Abstract
Age-related macular degeneration (AMD) is a leading cause of blindness in people over 50. AMD and cardiovascular disease share risk factors including age, impaired lipid metabolism, and extracellular lipid deposition. Because of its importance in age-related diseases, we hypothesize that apolipoprotein M (ApoM), a lipocalin that binds sphingosine-1-phosphate (S1P), might restore lipid homeostasis and retinal function in AMD. In support, we find that human patients with AMD demonstrate significantly reduced ApoM compared to controls. In mice with impaired retinal cholesterol efflux, ApoM improves retinal pigment epithelium (RPE) function and lipotoxicity in an S1P- and S1P receptor 3-dependent manner. Ultrastructural evidence of enhanced melanosome-lipid droplet interactions led us to hypothesize and demonstrate that ApoM-S1P signaling drives RPE-specific lysosomal lipid catabolism. RPE-specific knockout of lysosomal acid lipase recapitulates features of AMD. Our study defines a novel role for ApoM/S1P signaling in AMD driven by RPE lipotoxicity, mediated by cell-autonomous lysosomal lipid catabolism.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is the leading cause of blindness among Americans over 501,2,3. In its early and intermediate stages, AMD is marked by the buildup of lipoprotein-rich deposits—either under the neurosensory retina (sub-retinal drusenoid deposits, or SDD) or beneath the retinal pigment epithelium (RPE), known as drusen4,5. Vision loss occurs when AMD advances to one of its two late-stage forms. The first, known as “wet” AMD, involves abnormal blood vessel growth (choroidal neovascularization or CNV). Though it represents only about 20% of advanced cases, it accounts for roughly 80% of AMD-related vision loss6. The second form, advanced “dry” AMD, progresses to geographic atrophy (GA), a condition characterized by the atrophic degeneration of retinal neurons7.
Current treatments are limited to the advanced stages of the disease8. The only recommended intervention for early or intermediate AMD is micronutrient supplementation1,9. This underscores a critical gap in our understanding of the molecular mechanisms driving early dry AMD, and the lack of effective strategies to prevent its progression to GA or CNV and resulting vision loss. Anti-VEGF injections are used to manage wet AMD by reducing the risk of sudden vision loss, but they do not halt the ongoing neurodegeneration associated with the underlying dry form10,11,12. For GA, recently approved intravitreal C3 and C5 complement inhibitors offer only modest slowing of disease progression and carry risks such as conversion to wet AMD and retinal vasculitis13,14. These limitations highlight the need for novel and aggressive approaches to prevent the progression of AMD to its vision-compromising stages.
Currently, there are no curative treatments for early or intermediate dry AMD at any stage. Recent studies, including work from our laboratory, have highlighted the pivotal role of cholesterol and lipid accumulation in the initiation and progression of AMD4,7,15. Despite growing recognition that lipid buildup is a key driver of disease progression and vision loss, no therapeutic strategies have been developed to target this underlying cause of AMD. This critical gap underscores the urgent need for innovative approaches that directly address lipid accumulation as a therapeutic target.
In AMD, lipoprotein accumulation and thickening of Bruch’s membrane—the basement membrane beneath retinal pigment epithelial (RPE) cells—disrupt essential solute and lipid transport5,16,17,18. Lipid homeostasis in the RPE is typically regulated by the body’s reverse cholesterol transport (RCT) system, primarily through high-density lipoprotein (HDL) particles19. A key protein in HDL, apolipoprotein A-I (ApoA-I) plays a critical role in RCT by facilitating the removal of cholesterol from extrahepatic tissues. However, impaired RCT leads to the buildup of lipoproteins beneath the retina and RPE, contributing to the hallmark features of AMD4,5. Genetic studies have linked polymorphisms in lipid pathway genes—particularly those involved in cholesterol efflux, the initial step in RCT—to increased AMD risk20,21,22. Furthermore, clinical cohort studies have revealed serum dyslipidemia in AMD patients, supporting the role of lipid imbalance in disease progression4,15,23,24. These findings suggest that promoting the removal of cholesterol and lipids from the sub-retinal space, RPE, and Bruch’s membrane could prevent or slow the formation of drusenoid deposits during the early and intermediate stages of AMD25. Supporting this notion, murine models with knockouts of key genes in cholesterol metabolism, such as ATP binding cassette subfamily A member 1 (Abca1) and ATP binding cassette subfamily G member 1 (Abcg1), in rod photoreceptors, RPE, and myeloid cells exhibit dry AMD-like phenotypes26,27,28,29. Human genetic evidence and murine model data underscore the importance of cholesterol metabolism in RPE survival and function. Therefore, strategies to enhance RPE lipid catabolism may offer promising therapeutic avenues to mitigate AMD progression.
Based on its involvement in aging-related disease and cholesterol metabolism, we hypothesized that the lipocalin apolipoprotein M (ApoM) may play an important role in AMD30,31. Apolipoprotein M (ApoM) is primarily produced by the liver, with a smaller contribution from the kidneys. It binds directly to sphingosine-1-phosphate (S1P)32, a bioactive sphingosine that activates S1P receptors found on various cell types, including RPE cells. Although ApoM makes up only about 5% of HDL and less than 2% of low-density lipoprotein (LDL) particles, it is responsible for binding approximately 70% of circulating S1P33,34,35. ApoM has a broad range of pleiotropic effects, including antioxidant and anti-atherogenic properties36,37, modulation of inflammation, endothelial protection32,38, and promotion of cell survival39. In mice with hepatocyte-specific overexpression of human APOM (ApoMTG), plasma ApoM levels increase 3-5 fold, leading to elevated plasma S1P levels35. Conversely, ApoM knockout mice (ApoMKO) show a 50% reduction in plasma S1P, with no detectable S1P on HDL but normal levels on albumin32. Additionally, ApoM has also been identified as a regulator of lysosomal function in the murine heart40.
Despite evidence linking ApoM to aging, RCT, and lysosomes, few investigations have explored the role of ApoM in AMD41,42. With knowledge of ApoM connected to cholesterol efflux and S1P receptor signaling43, we hypothesized that ApoM and S1P receptor signaling could be involved in AMD pathogenesis. We also considered melanosomes within the RPE could play a role in ApoM-related AMD progression as they are involved in the biogenesis of lysosomal-related organelles and aiding phagosomes by fusion in stressed conditions44,45,46. In plasma samples from individuals with AMD, we observed significantly reduced levels of ApoM compared to healthy controls. When plasma from ApoM overexpressing mice was administered to mice with Abca1 and Abcg1 double knockouts in rod photoreceptors (Abca1/g1-rod/-rod), the development of AMD-like phenotypes was attenuated. In contrast, plasma from ApoM knockout mice had no such effect. Electron microscopy of the retinas from these mice revealed that ApoM appeared to enhance lysosomal lipid catabolism, as evidenced by a decrease in the overall number of lipid droplets, with more lipid droplets found interacting with melanosomes. The deletion of S1P receptor 3 (S1PR3) resulted in an AMD-like phenotype, with electron microscopy showing impaired lipid homeostasis and an increase in lipid droplets within the RPE. Similarly, both whole-body and RPE-specific knockout of lysosomal acid lipase (LAL, gene name Lipa), an enzyme essential for lysosomal cholesterol and triglyceride breakdown, reproduced the dry AMD-like phenotype seen in Abca1/Abcg1-rod/-rod mice. ApoM rich plasma did not rescue either S1PR3 knockout or RPE-specific LAL knockouts, suggesting that ApoM regulates S1P signaling to mediate lipid breakdown in the RPE and help prevent the development of dry AMD phenotypes.
Results
Patients with AMD have lower levels of circulating ApoM
To investigate a correlation between circulating ApoM and AMD, we measured plasma ApoM in age-matched patients with and without AMD by ELISA, the gold standard for measuring ApoM47,48. We measured plasma ApoM in patients diagnosed with AMD (n = 53) and compared their levels to age-matched controls without AMD (n = 328) (Fig. 1A). Patients with AMD had significantly decreased levels of ApoM compared to patients without AMD. These data support a potential role for circulating ApoM in AMD pathogenesis.
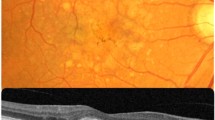
A ApoM levels controlled to total cholesterol levels were measured in patients with (n = 53) or without AMD (n = 328) aged 65 and over. Patients with AMD had significantly lower ApoM levels compared to those without AMD (****p = 0.0000000006, two-tailed Welch’s t-test). B High fat diet fed Abca1/g1-rod/-rod mice were treated with either ApoMKO or ApoMTG plasma (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). C RPE functional assessment using light bleach dark adaptation electroretinography (n = 6) revealed significantly improved functional recovery in ApoMTG plasma treated mice (*p = 0.0271, Two-way ANOVA). D, E Representative TEM imaging of RPE from either ApoMKO or ApoMTG plasma treated Abca1/g1-rod/-rod mice. Red arrows point to lipid droplets. F Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 30) revealed significantly reduced lipid droplets in ApoMTG plasma treated mice (****p = 0.0000011, two-tailed Welch’s t-test). G Quantitative assessment of melanosomes per high-powered field within the RPE (n = 30) revealed significantly increased melanosome counts in ApoMTG plasma treated mice (****p = 0.0000068, two-tailed Welch’s t-test). Full-field scotopic electroretinography (n = 6) demonstrated improved H rod photoreceptor (*p = 0.0343, Two-way ANOVA) but not I inner retina (Two-way ANOVA) function in ApoMTG plasma-treated mice. J Representative traces of 0 dB intensity flashes show an improved waveform from ApoMTg+ injected mice. The scale bar represents 2 μm. Values are mean ± SE. Source data are provided as a Source Data file.
ApoM ameliorates RPE functional deficits in a murine dry AMD-like model
A prior investigation from our laboratory established a dry AMD-like model by conditionally knocking out the cholesterol efflux transporters, Abca1 and Abcg1, in rod photoreceptors in mice (Abca1/g1-rod/-rod). After high fat diet treatment (60% kcal from fat, 25% kcal from carbohydrate, and 15% kcal from protein) for six weeks, Abca1/g1-rod/-rod demonstrated an accelerated neurodegenerative phenotype associated with excessive accumulation of lipid in the RPE26. We also considered utilizing the mouse model of conditional RPE knockout of Abca1 and Abcg127, but the accelerated neurodegeneration seen in this model did not offer a potential opportunity for early intervention in examining the role of ApoM.
We sought to test if concurrent plasma transfer from ApoM transgenic mice that overproduce ApoM (ApoMTG) could ameliorate the RPE and photoreceptor phenotype seen in high fat diet fed Abca1/g1-rod/-rod mice. Plasma transfer of ApoMTG mice has been validated as a strategy for ApoM delivery40. We utilized plasma from ApoM knockout mice (ApoMKO) as controls. High fat diet fed Abca1/g1-rod/-rod mice were injected with 120 μL of either ApoMTG or ApoMKO plasma every other day (Fig. 1B). Using the light bleach dark adaptation electroretinography technique28, we measured RPE function and found significant improvements in the ApoMTG plasma-treated mice by scotopic a-wave maximum measurements (Fig. 1C). These findings suggest that the RPE of ApoMTG plasma-treated Abca1/g1-rod/-rod mice functionally improved.
RPE lipid accumulation is significantly reduced by ApoM plasma transfer
We next assessed the ultrastructural effects of ApoM treatment paradigm in the high fat diet fed Abca1/g1-rod/-rod model using electron microscopy. These mice have previously been shown to have increased lipid droplets in the RPE26. We discovered that ApoMTG plasma-treated Abca1/g1-rod/-rod mice had significantly fewer lipid droplets on electron microscopy in the RPE compared to ApoMKO plasma-treated mice (Fig. 1D–F). A decrease in number of lipid droplets was also associated with significantly increased RPE melanosomes in ApoMTG plasma-treated mice (Fig. 1G). As melanosomes have been reported to be related to lysosomal function44,45,46, we hypothesized that ApoM could be reducing RPE lipotoxicity through lysosome-mediated lipid catabolism.
ApoM plasma transfer improves rod photoreceptor function in high-fat diet-fed Abca1/g1 -rod/-rod mice
As described above, we have previously demonstrated that RPE dysfunction in Abca1/g1-rod/-rod is associated with secondary rod photoreceptor dysfunction26,28. We further hypothesized that ApoM plasma transfer may improve rod photoreceptor function as rod photoreceptor function is closely tied to RPE function49. To measure rod photoreceptor function, we utilized full-field scotopic electroretinography to measure both the a-wave and b-wave amplitudes, which measure rod photoreceptor and inner retina function respectively50 (Fig. 1H–J). Scotopic a-wave amplitudes were significantly improved in ApoMTG treated mice compared to ApoMKO plasma-treated mice. These findings demonstrate that ApoMTG plasma-treated mice demonstrate both improved RPE and rod photoreceptor function.
S1P binding to ApoM is necessary for reduced RPE lipid accumulation and improved rod photoreceptor function
ApoM is the primary carrier of S1P32. We hypothesized that S1P binding to ApoM is necessary for the structural and functional rod photoreceptor and RPE improvement seen in Fig. 1. To test this, we obtained plasma from control mice (ApoMCtrl) and mice with a triple mutation in the ApoM binding site for S1P (ApoMTM)40. ApoMTM produces a mutated ApoM that is unable to bind S1P. We then utilized a similar treatment paradigm (Fig. 1B) to test if ApoM defective for S1P binding rescues the rod and RPE phenotype seen in the Abca1/g1-rod/-rod model (Fig. 2A). In contrast to what we observed with ApoM plasma transfer, full-field scotopic electroretinography revealed reduced scotopic a-wave and b-wave amplitudes in ApoMTM-treated mice (Fig. 2B–D). Thus, mutated ApoM could not functionally improve rod photoreceptors as wild-type ApoM did in Abca1/g1-rod/-rod.
A High fat diet fed Abca1/g1-rod/-rod were treated with plasma from either control mice with human ApoM knocked in (ApoMCtrl) or mice expressing ApoM incapable of binding S1P (ApoMTM) (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). Full-field scotopic electroretinography (n = 4) demonstrated significant reduction in B rod photoreceptor (*p = 0.0469, Two-way ANOVA) and C inner retina function (*p < 0.0199, Two-way ANOVA) in ApoMTM treated mice. D Representative traces of 0 dB intensity flashes show the waveform from ApoMTM treated mice do not recover. E, F Representative TEM imaging of RPE from either ApoMCtrl or ApoMTM plasma treated Abca1/g1-rod/-rod mice. Red arrows point to lipid droplets. G Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 45) revealed significantly increased lipid droplets in ApoMTM plasma treated mice (****p < 0.000000013, two-tailed Welch’s t-test). H Quantitative assessment of melanosomes per high-powered field within the RPE (n = 45) revealed no significant difference according to two-tailed Welch’s t-test without multiple comparisons in melanosome counts between ApoMCtrl and ApoMTM plasma treated mice. Scale bar represents 2 μm. Values are mean ± SE. Source data are provided as a Source Data file.
We also assessed the ultrastructural effects of ApoMTM plasma transfer by electron microscopy. We quantified lipid droplet and melanosome counts within the RPE (Fig. 2E and F) through electron microscopy analysis. Corroborating the phenotype seen in rod photoreceptors, we appreciated significantly increased lipid droplet counts in the ApoMTM treated RPE compared to those of ApoMCtrl treated RPE, despite similar melanosome counts (Fig. 2G and H). These data support that functional ApoM binding to S1P is necessary for the reduction of RPE lipid burden and functional preservation of rod photoreceptors.
S1P receptor 3 knockout mice demonstrate RPE lipotoxicity and visual dysfunction
We next hypothesized which S1P receptor could be mediating RPE lipid amelioration in AMD-like phenotypes. Using publicly available bulk RNA sequencing data of human RPE cells (Supplementary Fig. 1)51, we identified that two of the five S1P receptors, S1P receptor 1 (S1PR1) and S1P receptor 3 (S1PR3), were the predominantly expressed receptors. We first generated conditional RPE knockout mice of S1pr1 (S1pr1-RPE/-RPE) and placed them on a six week high fat diet to discern whether they phenocopy high fat diet fed Abca1/g1-rod/-rod mice (Supplementary Fig. 2A). We did not see any RPE or rod photoreceptor dysfunction in knockout mice compared to wild type controls (Supplementary Fig. 2B–2D).
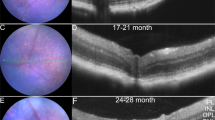
In-situ hybridization data of S1pr3 expression in the eye demonstrated that S1pr3 is expressed in the RPE (Supplementary Fig. 3). We assessed germline S1pr3 knockout mice (S1pr3−/−) to determine if they develop RPE lipotoxicity after six weeks of high-fat diet (Fig. 3A) treatment. Light bleach dark adaptation electroretinography assessment of S1pr3−/− RPE demonstrated significantly reduced RPE function compared to that of wild type RPE (Fig. 3B). Electron micrscopy assessment of RPE ultrastructure demonstrated strikingly similar characteristics of high fat diet fed Abca1/g1-rod/-rod RPE (Fig. 3C and D). Lipid droplet and melanosome quantification of S1pr3−/− RPE showed significantly increased lipid droplet count and decreased melanosome count (Fig. 3E and F) compared to those of wild-types. Full field scotopic electroretinography also showed significantly decreased scotopic a-wave amplitudes in S1pr3−/− (Fig. 3G–I) compared to wild-types. These data suggest that S1PR3 loss-of-function recapitulates the characteristic features of RPE lipotoxicity seen in the Abca1/g1-rod/-rod model.
A S1pr3 germline knockout mice (S1pr3−/−) were generated and placed on 6 weeks of high fat diet and subsequently assessed (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). B RPE functional assessment using light bleach dark adaptation electroretinography (n = 10) revealed significantly reduced functional recovery in S1pr3−/− mice compared to wild-type mice (*p = 0.0462, Two-way ANOVA). C, D Representative TEM imaging of RPE from either wild-type or S1pr3 knockout mice. Red arrows point to lipid droplets. E Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 80) revealed significantly increased lipid droplets in S1pr3 knockout mice (****p = 0.0000000001, two-tailed Welch’s t-test). F Quantitative assessment of melanosomes per high-powered field within the RPE (n = 80) revealed significantly decreased melanosomes in S1pr3 knockout mice (**p = 0.0018, two-tailed Welch’s t-test). Full-field scotopic electroretinography (n = 8) demonstrated reduced G rod photoreceptor (**p = 0.0018, Two-way ANOVA) but not H inner retina (Two-way ANOVA) function in S1pr3 knockout mice. I Representative traces of 0 dB intensity flashes show a diminutive waveform from S1pr3−/−. Scale bar represents 2 μm. Values are mean ± SE. Source data are provided as a Source Data file.
Overexpression of ApoM does not rescue high-fat diet-induced S1pr3 −/− RPE lipotoxicity
We next sought to investigate if ApoM can rescue the high fat diet-induced S1pr3−/− RPE lipotoxicity phenotype. We generated S1pr3−/−/ApoMTG mice and placed them on a 6-week high fat diet (Fig. 4A). No significant differences were appreciated in RPE function as measured by light bleach dark adaptation electroretinography between S1pr3−/− and S1pr3−/−/ApoMTG (Fig. 4B). Ultrastructural analysis of RPE through electron microscopy demonstrated similar features between S1pr3−/− and S1pr3−/−/ApoMTG (Fig. 4C and D). No significant differences were found between S1pr3−/− and S1pr3−/−/ApoMTG in lipid droplet quantification (Fig. 4E). Full-field scotopic electroretinography also did not show significant differences between S1pr3−/− and S1pr3−/−/ApoMTG in scotopic a-wave and b-wave amplitudes (Fig. 4F–H). These data suggest S1PR3 is necessary for ApoM-S1P alleviate RPE lipid burden and associated visual dysfunction.
A S1pr3 germline knockout mice (S1pr3−/−) were crossed with ApoM overexpressing transgenic mice (ApoMTG) to generate S1pr3−/−/ApoMTG mice and placed on 6 weeks of high fat diet and subsequently assessed (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). B RPE functional assessment using light bleach dark adaptation electroretinography (n = 6) revealed no significant differences in functional recovery between S1pr3−/− and S1pr3−/−/ApoMTG mice. C, D Representative TEM imaging of RPE from either S1pr3−/− or S1pr3−/−/ApoMTG mice. Red arrows point to lipid droplets. E Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 42) revealed no significant differences using two-tailed Welch’s t-test without multiple comparisons between S1pr3−/− and S1pr3−/−/ApoMTG mice. Full-field scotopic electroretinography (n = 8) demonstrated no significant differences by two-way ANOVA in F rod photoreceptor and G inner retina between S1pr3−/− and S1pr3−/−/ApoMTG mice. H Representative traces of 0 dB intensity flashes show waveforms do not improve despite ApoMTG treatment in S1pr3−/−. Scale bar represents 2 μm. Values are mean ± SE. Source data is provided as a Source Data file.
ApoM-S1P-mediated clearance of photoreceptor outer segment lipids by RPE requires S1PR3
In the eye, there is a diurnal rhythm associated with the shedding of photoreceptor outer segments (POS). There is extensive shedding of rod outer segments at dawn, while cones shed at dusk. This creates a large lipid burden for the RPE to phagocytose and metabolize daily over the lifetime of the organism52,53,54. To elucidate RPE lipotoxicity mechanisms, we sought to emulate the POS clearance by RPE cells in vitro and ex vivo. We utilized ARPE-19 cells to simulate the lipid burden seen in the in vivo genetic model exacerbated by the high-fat diet. We accomplished this by treating ARPE-19 cells with exogenous photoreceptor outer segments at varying concentrations (Supplementary Fig. 4). This model has been extensively characterized to test RPE phagocytic and lipid processing capacity44,45,55,56. Using commercially available bovine POS, we first visualized if ARPE-19 cells would fluoresce with increasing intensity when treated with FITC-labeled POS (Supplementary Fig. 4A). We treated cells with no POS, or at a 10:1, or 20:1 POS to RPE cell ratio. Cells were treated with POS for 4 hours before fixing and imaging. Indeed, the ARPE-19 cells demonstrated increased intensity of fluorescence according to the concentration of FITC-labeled POS. We then sought to appreciate the amount of neutral lipid through BODIPY staining after POS treatment of RPE cells at a 10:1 and 20:1 POS to RPE ratio (Supplementary Fig. 4B). Cells were treated with POS for 4 hours before fixing and imaging. The 10:1 POS to RPE ratio is typically used to observe baseline phagocytic and processing behavior of RPE55. Indeed, we observed that increased POS feeding led to increased BODIPY staining. We next tested if recombinant ApoM loaded with S1P could decrease BODIPY staining after POS feeding. To test this, we incubated the cells with media containing recombinant ApoM loaded with S1P (25 μg/mL) for an additional 2 hours after 4 hours of POS treatment. We observed reduced BODIPY staining within RPE cells treated with POS after incubation with ApoM-S1P compared to controls that did not receive ApoM-S1P in the medium. These data suggest in vitro ARPE-19 cells respond similarly to ApoM-S1P as in vivo RPE do.
We further sought to test and quantify the effect of POS treatment on RPE cells in an ex vivo ‘eyecup’ system (Fig. 5A). We dissected RPE, choroid, and sclera complex from wild-type mice to compose the ex vivo ‘eyecup’ system. We then incubated the eyecup with different amounts of POS, then subsequently incubated the eyecups with control media or media with recombinant ApoM-S1P. Eyecups were treated with POS for two hours and then treated with ApoM-S1P for two hours55. We calculated the amount of POS necessary for treatment according to a previous report quantifying approximate counts of RPE cells (25,000 cells in one eyecup) in mouse eyecups57. The eyecups were then stained with BODIPY, flat mounted, and imaged (Fig. 5B and C). Of note, eyecups treated with ApoM or S1P alone did not demonstrate a significant effect on BODIPY fluorescence compared to ApoM-S1P, suggesting ApoM and S1P must be present together (Supplementary Fig. 5A and 5B).
A The RPE/choroid/sclera complex was isolated from mouse eyecups to assess ex vivo RPE for lipid burden using BODIPY neutral lipid staining depicted in green (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). Eyecups from wild-type mice were treated with increasing dosages of photoreceptor outer segments (POS) before being treated with either B control media or C media with ApoM-S1P. The same paradigm was tested in eyecups from S1pr3−/− mice also treated with either D control media or E media with ApoM-S1P. F BODIPY fluorescence was quantified from each group and plotted (n = 8). Wild-type RPE treated with ApoM-S1P expressed significantly less BODIPY fluorescence compared to those treated with control media in 0x (****p = 0.000022, post hoc Bonferroni’s multiple comparisons test), 10x (***p = 0.00017, post hoc Bonferroni’s multiple comparisons test), and 20x POS (****p = 0.0000000001, post hoc Bonferroni’s multiple comparisons test) treated groups (****p = 0.0000000001, Two-way ANOVA). ApoM-S1P treated S1pr3KO RPE did not demonstrate significant differences in BODIPY fluorescence compared to control-treated S1pr3KO RPE. The scale bar represents 100 μm. Values are mean ± SE. Source data is provided as a Source Data file.
We utilized the same experimental paradigm of lipid staining ex vivo eyecups from S1pr3−/− mice (Fig. 5D and E). BODIPY fluorescence was then quantified across multiple images (Fig. 5F). Wild-type RPE treated with ApoM-S1P demonstrated significantly reduced BODIPY fluorescence compared to those treated with control media in 0x, 10x, and 20x POS treated groups. However, ApoM-S1P treatment did not significantly change BODIPY fluorescence in S1pr3−/− RPE. Consistent with our in vivo models, these data show ApoM-S1P does not reduce the amount of lipid staining in S1pr3−/− RPE, suggesting that ApoM-S1P requires functional S1PR3 to ameliorate RPE lipid burden. These data support the conclusions from the in vivo genetic and pharmacologic experiments presented above that ApoM-S1P helps reduce lipid burden in wild-type RPE, and S1PR3 function is necessary for adequate lipid processing from POS.
ApoM-S1P does not significantly improve cholesterol efflux capacity in RPE cells
After characterizing the effects of ApoM-S1P on RPE lipotoxicity, we investigated the mechanism of the effect of ApoM-S1P on the lipotoxicity phenotype, utilizing ARPE-19 cells. We performed in vitro administration of ApoM-S1P41 to measure total cholesterol efflux capacity from ARPE-19 cells (Supplementary Fig. 6). Serum from ApoM knockout mice was used as cholesterol acceptors for the assay. Although previous studies suggest ApoM influences macrophage cholesterol efflux43, ApoM-S1P did not significantly affect cholesterol efflux capacity in ARPE-19 cells. These data suggest that ApoM-S1P does not reduce RPE lipid burden through cholesterol efflux, and ApoM-S1P influences cholesterol efflux in a cell-type-dependent manner.
Lipophagy knockout induces RPE lipotoxicity features
Based on our observations of increased melanosome counts with ApoM treatment in Abca1/g1-rod/-rod, enhanced lysosomal lipid catabolism was a suspected mechanism of ApoM-S1P mediated lipid burden amelioration as melanosome and lysosomal function have been closely associated44,45,46. Previous work has demonstrated that ApoM is a novel regulator of autophagy and that ApoM preserves lysosomal function40. We therefore hypothesized that abrogating lysosomal lipid catabolism would recapitulate features of RPE lipotoxicity.
Lysosomal acid lipase (LAL; gene name Lipa) is a critical enzyme that is necessary for lysosomal lipid catabolism58,59. We generated germline LAL knockout mice (Lipa−/−) and placed them on high fat diet to investigate if abrogation of lysosomal lipid catabolism leads to AMD-like phenotypes (Supplementary Fig. 7A). Ultrastructural analyses of RPE demonstrated intracellular lipid droplets that are improperly processed in Lipa−/− mice (Supplementary Fig. 7B and 7C). Light bleach dark adaptation electroretinography of Lipa−/− mice showed decreased RPE function (Supplementary Fig. 7D). Full field scotopic electroretinography demonstrated significantly reduced rod photoreceptor function in Lipa−/− (Supplementary Fig. 7E and 7F). Since LAL is ubiquitously expressed, lack of LAL most likely caused severe effects in all cell types, including photoreceptors.
To pinpoint the role of lysosomal lipid catabolism in RPE, we generated a Lipa conditional RPE knockout (Lipa-RPE/-RPE)60 and placed them on high fat diet (Fig. 6A). Lipa-RPE/-RPE mice demonstrated significantly reduced RPE function by light bleach dark adaptation electroretinography (Fig. 6B). Ultrastructural analyses by electron microscopy of RPE cells showed a significant increase in lipid droplets in the RPE of Lipa-RPE/-RPE (Fig. 6C). Representative images demonstrate increased lipid droplet accumulation in RPE cells of Lipa-RPE/-RPE compared to controls (Fig. 6D and E). However, no significant differences were appreciated in rod photoreceptor function by full field scotopic electroretinography (Supplementary Fig. 8A and 8B).
A RPE-specific lysosomal acid lipase conditional knockout mice (Lipa-RPE/-RPE) were generated and placed on 6 weeks of high fat diet and subsequently assessed (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). B RPE functional assessment using light bleach dark adaptation electroretinography (n = 6) revealed significantly reduced functional recovery in Lipa-RPE/-RPE mice compared to wild-type mice (***p = 0.000468, Two-way ANOVA). C) Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 76) revealed significantly increased lipid droplets in Lipa-RPE-RPE mice (****p = 0.00000000001, two-tailed Welch’s t-test). D, E Representative TEM imaging of RPE from either wild-type or Lipa-RPE/-RPE mice. Red arrows point to lipid droplets. F High fat diet fed Lipa-RPE/-RPE mice were treated with either ApoMKO or ApoMTG plasma (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf). G RPE functional assessment using light bleach dark adaptation electroretinography (n = 6) revealed no significant differences by two-way ANOVA in functional recovery. H Quantitative assessment of lipid droplets per high-powered field within the RPE (n = 100) revealed no significant differences according to two-tailed Welch’s t-test without multiple comparisons in lipid droplet counts. I, J Representative TEM imaging of RPE from either wild-type or Lipa-RPE/-RPE mice. Red arrows point to lipid droplets. The scale bar represents 2 μm. Values are mean ± SE. Source data is provided as a Source Data file.
ApoM plasma transfer therapy does not rescue Lipa knockout-induced RPE lipotoxicity
To test if ApoM can rescue RPE lipotoxicity in Lipa-RPE/-RPE, we utilized ApoM plasma transfer, as performed in Fig. 1C(Fig. 6F). Functional assessment of RPE and rod photoreceptor function demonstrated no significant differences between the two groups (Fig. 6G) (Supplementary Fig. 8C and 8D). Quantification of lipid droplet count by TEM demonstrated no significant differences between groups (Fig. 6H–J). These results suggest that ApoM attenuates RPE lipotoxicity through LAL. Consistent with this effect, we performed in vitro studies in ARPE-19 cells to test the hypothesis that LAL acts downstream of ApoM-S1P signaling. We treated ARPE-19 cells with Lalistat-2 in the presence of ApoM-S1P and examined BODIPY fluorescence after POS treatment (Supplementary Fig. 9). ARPE-19 cells were first treated with POS, then either with ApoM-S1P alone or ApoM-S1P with Lalistat-2, an inhibitor of LAL, then mounted and stained for neutral lipids using BODIPY staining (Supplementary Fig. 9A). Fluorescence intensities were subsequently quantified and analyzed (Supplementary Fig. 9B). Both groups exhibited increased fluorescence with higher doses of POS. Furthermore, cells treated with Lalistat-2 displayed significantly more fluorescence than those not treated with Lalistat-2, despite ApoM-S1P treatment. In aggregate, these results are consistent with LAL acting downstream of ApoM-S1P to reduce RPE lipid burden.
Discussion
In this study, we identified a novel role for the lipocalin ApoM in RPE lipotoxicity as seen in early dry AMD and recapitulated in murine models (Fig. 7). We discovered that patients with AMD had significantly reduced circulating ApoM, as measured by ELISA. We demonstrated that several pathogenic features observed in murine models of dry AMD, such as RPE and rod photoreceptor dysfunction and RPE lipid accumulation, are improved by ApoM. We also demonstrated that the salutary effects of ApoM are contingent on S1P binding. Furthermore, we identified S1PR3 as a critical target of ApoM-S1P as S1pr3 knockout recapitulated dry AMD-like features. While ApoM-S1P reduced the lipid burden of the RPE as seen in the ex vivo eye cup assay, this effect required S1PR3. Finally, we identified a cell-autonomous role for LAL in the RPE, as not only did the RPE-specific LAL knockout develop AMD-like features, but it was not rescued by ApoM therapy. In totality, our studies identify a novel role for ApoM in AMD pathogenesis through RPE lipotoxicity, ApoM/S1P/S1PR3 signaling, and LAL.
ApoM is carried by HDL particles in systemic circulation and is made available to the RPE through the choriocapillaris. ApoM and its binding partner, S1P, activates S1PR3 on the RPE surface to activate lysosomal lipid catabolism to alleviate RPE lipid burden. Inactive S1PR3 allows aberrant accumulation of intracellular lipids within the RPE, leading to dysfunction and potentially increasing the risk to develop dry AMD features. By supplying the RPE with exogenous ApoM-S1P through plasma transfer, we can reduce lipid burden in the RPE through a S1PR3-dependent mechanism and subsequently reduce the risk of dry AMD pathogenesis (created in BioRender. Lee, T. (2025) https://BioRender.com/li4w1zf).
As existing therapies for AMD are tailored towards the advanced stages, we endeavored to explore new therapeutic avenues for the early to intermediate forms of AMD. Utilizing the high fat diet fed Abca1/g1-rod/-rod model, we highlighted the RPE’s limitations of processing improperly loaded photoreceptor outer segments that lead to lipotoxicity reminiscent of early to intermediate AMD. As ABCA1 polymorphisms are a characterized risk factor for AMD21, we believe this is a reasonable model that recapitulates several features of early AMD26. RPE lipotoxicity is a key driver of AMD pathogenesis and progression, underscoring the urgent need for innovative strategies to reduce lipid accumulation in the RPE and associated sub-retinal and sub-RPE regions. The RPE relies primarily on two mechanisms for lipid clearance: efflux and catabolism56,58,61. While ApoM and S1P are known to facilitate cholesterol transport in other cell types, our data show that recombinant ApoM-S1P does not significantly enhance cholesterol efflux in ARPE-19 cells. This led us to explore and alternative role for ApoM in promoting lipid catabolism within the RPE. Our observations, particularly the changes in melanosome and lipid droplet numbers following ApoM plasma transfer, suggest ApoM may enhance lysosomal lipid catabolism. This study as a whole supports the notion that ApoM-S1P signaling upregulates lysosomal acid lipase activity, a mechanism that warrants further investigation.
Our study also establishes a novel role for S1PR3 in AMD pathogenesis in the mouse. While bulk RNA sequencing of human RPE indicates that S1PR1 and S1PR3 are the predominantly expressed S1P receptors, previous investigations have identified other S1P receptors, such as S1PR2, play an essential role in RPE function41. Notably, Terao et al. demonstrated that S1PR2 modulates the inflammatory profile of ARPE-19 cells, and intravitreal administration of a selective S1PR2 inhibitor significantly reduced lesion size in a laser-induced choroidal neovascularization (CNV) model. These findings implicate S1PR2 in the regulation of inflammatory and angiogenic pathways in the RPE and potentially other cell types involved in CNV. Although S1PR4 and S1PR5 are expressed at low levels in RPE, their roles along with that of S1PR2 should be further explored in early-stage dry AMD models to better understand their contributions to disease mechanisms.
It is evident that AMD pathogenesis is complex and influenced by numerous genetic and environmental factors, in addition to the effects of aging on the eye. As such, it is critical to identify and target the earliest triggers of disease pathogenesis prior to catastrophic vision loss. Our study, specifically focused on addressing the fundamental mechanisms of RPE lipotoxicity, highlights a novel therapeutic use of ApoM-S1P to prevent RPE lipotoxicity via enhanced elimination of lipids and deserves further exploration.
Methods
Animals
All animal experiments were conducted in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research and Washington University School of Medicine in St. Louis Animal Care and Use guidelines and after approval by the Institutional Animal Care and Use Committee (IACUC). Animals were monitored daily and euthanized by CO2 at experiment endpoints according to these guidelines. All animal experiments abide by the ARRIVE guidelines. Male and female mice between 8 and 12 weeks old (2-3 months of age) were used in this study. Mice were housed in a 12-hour light/dark cycle with free access to food and water. For high fat diet (HFD) feeding experiments, only male mice were used. We used an adjusted-calorie diet (60% from fat, 25% kcal from carbohydrate, and 15% kcal from protein (ENVIGO, Indianapolis, IN) as HFD, starting from 6 weeks old to the target age of analysis. We used Purina 4043 chow (13% kcal from fat, 62% kcal from carbohydrate, 25% kcal from protein) as the normal diet. ApoMKO 37, ApoMTG 35,40, S1pr3-/− 62, and S1pr1-RPE/-RPE 63 have been described in previous studies and generated in house. Lipa−/− and Lipa-RPE/-RPE mice were donated by Drs. Jaya Mishra (University of Cincinnati College of Medicine) and Dagmar Kratky (Gottfried Schatz Research Center) respectively and generated in house60,64. Mice with RPE conditional knockouts were crossed with mice carrying one copy of the Bestrophin1 (Best1-cre) transgene, which are available from Jackson Laboratories (017557). Mice were fully backcrossed to the inbred C57BL/6J background.
Human dataset
Generation of the human dataset was approved by the Human Research Protection Office of Washington University School of Medicine in St. Louis and the study was conducted according to the Declaration of Helsinki and approved by Danish Ethics committees (no. KF-100.2039/91, KF-01-144/01, H-KF-01-144/01) and the Washington University in St. Louis Institutional Review Board (IRB#201301075). We obtained written informed consent from all patients prior to enrollment in the study. Patients were not excluded based on gender, sex, race, ethnicity, or other socially relevant groupings. We classified samples as coming from patients with no AMD; early AMD; or AMD with geographic atrophy and/or CNV based on established clinical criteria. Early AMD patients had either small or moderate drusen ( < 125 μm) or pigment changes in at least 1 eye but no CNV or geographic atrophy in either eye. Patients with geographic atrophy and/or CNV in at least 1 eye were labeled as such. We excluded any patients receiving immunotherapy, chemotherapy, or radiation for underlying autoimmune/immune-mediated diseases or cancers, which could affect circulating immune cells.
Sandwich ELISA for human unfolded plasma ApoM
We obtained informed consent from patients with dry or wet AMD and collected blood via venous blood draw into K2EDTA-coated BD Vacutainer Venous Blood Collection Tubes. Samples were then deidentified. Plasma was separated and collected after centrifugation. An ELISA plate (Costar 3590 high binding) was coated with 50 μl of capture antibody (clone 1G9) by diluting to 5 μg/ml in TBS (pH 7.4) and incubated at room temperature overnight. The plate was blocked for 2 h with 200 μl of 2% BSA in TBS (pH 7.4). Ten microliters of each plasma sample were mixed with 90 μl of 50 mmol/l DTT (Sigma-Aldrich) in a 0.2 mol/l sodium phosphate buffer (pH 8.5). Disulfide bridges in ApoM were broken by incubating samples at 30 °C for 15 min. One hundred microliters of 0.6 mol/l iodoacetamide (Sigma-Aldrich) in a 0.02 mol/l sodium phosphate buffer (pH 8.0) were then added, and samples were incubated for 1 h at room temperature in the dark to alkylate free cysteines in ApoM and prevent reformation of disulfide bridges. After 1 h, the samples were diluted fifty times (variable for the standard curve) in TBS (pH 7.4) containing 1% BSA and transferred to the ELISA plate for overnight incubation at room temperature. The plate was washed three times with TBS (pH 7.4) and incubated overnight at room temperature with 75 μl of detection antibody (clone EPR2904) diluted to 125 ng/ml in TBS (pH 7.4) containing 1% BSA and 2% Triton-X 100. The plate was washed three times with TBS (pH 7.4) and 0.1% Triton-X 100 and incubated for 2 h with 75 μl of HRP-conjugated anti-rabbit IgG antibody diluted to 125 ng/ml in TBS (pH 7.4) containing 1% BSA and 0.1% Triton-X 100. Finally, the plate was washed three times with TBS (pH 7.4) and 0.1% Triton-X 100, and ApoM was detected by reading absorbance at 492 nm after incubation with 75 μl o-phenylenediamine/hydrogen peroxide solution for 10 min followed immediately by addition of 75 μl 1 mol/l H2SO4. The ApoM concentration of measured samples was determined from the standard curve included in each assay run.
Plasma transfer
Plasma was obtained from either ApoMKO or ApoMTG mice from peripheral blood via the retro-orbital plexus under anesthesia. 120 μL of either ApoMKO or ApoMTG plasma was intraperitoneally injected in Abca1/g1-rod/-rod starting at 6 weeks of age. High fat diet was implemented on the first day of injections. Mice were injected thrice weekly for 6 weeks.
Electroretinography
Full field scotopic ERG was performed as previously described50. A UTAS BigShot System (LKC Technologies Inc.) was used. Mice were dark-adapted overnight. Under red light illumination, mice were anesthetized with an intraperitoneal injection of 86.9 mg/kg ketamine and 13.4 mg/kg xylazine. Pupils were dilated with 1% tropicamide eye drops. Body temperature was maintained at 37 °C with a heating pad. Contact lens electrodes were placed bilaterally with appropriate reference and ground electrodes. The stimulus consisted of a full-field white light flash (10 μs). Raw data were processed using MATLAB software (MathWorks). The a wave amplitude was measured from the average pretrial baseline to the most negative point of the average trace, and the b wave amplitude was measured from that point to the highest positive point.
For testing dark adaptation, we modified the protocol as previously described65. Briefly, we used a UTAS BigShot System (LKC Technologies Inc.) to get scotopic a-waves. A bright LED light (150,000 lux) was applied to both eyes for 15 seconds to photobleach an estimated 90% of the visual pigment. The recovery of the ERG responses was monitored at fixed post-bleach time points within 100 minutes after the bleach. The sensitivity was calculated as the ratio of dim flash response amplitude and the corresponding flash intensity in the linear range of the intensity-response curve. The post-bleach sensitivities were normalized to their dark-adapted prebleach level.
Transmission electron microscopy
We performed transmission electron microscopy as previously described50. For ultrastructural analyses, eyecups were fixed in 2% paraformaldehyde (PFA)/2.5% glutaraldehyde (Polysciences Inc.) in 100 mM sodium cacodylate buffer, pH 7.2, for 2 hours at room temperature and then overnight at 4 °C. Samples were washed in sodium cacodylate buffer at room temperature and postfixed in 1% osmium tetroxide (Polysciences Inc.) for 1 hour. Samples were then rinsed extensively in dH20 prior to en bloc staining with 1% aqueous uranyl acetate (Ted Pella Inc.) for 1 hour. Following several rinses in dH2O, samples were dehydrated in a graded series of ethanol and embedded in Eponate 12 resin (Ted Pella Inc.). Sections of 95 nm were cut with a Leica Ultracut UCT ultramicrotome (Leica Microsystems Inc.), stained with uranyl acetate and lead citrate, and viewed on a JEOL 1200 EX transmission electron microscope (JEOL USA Inc.) equipped with an AMT 8 megapixel digital camera and AMT Image Capture Engine V602 software (Advanced Microscopy Techniques).
In-situ hybridization
RNAscope Multiplex Fluorescent V2 assay (ACDBio, Cat. No. 323100) was performed according to the manufacturer’s instructions. Briefly, slides with ice cold 97% methanol/3% acidic acid-fixed, paraffin-embedded eye sections (4 µM thick) were baked for 60’ at 60 °C before being deparaffinized in 2 changes of xylenes and dehydrated in two changes of 100% ethanol for 5’ each, then fully dried in a 60 °C oven, ~10’. Slides were then treated with RNAscope hydrogen peroxide solution for 10’ at room temperature and washed twice in distilled water prior to 15’ of antigen retrieval in 100 °C RNAscope target retrieval solution (ACDBio, Cat. No. 322000). After rinsing in distilled water, slides were dried in 100% Ethanol and placed in a 60 °C oven for 5’. Barriers were drawn around tissues using an ImmEdge hydrophobic Pen (Vector Labs, Cat. No. H-4000), and then slides were allowed to fully dry. All incubations were performed in a HybEZ oven (ACDBio, Cat. No. 241000ACD) at 40 °C. First, RNAscope Protease II solution was added to each slide for 30’. After 2 washes in nuclease-free water, probes were applied for 2 hr. MM-S1pr3 (ACDBIO, Cat. No. 435951), Mm-PPIB positive control (Cat. No. 313911) or negative control probes (Cat. No. 320871) were utilized on sequential sections from each eye. Following the kit’s 3 amplification solution incubations at 37 °C and washes in RNAscope wash buffer (diluted to 1x in nuclease-free water), HRP-C1 solution was applied for 15’ at 40 °C, followed by 2 changes of wash buffer and application of Opal 520 (Akoya Biosciences, Cat. No. FP1478001KT) diluted 1:1500 in TSA buffer for 30’ at 40 °C. Slides were washed, nuclei were stained DAPI for 10’ at room temp, washed in wash buffer two times and cover slipped using FluoroSave Reagent (Millipore-Sigma, Cat. No. 345789).
Cell culture
ARPE-19 (CAT#CRL-2302) was purchased from American Type Culture Collection (Manassas, VA, USA) and used for experiments. Dulbecco’s Modified Eagle’s Medium/F12 (Sigma-Aldrich) containing 1% penicillin/streptomycin (Sigma-Aldrich) and 10% fetal bovine serum was used for culture medium. Medium was changed every 2 days. Cells in the range of passages 3–16 were used for studies. All experiments were performed after serum starvation.
Preparation of ApoM-S1P
S1P was obtained from Enzo Life Sciences, inc. (Exeter, UK), and dissolved in methanol at 0.5 mg/mL. Before use in experiments, the methanol was evaporated using nitrogen gas. Human recombinant ApoM was obtained from R&D Systems (Minneapolis, MN, USA) and combined to create the ApoM-S1P complex as previously described42. S1P was dissolved in ApoM, followed by 45 minutes of incubation at room temperature.
Preparation of FITC labeled POS
POS were labeled with FITC as previously described55. Briefly, POS were incubated with fluorescein-t-isothiocyanate (FITC ‘Isomer I’) from ThermoFisher Scientific (Waltham, MA, USA) for 1 hour and washed thoroughly with PBS.
Treatment of ARPE-19 and ex vivo eyecups
To challenge RPE cells with photoreceptor outer segments, POS were obtained from InVision BioResources (Seattle, WA, USA). For ARPE-19, cells were allowed to adhere overnight in chamber slides from Ibidi (Germany). Media was exchanged for POS rich media at a 10:1 or 20:1 POS to RPE ratio as described previously55. Cells were incubated for 4 hours at 37 °C in a humidified cell culture incubator with 5% CO2. After incubation, ApoM-S1P that was previously prepared was added and incubated for 1 hour at 37 °C in a humidified cell culture incubation with 5% CO2 after three washes with PBS. Cells were then washed thrice with PBS, fixed with 4% paraformaldehyde for 20 minutes at room temperature, and processed for analysis. For ex vivo eyecups, mice were first sacrificed and enucleated. Eyes were carefully dissected to remove the cornea, lens, and retina. The remaining eyecup was placed in a 96-well U-bottom plate from Corning (Corning, NY, USA) with either control DMEM/F12 or media enriched with POS-FITC. The plate was then incubated for 2 hours at 37 °C in a humidified cell culture incubator with 5% CO2. After incubation, ApoM-S1P that was previously prepared was added and incubated for 1 hour at 37 °C in a humidified cell culture incubation with 5% CO2 after three washes with PBS. After three more PBS washes, eyecups were fixed for 20 minutes with 4% paraformaldehyde at room temperature. Eyecups were then immunohistologically stained and mounted onto a glass slide for imaging. To test for the effects of lipophagy inhibition, ARPE19 cells were seeded in 12-well chamber slides precoated with 1% Gelatin solution (Cell Biologics, Cat. No. 6950) to aid adherence and maintained at 37 °C with 5% CO2. Cells were serum-starved overnight to remove exogenous sources of lipid. The next day, they were washed in DPBS and treated with bovine photoreceptor outer segments (POS) at 0, 10, or 20x ratio of POS:ARPE19 cells for 4 hr in serum-free media. Cells were washed in multiple changes of DPBS to remove POS followed by treatment with prepared ApoM-S1P (as described previously herein) and either DMSO (vehicle/control) or 30 µM Lalistat 2 (Axon Medchem, Cat. No. 2797) for 72 hr. Slides were the washed in DPBS, fixed for 20 min at room temperature in prepared methanol-free 4% paraformaldehyde in PBS (Electron Microscopy Sciences, Cat. No. 15710) and stained with BODIPY, Alexfluor 594-conjugated phalloidin and DAPI as described herein. Images were acquired using an Olympus FV1000 confocal with a BX61-WI microscope and PlanApo N 60x TIRF Oil-immersion objective lens (1.45 N.A.) utilizing Fluoview software.
Immunohistochemistry
After fixing either ARPE-19 or eyecups, cells were stained with 1:500 DAPI (ThermoFisher Scientific), 1:250 phalloidin-iFluor 594 (Abcam), and 1:250 BODIPY 493/503 (ThermoFisher Scientific) in PBS with 0.3% triton-X100 (Sigma-Aldrich) for 20 minutes at room temperature. Cells were then washed thrice with PBS before mounting and imaging. BODIPY fluorescence was quantified by ImageJ software through the RGB measure plugin.
Cholesterol efflux assay
Cholesterol efflux of ARPE-19 cells with the addition of ApoM-S1P was assessed using the cholesterol efflux assay kit (ab196985) from Abcam (Cambridge, UK) according to the manufacturer’s protocol. Briefly, ARPE-19 cells were allowed to adhere overnight in a 96-well tissue culture plate. Cells were loaded with fluorescently labeled cholesterol before being treated with a cholesterol acceptor. Serum from ApoMKO mice was prepared as a cholesterol acceptor, so cells treated with ApoM-S1P had the complex mixed in with serum from ApoMKO mice. Fluorescence intensity of the supernatant and cell lysates was assessed with a microplate reader to then calculate a percentage of cholesterol efflux.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
All data from publicly available datasets analyzed are included in this published article (DOI: 10.1111/jcmm.16569) and the Gene Expression Omnibus (https://www.ncbi.nlm.nih.gov/geo/) through accession number GSE159435. Source data are provided with this paper. Any data supporting the findings from the study will be made readily available from the corresponding author upon request. Source data are provided with this paper.
References
Apte, R. S. Age-related macular degeneration. N. Engl. J. Med 385, 539–547 (2021).
Wong, W. L. et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob. Health 2, e106–e116 (2014).
Rein, D. B. et al. Prevalence of age-related macular degeneration in the US in 2019. JAMA Ophthalmol. 140, 1202–1208 (2022).
Sene, A. et al. Impaired cholesterol efflux in senescent macrophages promotes age-related macular degeneration. Cell Metab. 17, 549–561 (2013).
Curcio, C. A. Antecedents of Soft Drusen, the specific deposits of age-related macular degeneration, in the biology of human Macula. Invest Ophthalmol. Vis. Sci. 59, AMD182–AMD194 (2018).
Ferris, F. L. III, Fine, S. L. & Hyman, L. Age-related macular degeneration and blindness due to neovascular maculopathy. Arch. Ophthalmol. 102, 1640–1642 (1984).
Apte, R. S. Targeting tissue lipids in age-related macular degeneration. EBioMedicine 5, 26–27 (2016).
Apte, R. S., Chen, D. S. & Ferrara, N. VEGF in signaling and disease: beyond discovery and development. Cell 176, 1248–1264 (2019).
The Age-Related Eye Disease Study 2 (AREDS2) Research Group* Lutein + Zeaxanthin and Omega-3 fatty acids for age-related macular degeneration: The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 309, 2005–2015 (2013).
Yang, S., Zhao, J. & Sun, X. Resistance to anti-VEGF therapy in neovascular age-related macular degeneration: a comprehensive review. Drug Des. Dev. Ther. 10, 1857–1867 (2016).
Vishwakarma, S. & Kaur, I. Molecular mediators and regulators of retinal angiogenesis. Semin. Ophthalmol. 38, 124–133 (2023).
Khachigian, L. M., Liew, G., Teo, K. Y. C., Wong, T. Y. & Mitchell, P. Emerging therapeutic strategies for unmet need in neovascular age-related macular degeneration. J. Transl. Med. 21, 133 (2023).
Liao, D. S. et al. Complement C3 inhibitor Pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized Phase 2 trial. Ophthalmology 127, 186–195 (2020).
Wilke, G. A. & Apte, R. S. Complement regulation in the eye: implications for age-related macular degeneration. J. Clin. Invest. 134, e178296.
Cheung, C. M. G. et al. Plasma lipoprotein subfraction concentrations are associated with lipid metabolism and age-related macular degeneration. J. Lipid Res. 58, 1785–1796 (2017).
Danis, R. P., Lavine, J. A. & Domalpally, A. Geographic atrophy in patients with advanced dry age-related macular degeneration: current challenges and future prospects. Clin. Ophthalmol. 9, 2159–2174 (2015).
Handa, J. T. et al. A systems biology approach towards understanding and treating non-neovascular age-related macular degeneration. Nat. Commun. 10, 3347 (2019).
Malek, G., Li, C.-M., Guidry, C., Medeiros, N. E. & Curcio, C. A. Apolipoprotein B in cholesterol-containing drusen and basal deposits of human eyes with age-related maculopathy. Am. J. Pathol. 162, 413–425 (2003).
Martin, S. S. et al. Comparison of high-density lipoprotein cholesterol to Apolipoprotein A-I and A-II to predict coronary calcium and the effect of insulin resistance. Am. J. Cardiol. 107, 393–398 (2011).
Shen, L. L. et al. Associations of systemic health and medication use with the enlargement rate of geographic atrophy in age-related macular degeneration. Br. J. Ophthalmol. 107, 261–266 (2023).
Winkler, T. W. et al. Genome-wide association meta-analysis for early age-related macular degeneration highlights novel loci and insights for advanced disease. BMC Med Genom.13, 120 (2020).
Strunz, T., Kiel, C., Sauerbeck, B. L. & Weber, B. H. F. Learning from fifteen years of genome-wide association studies in age-related macular degeneration. Cells 9, 2267 (2020).
Landowski, M. & Bowes Rickman, C. Targeting lipid metabolism for the treatment of age-related macular degeneration: insights from preclinical mouse models. J. Ocul. Pharm. Ther. 38, 3–32 (2022).
Kelly, U. L. et al. High-density lipoproteins are a potential therapeutic target for age-related macular degeneration. J. Biol. Chem. 295, 13601–13616 (2020).
Rudolf, M. et al. Sub-retinal drusenoid deposits in human retina: Organization and composition. Exp. Eye Res. 87, 402–408 (2008).
Ban, N. et al. Disrupted cholesterol metabolism promotes age-related photoreceptor neurodegeneration. J. Lipid Res. jlr.M084442 https://doi.org/10.1194/jlr.M084442. (2018).
Storti, F. et al. Impaired ABCA1/ABCG1-mediated lipid efflux in the mouse retinal pigment epithelium (RPE) leads to retinal degeneration. eLife 8, e45100.
Ban, N. et al. Impaired monocyte cholesterol clearance initiates age-related retinal degeneration and vision loss. JCI Insight 3, e120824 (2018).
Terao, R. et al. LXR/CD38 activation drives cholesterol-induced macrophage senescence and neurodegeneration via NAD+ depletion. Cell Rep. 114102 https://doi.org/10.1016/j.celrep.2024.114102. (2024).
Wolfrum, C., Poy, M. N. & Stoffel, M. Apolipoprotein M is required for preβ-HDL formation and cholesterol efflux to HDL and protects against atherosclerosis. Nat. Med 11, 418–422 (2005).
Ding, B.-S. et al. Aging Suppresses Sphingosine-1-Phosphate Chaperone ApoM in circulation resulting in maladaptive organ repair. Dev. Cell 53, 677–690.e4 (2020).
Christoffersen, C. et al. Endothelium-protective sphingosine-1-phosphate provided by HDL-associated apolipoprotein M. Proc. Natl. Acad. Sci. USA 108, 9613–9618 (2011).
Christoffersen, C. et al. Isolation and characterization of human apolipoprotein M-containing lipoproteins. J. Lipid Res. 47, 1833–1843 (2006).
Xu, N. & Dahlbäck, B. A Novel Human Apolipoprotein (apoM)*. J. Biol. Chem. 274, 31286–31290 (1999).
Liu, M. et al. Hepatic Apolipoprotein M (ApoM) overexpression stimulates formation of larger ApoM/Sphingosine 1-Phosphate-enriched plasma high density Lipoprotein. J. Biol. Chem. 289, 2801–2814 (2014).
Elsøe, S. et al. Apolipoprotein M binds oxidized phospholipids and increases the antioxidant effect of HDL. Atherosclerosis 221, 91–97 (2012).
Christoffersen, C. et al. Effect of Apolipoprotein M on high density lipoprotein metabolism and atherosclerosis in low density lipoprotein receptor knock-out mice*. J. Biol. Chem. 283, 1839–1847 (2008).
Christensen, P. M. et al. Impaired endothelial barrier function in apolipoprotein M–deficient mice is dependent on sphingosine-1-phosphate receptor 1. FASEB J. 30, 2351–2359 (2016).
Ruiz, M., Okada, H. & Dahlbäck, B. HDL-associated ApoM is anti-apoptotic by delivering sphingosine 1-phosphate to S1P1 & S1P3 receptors on vascular endothelium. Lipids Health Dis. 16, 36 (2017).
Guo, Z. et al. Apolipoprotein M attenuates anthracycline cardiotoxicity and lysosomal injury. JACC Basic Transl. Sci. 8, 340–355 (2023).
Terao, R. et al. The role of sphingosine 1-phosphate receptors on retinal pigment epithelial cells barrier function and angiogenic effects. Prostaglandins Other Lipid Mediat.145, 106365 (2019).
Terao, R., Honjo, M. & Aihara, M. Apolipoprotein M inhibits angiogenic and inflammatory response by Sphingosine 1-Phosphate on retinal pigment epithelium cells. Int J. Mol. Sci. 19, 112 (2017).
Vaidya, M. et al. Regulation of ABCA1-mediated cholesterol efflux by sphingosine-1-phosphate signaling in macrophages. J. Lipid Res. 60, 506–515 (2019).
Raposo, G. & Marks, M. S. The dark side of lysosome-related organelles: specialization of the endocytic pathway for melanosome biogenesis. Traffic 3, 237–248 (2002).
Schraermeyer, U., Peters, S., Thumann, G., Kociok, N. & Heimann, K. Melanin granules of retinal pigment epithelium are connected with the lysosomal degradation pathway. Exp. Eye Res. 68, 237–245 (1999).
Kim, I. T. & Choi, J. B. Melanosomes of retinal pigment epithelium-distribution, shape, and acid phosphatase activity. Korean J. Ophthalmol. 12, 85–91 (1998).
Chirinos, J. A. et al. Reduced Apolipoprotein M and adverse outcomes across the spectrum of human heart failure. Circulation 141, 1463–1476 (2020).
Bosteen, M. H., Dahlbäck, B., Nielsen, L. B. & Christoffersen, C. Protein unfolding allows use of commercial antibodies in an apolipoprotein M sandwich ELISA. J. Lipid Res 56, 754–759 (2015).
Tsin, A., Betts-Obregon, B. & Grigsby, J. Visual cycle proteins: Structure, function, and roles in human retinal disease. J. Biol. Chem. 293, 13016–13021 (2018).
Lee, T. J. et al. Catalytic isoforms of AMP-activated protein kinase differentially regulate IMPDH activity and photoreceptor neuron function. JCI Insight https://doi.org/10.1172/jci.insight.173707. (2024).
Butler, J. M., Supharattanasitthi, W., Yang, Y. C. & Paraoan, L. RNA-seq analysis of ageing human retinal pigment epithelium: Unexpected up-regulation of visual cycle gene transcription. J. Cell Mol. Med. 25, 5572–5585 (2021).
Goldberg, A. F. X., Moritz, O. L. & Williams, D. S. Molecular basis for photoreceptor outer segment architecture. Prog. Retin. Eye Res. 55, 52–81 (2016).
Albert, A., Alexander, D. & Boesze-Battaglia, K. Cholesterol in the rod outer segment: A complex role in a “simple” system. Chem. Phys. Lipids 199, 94–105 (2016).
Storti, F. et al. Regulated efflux of photoreceptor outer segment-derived cholesterol by human RPE cells. Exp. Eye Res. 165, 65–77 (2017).
Mazzoni, F., Mao, Y. & Finnemann, S. C. Advanced analysis of photoreceptor outer segment phagocytosis by RPE cells in culture. Methods Mol. Biol. 1834, 95–108 (2019).
Yako, T., Otsu, W., Nakamura, S., Shimazawa, M. & Hara, H. Lipid droplet accumulation promotes RPE dysfunction. Int J. Mol. Sci. 23, 1790 (2022).
Rosario, F.-G., Garland, D. L. & Pierce, E. A. Isolation, culture and characterization of primary mouse RPE cells. Nat. Protoc. 11, 1206–1218 (2016).
Zhang, S. et al. The regulation, function, and role of lipophagy, a form of selective autophagy, in metabolic disorders. Cell Death Dis. 13, 132 (2022).
Du, H., Duanmu, M., Witte, D. & Grabowski, G. A. Targeted disruption of the mouse lysosomal acid lipase gene: long-term survival with massive cholesteryl ester and triglyceride storage. Hum. Mol. Genet. 7, 1347–1354 (1998).
Leopold, C. et al. Hepatocyte-specific lysosomal acid lipase deficiency protects mice from diet-induced obesity but promotes hepatic inflammation. Biochim. et. Biophys. Acta (BBA) - Mol. Cell Biol. Lipids 1864, 500–511 (2019).
Nolan, N. D., Jenny, L. A., Wang, N.-K. & Tsang, S. H. Retinal pigment epithelium lipid metabolic demands and therapeutic restoration. Taiwan J. Ophthalmol. 11, 216–220 (2021).
Kono, M. et al. The Sphingosine-1-phosphate Receptors S1P1, S1P2, and S1P3 Function Coordinately during Embryonic Angiogenesis *. J. Biol. Chem. 279, 29367–29373 (2004).
Allende, M. L., Yamashita, T. & Proia, R. L. G-protein-coupled receptor S1P1 acts within endothelial cells to regulate vascular maturation. Blood 102, 3665–3667 (2003).
Du, H. et al. Lysosomal acid lipase-deficient mice: depletion of white and brown fat, severe hepatosplenomegaly, and shortened life span. J. Lipid Res. 42, 489–500 (2001).
Xue, Y., Shen, S. Q., Corbo, J. C. & Kefalov, V. J. Circadian and light-driven regulation of rod dark adaptation. Sci. Rep. 5, (2015).
Lee, T. J. Mechanisms of rod photoreceptor metabolism and function in health and disease. Arts Sci. Electron. Theses Dissert. 3037. https://openscholarship.wustl.edu/art_sci_etds/3037. (2024).
Acknowledgements
This work was supported by National Institutes of Health (NIH) grants R01 EY019287 (RSA) and P30 EY02687 (Vision Core Grant); Jeffrey T. Fort Innovation Fund (RSA); Starr Foundation AMD Research Fund (RSA); Siteman Retina Research Fund (RSA); Carl Marshall and Mildred Almen Reeves Foundation (RSA); Retina Associates of St. Louis Research Fund (RSA); a pilot project grant from the Washington University Genome Technology Access Center (RSA); Research to Prevent Blindness/American Macular Degeneration Foundation Catalyst Award for Innovative Research Approaches for Age-Related Macular Degeneration (RSA) and an unrestricted grant from Research to Prevent Blindness to the John F. Hardesty, MD Department of Ophthalmology and Visual Sciences at Washington University School of Medicine in St. Louis. The authors thank the families of the generous tissue donors, the Mid-America Transplant Eye Bank for their collection of human tissue used in this study, and the Bright Center for Human Vision at WashU Medicine for the distribution of human tissue samples for research. TL was supported by NIH Training Grant (1T32GM1397740-1) and Vitreoretinal Surgery Foundation Fellowship (VGR0023118). AJ was supported by K08HL138262 and 1R01HL155344 from the NHLBI and by the Children’s Discovery Institute of Washington University and St. Louis Children’s Hospital (MC-FR-2020- 919), as well as the Diabetes Research Center at Washington University in St. Louis of the National Institutes of Health under award number P30DK020579, and the NIH grant P30DK056341 (Nutrition Obesity Research Center) and received support from the Longer Life Foundation. DK was supported by funding from the Austrian Science Fund (FWF) (SFB 10.55776/F73). The authors acknowledge Wandy L. Beatty, Molecular Microbiology Imaging Facility in Washington University School of Medicine, for electron microscopy analyses. This manuscript re-used the data and results from the thesis and dissertation of the first author, TJL, that have been previously published66.
Author information
Authors and Affiliations
Contributions
T.J.L., R.S.A. and A.J. designed and analyzed the experiments. T.J.L., A.S., K.P., C.V.P., R.T., Z.G., M.O. and C.C. conducted the experiments. D.K., C.C., A.J., and R.S.A. provided resources. T.J.L., R.S.A. and A.J. designed the methodology and wrote the manuscript. T.J.L., R.S.A. and A.J. conceptualized the study.
Corresponding authors
Ethics declarations
Competing interests
RSA and AJ have intellectual property applications licensed by Washington University to Mobius Scientific. RSA and AJ are on the advisory board of Mobius Scientific, and RSA is currently the CSO at Mobius Scientific. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Makoto Kurano, Yoko Ozawa, and the other anonymous reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, T.J., Santeford, A., Pitts, K.M. et al. Apolipoprotein M attenuates age-related macular degeneration phenotypes via sphingosine-1-phosphate signaling and lysosomal lipid catabolism. Nat Commun 16, 5331 (2025). https://doi.org/10.1038/s41467-025-60830-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-025-60830-1