRET signal (Ex 650 nm, Em 770 nm) was examined using SpectraMAX M2 microplate reader (Molecular Devices). Pla-Lipo (DiR), MSN (iFluor 647), and their mixture were included as controls.
Further, DeltaVision OMX SR super-resolution microscopy (GE Healthcare) was used to identify the spatial position of MSN and lipid bilayer of MSN@Pla-Lipo, in which MSN and liposome membrane were labeled with iFluor 647 and DiO, respectively. Also, nano-flow cytometry (Flow NanoAnalyzer, Xiamen, China)66 was used to examine the structure and purity of the dual-fluorophore labeled nanosystems.
Identification of Pla-Lipo responsiveness to sPLA2
The responsiveness of Pla-Lipo to sPLA2 was examined through several methods. First, the morphology of Pla-Lipo before and after sPLA2 treatment was observed and compared under TEM. For sPLA2 treatment, the liposomes were incubated in the enzyme-contained COLO205 conditioned culture medium (CCM) at 37 °C for 1 h. COLO205 CCM was prepared after culturing 5×104 COLO205 in RPMI 1640 medium for 48 h. The sPLA2 activity concentration (144.5 nmol/min/mL) in COLO205 CCM was measured by a sPLA2 assay kit (Cayman Chemical, Ann Arbor, USA). HT29 CCM with almost none sPLA2 (0.9 nmol/min/mL) was prepared and used as a control27.
Second, sulforhodamine B (SRB) leakage test was performed to detect the Pla-Lipo responsiveness to sPLA241. Briefly, SRB with self-quenching concentration (50 mM) was encapsulated in the aqueous cavity of liposomes. The resulting SRB@Pla-Lipo was then incubated with bee venom sPLA2, COLO205 CCM, or HT29 CCM, respectively. The activity concentration of sPLA2 used in this test was 144.5 nmol/min/mL when involved. After 15 min incubation, SRB fluorescence recovery which indicated the disruption of liposomal membrane and SRB leakage was visualized (Ex 490 nm, Em 590 nm) in an Xenogen IVIS spectrum/CT imaging instrument. Further, ultrafiltration was performed to collect the released SRB in the filtrate, which was quantified through fluorescence detection (Ex 490 nm, Em 590 nm). The SRB release ratios after 15-, 30-, and 45-min incubation with sPLA2 or CCM were determined.
Third, the changes of particle sizes or zeta potentials caused by COLO205 CCM treatment were examined using both DLS and nanoparticle tracking analysis (NTA, ZetaView PMX120). In all above tests, sPLA2 non-sensitive liposomes were included as a control.
DOX release from DMSN@Pla-Lipo
To investigate the influence of sPLA2 on DOX release, DMSN@Pla-Lipo was dispersed in various media, including PBS (pH 7.4 and 5.5) with or without sPLA2 (activity concentration, 144.5 nmol/min/mL) and PBS containing 10% FBS, in the centrifuge tubes. The tubes were placed in a 37 °C gas bath and shaken at 120 rpm. After 1, 2, 4, 8, 12, 16, and 24 h, respectively, the tubes were centrifugated (16700 ×g, 30 min, 4 °C) to pellet the nanoparticles. The DOX content in the supernatant was quantified through fluorescence detection (Ex 488 nm, Em 590 nm) for the estimation of cargo release ratio.
Cellular uptake and cytotoxicity
For cell uptake assay, COLO205 cells (5×104 cell per well) were seeded onto a coverslip in 24-well plate overnight. The cells were then incubated with MSN@Pla-Lipo (containing 0.6 ng/mL MSN), in which MSN was labeled with iFluor 647. After 3 h, the cells were washed with Dulbecco’s phosphate-buffered saline (DPBS) solution for 3 times. Then, the cell nuclei were stained with 4′,6-diamidino-2-phenylindole (DAPI) and the cell membrane was labeled with DiO. Cell uptake indicated with the fluorescence iFluor 647 (Ex 649 nm, Em 664 nm) was observed under a confocal laser scanning microscopy (Leica TCS SP8). Flow cytometry (Cytomics FC500, Beckman Coulter) was also used to quantify the cell-associated fluorescence intensity. MSN alone and MSN@Lipo were included as controls.
For cell viability assay, COLO205 cells were seeded in 96-well plates at a density of 8000 cells per well for 12 h. The medium was then replaced with fresh medium containing DMSN, DMSN@Lipo, or DMSN@Pla-Lipo at DOX dose of 0.001, 0.01, 0.1, 1, 10, and 100 µg/mL, respectively. After 24 h incubation, cell viabilities were detected using Cell Counting Kit-8 (Dojindo, Laboratories, Kumamoto, Japan).
Cytotoxicity was also qualitatively evaluated using calcein-AM and propidium iodide (PI) dual-staining test. Calcein-AM can be enzymatically converted into calcein (green fluorescence) in live cells, and the nuclei of dead cells are stained with PI (red fluorescence). After 24 h incubation with various DOX-contained formulations (DOX, 1 μg/mL), cell medium was replaced with PBS, and cell viability was examined with the calcein-AM/PI dual-staining test. The cells were photographed under the CLSM (Leica TCS SP8).
Tumor spheroid penetration and cytotoxicity assay
The 3D multicellular spheroids were cultured according to the method previously described67. Briefly, COLO205 cells were seeded at a density of 1 × 104 cells in ultralow attachment, round bottom 96-well plates. After 24 h incubation, the COLO205 tumor spheroids were formed and the medium was replaced by RPMI 1640 medium containing the iFluor 647-labeled liposomes (iFluor 647, 800 ng/mL) for penetration assay. After 36 h incubation, the spheroids were harvested and washed with PBS three times. The fluorescence of iFluor 647 (Ex 649 nm, Em 664 nm) at different depths from the spheroid surface was observed under CLSM and quantified using ImageJ.
The toxicity of DOX-contained formulations (DMSN, DMSN@Lipo, or DMSN@Pla-Lipo), to the tumor spheroids were also evaluated. The tumor spheroids were incubated with the formulations containing 1 µg/mL DOX for 36 h. The cell viability was evaluated using both calcein-AM/PI dual-staining test and flow cytometry (Cytomics FC500, Beckman Coulter) after FITC-Annexin V and PI staining.
Blood clearance kinetics
Female BALB/c nude mice (n = 5) were injected with DMSN@Pla-Lipo and DMSN@Lipo at DOX dose of 7 mg/kg. At 0.5, 1, 2, 4, 8, 12, 24, and 48 h post injection, 50 μL blood was sampled from orbital vein for DOX quantification68. Briefly, blood was centrifuged at 1500 rpm for 15 min at 4 °C. Then, 20 μL serum was dispersed in 100 μL extraction buffer (containing 10% hydrofluoric acid and 90% isopropanol), and vortexed for 30 min. DOX was then assayed using fluorescent detection (Ex 488 nm, Em 590 nm). The drug concentration versus time plot was drawn and pharmacokinetic parameters were calculated using the WinNonlin software (Version 6.1, Pharsight, Mountain View, CA) according to noncompartmental model.
Orthotopic colorectal cancer model and characterization of sentinel LN and organ metastases
The orthotopic colorectal cancer model was established according to our previous report5. Briefly, female BALB/c nude mice were anesthetized with ketamine and xylazine. A lower ventral median incision was made to expose the cecum. Then, 3×106 COLO205-luc-GFP cells in the mixture of 10 μL Matrigel and 40 μL culture medium were inoculated into the subserosa layer of the cecum wall using a 30 gauge needle (Hamilton). The injection site was then pressed with a cotton swab for leakage prevention. The cecum was then put back into the abdominal cavity and the abdominal wall and skin were sutured.
The orthotopic tumor formation and growth were monitored using the IVIS Spectrum/CT imaging system (Perkin Elmer). For lymph node and organ metastasis pattern monitoring, the mice at different time points (days 7, 14, 21, and 28) after tumor cell inoculation were sacrificed. The mesenteric LNs and major organs (heart, liver, spleen, lung, and kidney) were excised for ex vivo bioluminescence imaging to examine the metastasis.
Accumulation of DMSN@Pla-Lipo in primary tumors and metastatic LNs
MSN was labeled with iFluor 647, and then the fluorescent MSN@Pla-Lipo or MSN@Lipo was (iFluor 647, 0.2 mg/kg) i.v. injected to the orthotopic COLO205-luc-GFP tumor-bearing mice. After 1, 2, 4, 8, 12, and 24 h, respectively, the mice (n = 3) from each group were sacrificed, and the primary tumors and mesenteric sentinel LN (1st LN) were excised for fluorescence imaging (Ex 649 nm, Em 664 nm) using the IVIS Spectrum/CT system. MSN accumulation (indicated as iFluor 647 fluorescence intensity) in primary tumors and metastatic sentinel LNs with the time were thus obtained. Further, the accumulation of iFluor 647-labeled MSN in the 2nd mesenteric LN with or without metastases (n = 5) was also characterized.
In another test, the time-dependent DOX contents in both primary tumors and metastatic LNs (1st LN) were also characterized after i.v. injection of DMSN@Pla-Lipo or DMSN@Lipo (DOX, 7 mg/kg). For DOX quantification, the tumors and the 1st LNs were excised, homogenized and extracted overnight in 90% hydrofluoric acid, and DOX content was determined by fluorescence detection (Ex 488 nm, Em 590 nm).
Microdistribution of MSN@Pla-Lipo in primary tumors and metastatic LNs
On day 28 after tumor cell implantation, mice were i.v. injected with iFluor 647-labeled MSN@Pla-Lipo or MSN@Lipo (iFluor 647, 0.2 mg/kg). After 4 h, the mice were sacrificed, and the tumors were processed for frozen section. The lymphatic vessels were stained with rabbit anti-LYVE1 antibody (1:1000, Abcam) overnight at 4 °C and goat anti-rabbit IgG H&L (Alexa Fluor 488, 1:500, Abcam) for 1 h at room temperature. The sections were observed under CLSM for lymphatic vessels (Ex 488 nm, Ex 515 nm) and MSN (Ex 649 nm, Em 664 nm). The fluorescence intensity of MSN inside tumor lymphatic vessels was quantified using ImageJ.
For the micro-distribution detection in metastatic LNs (1st LN), 8 h after injection of MSN@Pla-Lipo or MSN@Lipo, the metastatic sentinel LNs were excised for frozen section. The lymphatic vessels were stained with rabbit Polyclonal LYVE1 antibodyrabbit anti-LYVE1 antibody (Abcam, Cat#: ab14917, 1:1000) overnight at 4 °C and goat anti-rabbit IgG H&L (Alexa Fluor 488) (Abcam, Cat#: ab150077, 1:500) for 1 h at room temperature. The microvessels in LNs were stained with mouse anti-CD31 (1:1000, ThermoFisher) and goat anti-mouse IgG (Cy3, 1:500, Abcam). The sections were observed under CLSM for lymphatic vessels (Ex 488 nm, Ex 515 nm), blood vessels (Ex 543 nm, Em 570 nm), and MSN (Ex 649 nm, Em 664 nm). For another comparison, on day 28, the tumor-bearing mice were subjected to primary tumor resection5, and MSN@Pla-Lipo was i.v. injected on the same day. The fluorescence intensity of MSN inside lymphatic vessels in LNs was quantified assayed using ImageJ. Further, digital image analysis of the immunofluorescence images of LNs was performed using HALO software (version 3.4.2986, Indica Labs, NM, USA)51. Tissue classification was performed to stratify blood vessels and lymphatic vessels using the Tissue Classifier Module. Then, MSN signal heat map was established for the observation and estimation of MSN distribution in lymphatic vessels.
Therapeutic efficacy in orthotopic colorectal tumor with metastatic LNs
28 days after orthotopic tumor cell inoculation, the tumor-bearing female mice were randomly allocated to six groups, including 1) saline, 2) MSN@Lipo (empty), 3) MSN@Pla-Lipo (empty), 4) free DOX, 5) DMSN@Lipo, and 6) DMSN@Pla-Lipo. Then, the mice were administered with the formulations on days 0 and 4, respectively. The DOX dose was 7 mg/kg, the maximum tolerated dose free DOX in mice69, when involved. The tumor burden in each group (n = 5) was measured weekly on days 0, 7, 14, 21, 28, 35, 42, and 49 by bioluminescence imaging. Body weights of the mice were recorded throughout the study. The mice were sacrificed when the bioluminescence intensity reached 3 × 1010 photons/s. Mice will also be died of disease progression and metastasis. The mouse survival time was monitored until day 90. On day 5 (24 h after the last injection), mice in each group (n = 3) were sacrificed, and major organs (heart, liver, spleen, liver, and kidney) were processed for hematoxylin and eosin (H&E) staining and pathological examination. Sex of the animals was not considered as it was not postulated as an contributing factor in this study.
In a separate study, metastases in mesenteric sentinel LNs (1st LN) and distant major organs were investigated. When one mouse of the saline group died of the tumor (day 19), sentinel LNs and organs (liver, spleen, lung, kidney, and intestine) of the mice from all groups (n = 5) were excised, overlaid with a substrate mix solution (0.5 mg/mL D-luciferin and 1 mM ATP in 0.01 M PBS containing bivalent magnesium ions), and ex vivo imaged under the Xenogen IVIS spectrum system. Further, LNs were digested with collagenase I and DNase to generate single-cell suspensions70. Then, the cells were collected and diluted to 1 × 107 cells/mL. COLO205 cells expressing GFP were identified using Attune NxT Flow Cytometer (Thermo Fisher Scientific). Data were analyzed using FlowJo 10.4 software (FlowJo, Ashland, OR).
RNA sequencing (RNA-seq)
On day 5 (24 h after the last injection), mesenteric sentinel LNs (1st LN) treated with DMSN@Pla-Lipo or DMSN@Lipo (n = 3) were excised for RNA extraction and sequencing by XuRan Biological (Shanghai, China). Differentially expressed genes (DEGs) were identified when the fold change was > 2 and p value was < 0.05. Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analysis and Gene set enrichment analysis (GSEA) were performed to identify the significantly enriched pathway when p value was less than 0.05.
Blood analysis
Healthy female BALB/c nude mice (n = 3) were i.v. administered with the liposomes (DOX, 7 mg/kg) on days 0 and 4. On day 5 (24 h after the second injection), retro-orbital blood was collected. Serum biochemistry and complete blood analysis were performed in Drug Safety Evaluation Research Center (Shanghai Institute of Materia Medica, Shanghai, China).
Footpad tumor model and therapeutic efficacy
To evaluate the influence of the lymph node-drained DOX on T cells, an immune-competent model is needed. A footpad tumor model with specific treatment groups were designed for this study. Briefly, 5 × 105 mouse CT-26-luc cancer cells (GeneCopoeia) in 50 μL of PBS were subcutaneously injected into the right hind food sole of female BALB/c mice to establish the footpad tumor model24. Thus, the sentinel LNs (1st LNs) in this tumor model were the popliteal LNs. The tumor-bearing mice were randomly allocated to four groups (n = 5): 1) saline, 2) DMSN@Lipo, 3) DMSN, 4) DMSN@Pla-Lipo pre-incubated with sPLA2 (144.5 nmol/min/mL, activity concentration) for 30 min.
When the tumor grew up to ~50 mm3, a single intratumorally injection of the DOX-contained formulations (0.7 mg/kg) was performed. When the tumor volume of one mouse in the saline group grew beyond 300 mm3, the tumors and sentinel LNs were excised. The tumor volume (V) was calculated as follows: V= (length) × (width)2/2. The LNs were overlaid with a substrate mix solution (0.5 mg/mL D-luciferin and 1 mM ATP in 0.01 M PBS containing bivalent magnesium ions) and imaged under the Xenogen IVIS spectrum system. Further, LNs were digested with collagenase I and DNase to generate single-cell suspensions. Then, the cells were collected and diluted to 1 × 107 cells/mL. 100 µL cells were stained using fluorescent conjugated antibodies. For CD4+ cell detection, the cells were stained with rat anti-mouse CD3 (APC, BioLegend) and rat anti-mouse CD4 (FITC, BioLegend) antibodies. For CD8+ T cell detection, the cells were stained with rat anti-mouse CD3 (APC, BioLegend) and rat anti-mouse CD8a (PerCP-Cy5.5, BioLegend) antibodies. The flow cytometry assay was performed using Attune NxT Flow Cytometer (Thermo Fisher Scientific). Data were analyzed using FlowJo 10.4 software (FlowJo, Ashland, OR).
Statistics & reproducibility
The objective of this study was to develop a multistage drug delivery approach for the treatments of both primary solid tumors and associated LN metastases. To investigate the multistage delivery property of DMSN@Pla-Lipo, we designed a series of in vitro and in vivo experiments. For in vivo experiments, orthotopic colorectal murine tumor models with metastatic LNs were randomly assigned into treatment groups. The sample size was determined based on previous experience and preliminary tests. Sample sizes are denoted in figure legends. Statistical analysis was performed using GraphPad Prism 8.0.1 software (La Jolla, CA). No data were excluded from the analyses. Log-rank (Mantel-Cox) test, two-tailed unpaired t test, one-way ANOVA with Tukey’s multiple comparisons test, or two-tailed non-parametric Mann-Whitney test were used for the examination of differences between groups. P-value below 0.05 was considered significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All RNA-seq raw data have been deposited to NCBI Sequence Read Archive (SRA) (https://www.ncbi.nlm.nih.gov/sra) with the identified BioProject ID: PRJNA1078446. The individual de-identified participant information is summarized in Table S1 with informed consent from patients for disclosing this data obtained. All other data supporting the findings in this work are provided in the main article, supplementary information or source data file. Source data are provided with this paper.
References
Stacker, S. A. et al. Lymphangiogenesis and lymphatic vessel remodelling in cancer. Nat. Rev. Cancer 14, 159–172 (2014).
Pereira, E. R. et al. Lymph node metastases can invade local blood vessels, exit the node, and colonize distant organs in mice. Science 359, 1403–1407 (2018).
Digesu, C. S., Weiss, K. D. & Colson, Y. L. Near-infrared sentinel lymph node identification in non-small cell lung cancer. JAMA Surg 153, 487–488 (2018).
Kwon, I. G., Son, T., Kim, H. I. & Hyung, W. J. Fluorescent lymphography-guided lymphadenectomy during robotic radical gastrectomy for gastric cancer. JAMA Surg 154, 150–158 (2019).
Feng, H. Y. et al. Targeted micellar phthalocyanine for lymph node metastasis homing and photothermal therapy in an orthotopic colorectal tumor model. Nano-Micro Lett 13, 145 (2021).
Oshikiri, T. et al. Is thoracic duct resection necessary for esophageal squamous cell carcinoma patients treated with neoadjuvant chemoradiotherapy? a propensity-matched analysis based on the comprehensive registry of esophageal cancer in Japan. Ann. Surg. Oncol. 30, 2691–2698 (2023).
Nakamura, Y. et al. Surgical damage to the lymphatic system promotes tumor growth via impaired adaptive immune response. J. Dermatol. Sci. 90, 46–51 (2018).
Harter, P. et al. A randomized trial of lymphadenectomy in patients with advanced ovarian neoplasms. N. Engl. J. Med. 380, 822–832 (2019).
Li, B. et al. Fueling sentinel node via reshaping cytotoxic T lymphocytes with a flex-patch for post-operative immuno-adjuvant therapy. Nat. Commun. 14, 2518 (2023).
van der Schaaf, M., Johar, A., Wijnhoven, B., Lagergren, P. & Lagergren, J. Extent of lymph node removal during esophageal cancer surgery and survival. J. Natl. Cancer Inst. 107, (2015).
Su, Z. et al. Novel nanomedicines to overcome cancer multidrug resistance. Drug Resist. Updat. 58, 100777 (2021).
Barenholz, Y. Doxil®–the first FDA-approved nano-drug: lessons learned. J. Control. Release 160, 117–134 (2012).
Guidolin, K. & Zheng, G. Nanomedicines lost in translation. ACS Nano 13, 13620–13626 (2019).
Cabral, H. et al. Systemic targeting of lymph node metastasis through the blood vascular system by using size-controlled nanocarriers. ACS Nano 9, 4957–4967 (2015).
Schudel, A. et al. Programmable multistage drug delivery to lymph nodes. Nat. Nanotechnol. 15, 491–499 (2020).
Liang, C. et al. Tumor metastasis inhibition by imaging-guided photothermal therapy with single-walled carbon nanotubes. Adv. Mater. 26, 5646–5652 (2014).
Li, X. et al. MPEG-DSPE polymeric micelle for translymphatic chemotherapy of lymph node metastasis. Int. J. Pharm. 487, 8–16 (2015).
Kim, T., Suh, J., Kim, J. & Kim, W. J. Lymph-directed self-immolative nitric oxide prodrug for inhibition of intractable metastatic cancer. Adv. Sci. 9, 2101935 (2022).
Schudel, A., Francis, D. M. & Thomas, S. N. Material design for lymph node drug delivery. Nat. Rev. Mater. 4, 415–428 (2019).
Trevaskis, N. L., Kaminskas, L. M. & Porter, C. J. From sewer to saviour - targeting the lymphatic system to promote drug exposure and activity. Nat. Rev. Drug Discov. 14, 781–803 (2015).
Wong, C. et al. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc. Natl. Acad. Sci. Usa. 108, 2426–2431 (2011).
Haynes, M. T. & Huang, L. Multistage delivery technologies: multifunctional, interdisciplinary approaches to nanomedicine. Mol. Ther. 24, 849–851 (2016).
Shi, J., Kantoff, P. W., Wooster, R. & Farokhzad, O. C. Cancer nanomedicine: progress, challenges and opportunities. Nat. Rev. Cancer 17, 20–37 (2017).
Liu, J. et al. Enhanced primary tumor penetration facilitates nanoparticle draining into lymph nodes after systemic injection for tumor metastasis inhibition. ACS Nano 13, 8648–8658 (2019).
Tang, L. et al. Investigating the optimal size of anticancer nanomedicine. Proc. Natl. Acad. Sci. Usa. 111, 15344–15349 (2014).
Mei, L. et al. Effective treatment of the primary tumor and lymph node metastasis by polymeric micelles with variable particle sizes. J. Control. Release 292, 67–77 (2018).
Pourhassan, H. et al. Revisiting the use of sPLA(2)-sensitive liposomes in cancer therapy. J. Control. Release 261, 163–173 (2017).
Hansen, A. H., Mouritsen, O. G. & Arouri, A. Enzymatic action of phospholipase A2 on liposomal drug delivery systems. Int. J. Pharm. 491, 49–57 (2015).
Yamashita, S., Yamashita, J. & Ogawa, M. Overexpression of group II phospholipase A2 in human breast cancer tissues is closely associated with their malignant potency. Br. J. Cancer 69, 1166–1170 (1994).
Yamashita, S. et al. Elevation of serum group II phospholipase A2 levels in patients with advanced cancer. Clin. Chim. Acta 228, 91–99 (1994).
Peng, Z., Chang, Y., Fan, J., Ji, W. & Su, C. Phospholipase A2 superfamily in cancer. Cancer Lett 497, 165–177 (2021).
Khan, S. A. & Ilies, M. A. The Phospholipase A2 Superfamily: Structure, Isozymes, Catalysis, Physiologic and Pathologic Roles. Int. J. Mol. Sci. 24, 1353 (2023).
Davidsen, J., Jorgensen, K., Andresen, T. L. & Mouritsen, O. G. Secreted phospholipase A(2) as a new enzymatic trigger mechanism for localised liposomal drug release and absorption in diseased tissue. Biochim. Biophys. Acta 1609, 95–101 (2003).
Bilchik, A. et al. Surgical quality and nodal ultrastaging is associated with long-term disease-free survival in early colorectal cancer: an analysis of 2 international multicenter prospective trials. Ann. Surg 252, 467–474 discussion 474-466 (2010).
Itabashi, M. et al. Lymph node positivity in one-step nucleic acid amplification is a prognostic factor for postoperative cancer recurrence in patients with stage ii colorectal cancer: a prospective, multicenter study. Ann. Surg. Oncol. 27, 1077–1083 (2020).
Zhou, S. et al. Chemically engineered mesoporous silica nanoparticles-based intelligent delivery systems for theranostic applications in multiple cancerous/non-cancerous diseases. Coord. Chem. Rev. 452, 214309 (2022).
Vallet-Regí, M., Schüth, F., Lozano, D., Colilla, M. & Manzano, M. Engineering mesoporous silica nanoparticles for drug delivery: where are we after two decades? Chem. Soc. Rev. 51, 5365–5451 (2022).
Janjua, T. I., Cao, Y., Yu, C. & Popat, A. Clinical translation of silica nanoparticles. Nat. Rev. Mater. 6, 1072–1074 (2021).
Zanoni, D. K. et al. Use of ultrasmall core-shell fluorescent silica nanoparticles for image-guided sentinel lymph node biopsy in head and neck melanoma: a nonrandomized clinical trial. JAMA Netw. Open 4, e211936 (2021).
Lai, X. et al. Light-triggered efficient sequential drug delivery of biomimetic nanosystem for multimodal chemo-, antiangiogenic, and anti-mdsc therapy in melanoma. Adv. Mater. 34, e2106682 (2022).
Miranda, D. et al. Multifunctional liposomes for image-guided intratumoral chemo-phototherapy. Adv. Healthc. Mater. 6, 1700253 (2017).
Zahednezhad, F., Zakeri-Milani, P., Shahbazi Mojarrad, J. & Valizadeh, H. The latest advances of cisplatin liposomal formulations: essentials for preparation and analysis. Expert Opin. Drug Deliv. 17, 523–541 (2020).
Ponta, A., Fugit, K. D., Anderson, B. D. & Bae, Y. Release, partitioning, and conjugation stability of doxorubicin in polymer micelles determined by mechanistic modeling. Pharm. Res. 32, 1752–1763 (2015).
Wang, Y. & Kohane, D. S. External triggering and triggered targeting strategies for drug delivery. Nat. Rev. Mater. 2, 17020 (2017).
Wei, Y. et al. Phospholipase A2 inhibitor-loaded micellar nanoparticles attenuate inflammation and mitigate osteoarthritis progression. Sci. Adv. 7, eabe6374 (2021).
Liu, H.-J. et al. Integrated combination treatment using a “smart” chemotherapy and microRNA delivery system improves outcomes in an orthotopic colorectal cancer model. Adv. Funct. Mater. 28, 1801118 (2018).
Liu, X. et al. Irinotecan delivery by lipid-coated mesoporous silica nanoparticles shows improved efficacy and safety over liposomes for pancreatic cancer. ACS Nano 10, 2702–2715 (2016).
Minchinton, A. I. & Tannock, I. F. Drug penetration in solid tumours. Nat. Rev. Cancer 6, 583–592 (2006).
Hirakawa, S. et al. VEGF-A induces tumor and sentinel lymph node lymphangiogenesis and promotes lymphatic metastasis. J. Exp. Med. 201, 1089–1099 (2005).
Harrell, M. I., Iritani, B. M. & Ruddell, A. Tumor-induced sentinel lymph node lymphangiogenesis and increased lymph flow precede melanoma metastasis. Am. J. Pathol. 170, 774–786 (2007).
Shi, D. et al. USP14 promotes tryptophan metabolism and immune suppression by stabilizing IDO1 in colorectal cancer. Nat. Commun. 13, 5644 (2022).
Tauriello, D. V. F. et al. TGFβ drives immune evasion in genetically reconstituted colon cancer metastasis. Nature 554, 538–543 (2018).
Zhang, N. et al. Novel therapeutic strategies: targeting epithelial-mesenchymal transition in colorectal cancer. Lancet Oncol 22, e358–e368 (2021).
Cheung, P. et al. Regenerative reprogramming of the intestinal stem cell state via hippo signaling suppresses metastatic colorectal cancer. Cell Stem Cell 27, 590–604.e599 (2020).
Reticker-Flynn, N. E. et al. Lymph node colonization induces tumor-immune tolerance to promote distant metastasis. Cell 185, 1924–1942.e1923 (2022).
Ji, H. et al. Lymph node metastasis in cancer progression: molecular mechanisms, clinical significance and therapeutic interventions. Signal Transduct. Target. Ther. 8, 367 (2023).
Nguyen, L. N. M. et al. The exit of nanoparticles from solid tumours. Nat. Mater. 22, 1261–1272 (2023).
Zhang, Y. N. et al. Nanoparticle size influences antigen retention and presentation in lymph node follicles for humoral immunity. Nano Lett 19, 7226–7235 (2019).
Porter, C. J. H. & Trevaskis, N. L. Targeting immune cells within lymph nodes. Nat. Nanotechnol. 15, 423–425 (2020).
Lu, Y., Aimetti, A. A., Langer, R. & Gu, Z. Bioresponsive materials. Nat. Rev. Mater. 2, 16075 (2016).
Mura, S., Nicolas, J. & Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 12, 991–1003 (2013).
Li, X., Lovell, J. F., Yoon, J. & Chen, X. Clinical development and potential of photothermal and photodynamic therapies for cancer. Nat. Rev. Clin. Oncol. 17, 657–674 (2020).
Gao, Y. et al. Metal phenolic network-integrated multistage nanosystem for enhanced drug delivery to solid tumors. Small 17, e2100789 (2021).
Liu, H.-J. et al. Integrated Combination Treatment Using a “Smart” Chemotherapy and MicroRNA Delivery System Improves Outcomes in an Orthotopic Colorectal Cancer Model. Adv. Funct. Mater. 28, 1801118 (2018).
Dong, X. et al. Biomimetic, hypoxia-responsive nanoparticles overcome residual chemoresistant leukemic cells with co-targeting of therapy-induced bone marrow niches. Adv. Funct. Mater. 30, 2000309 (2020).
Choi, D. et al. Mapping subpopulations of cancer cell-derived extracellular vesicles and particles by nano-flow cytometry. ACS Nano 13, 10499–10511 (2019).
Ivascu, A. & Kubbies, M. Rapid generation of single-tumor spheroids for high-throughput cell function and toxicity analysis. J. Biomol. Screen. 11, 922–932 (2006).
Luo, D. et al. Intrabilayer (64)Cu Labeling of photoactivatable, doxorubicin-loaded stealth liposomes. ACS Nano 11, 12482–12491 (2017).
Luo, D. et al. Doxorubicin encapsulated in stealth liposomes conferred with light-triggered drug release. Biomaterials 75, 193–202 (2016).
Liu, X. Y. et al. A nano-innate immune system activator for cancer therapy in a 4T1 tumor-bearing mouse model. J Nanobiotechnol 20, 54 (2022).
Acknowledgements
The authors thank the Core Facility of Basic Medical Sciences (SJTU-SM) for the help in the flow cytometry assay. C.F. was supported by the National Natural Science Foundation of China (82373448, 82073379, and 81773274), the Program of Shanghai Academic Research Leader (Shanghai Municipal Science and Technology Commission) (22XD1401700), and Shanghai Municipal Health Commission (2022XD035). P.S. was supported by the National Natural Science Foundation of China (82070634), and the Shanghai Municipal Science and Technology Commission (23ZR1458200, 20ZR1451700).
Author information
Authors and Affiliations
Contributions
Y.Y., P.S., and C.F. conceptualized the study. Y.Y., Q.L., H.Y.F., and Y.Z. developed the methodology. Y.Y., Q.L., H.Y.F., Y.Z., X.L., M.H.Z., J.W., J.S., Y.H., L.Z., Q.L., Z.Y., and H.Z.C. participated in investigations. P.S. and C.F. supervised the project. Y.Y., Q.L., and C.F. wrote the original draft. J.F.L. participated in the review and editing of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Leng Han, Yoon Yeo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, Y., Lin, Q., Feng, HY. et al. A multistage drug delivery approach for colorectal primary tumors and lymph node metastases. Nat Commun 16, 1439 (2025). https://doi.org/10.1038/s41467-025-56768-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-56768-z