Abstract
This study aimed to evaluate the glymphatic system activity in Parkinson’s disease (PD) with and without rapid eye movement sleep behavior disorder (RBD) using the diffusion tensor image analysis along the perivascular space (DTI-ALPS) methods. Overall, 91 patients with PD and 33 healthy controls were recruited. PD patients were divided into PD-RBD (n = 55) and PD-nRBD (n = 36) groups according to RBD scales. The ALPS-index and enlarged perivascular spaces (EPVS) scores were calculated. PD-RBD group exhibited lower ALPS-index than PD-nRBD and controls after controlling for the effect of age (p = 0.018 and p = 0.001). PD-RBD group showed higher UPDRS part I and HAMD score than those in PD-nRBD group. RBD symptom was independently correlated with ALPS-index in PD (β = −0.259, p = 0.014). In conclusion, PD with possible RBD correlated with more severe glymphatic system dysfunction and non-motor symptoms than those in PD without RBD.
Similar content being viewed by others
Introduction
Parkinson’s disease (PD) is a common neurodegenerative disease, which is characterized by the loss of dopaminergic neurons and the aggregation of misfolded α-synuclein (α-syn)1,2. Rapid eye movement (REM) sleep behavior disorder (RBD) is a specific clinical prodromal symptoms of PD, described as the loss of normal skeletal muscle atonia and manifested by prominent motor activity and dreaming. RBD is found in up to 50% of patients with PD, has a negative impact on the quality of life3. However, the underlying mechanism of PD with RBD is poorly understood.
Glymphatic system has been considered as the main pathway for the removal of abnormal proteins and metabolic waste in the brain4,5. Abnormal aggregates of α-syn protein are involved in both PD and RBD1,6. Hence, impairment of glymphatic system may lead to reduced clearance of α-syn and its consequent accumulation, which plays a critical role in the pathogenesis of PD7,8. Recently, a non-invasive method, diffusion tensor image analysis along the perivascular space (DTI-ALPS) has been used to assess the function of glymphatic system9. Our group was the second one to apply DTI-ALPS method in the field of PD10. Our findings showed that PD patients revealed lower ALPS-index than controls, especially in the late stage. In the early PD group, ALPS-index was significantly associated with MMSE score after controlling for multiple variables. While ALPS-index inversely associated with age in the late PD group. In addition, enlarged perivascular spaces (EPVS) on MRI also reflect lymphatic drainage channels dysfunction11. Our group supported a negative correlation between ALPS index and EPVS score in early PD group10. Subsequently, other studies provided evidences supporting that ALPS-index correlated with motor and non-motor symptoms in PD12,13,14,15,16. Recent studies also suggested that RBD patients exhibited lower DTI-ALPS-index than controls17,18. However, the effect of RBD symptom of glymphatic system in PD remained uninvestigated before.
Consequently, we expanded the sample size and investigated the impact of RBD symptom on glymphatic system using this noninvasive DTI-ALPS method. We also examined the difference in clinical variables between PD with and without RBD symptom. We hypothesized that RBD may correlate with more severe glymphatic system impairment and non-motor symptoms. This study highlights the relationship between RBD and glymphatic system in PD with respect to neuroimaging markers.
Methods
Participants and clinical assessment
In this study, patients with idiopathic PD (n = 91) and age- and sex-matched normal controls (NC) (n = 33) were recruited. All PD patients were diagnosed based on the 2015 Movement Disorder Society diagnostic criteria. Patients whose PD were induced by trauma, tumor, encephalitis, cerebrovascular disease, other neurodegenerative diseases (such as multiple system atrophy, progressive supranuclear palsy and dementia with Lewy bodies), medications, and poisoning were excluded. Patients who had moderate-to-severe obstructive sleep apnea hypopnea syndrome, night terror/sleepwalking, sleep-related epilepsy, nocturnal paroxysmal dystonia, secondary RBD caused by drugs (especially the use of selective serotonin reuptake inhibitor), and other sleep disorders associated with psychiatric, autoimmune and infectious neurological disorders were also excluded. All participants were right-handed Chinese natives. Clinical evaluation included Mini-Mental State Examination (MMSE), Unified Parkinson’s Disease Rating Scale (UPDRS) score, Hoehn and Yahr (HY) Stages, Hamilton Rating Scale for Depression (HAMD), Hamilton Rating Scale for Anxiety (HAMA). PD Patients undergoing anti-parkinsonian therapy were all examined in the clinically defined “ON” state. Neuropsychological scales were accomplished by one neurologist who was blinded to the clinical data. Our study was approved by a local ethics committee, and each participants signed an informed consent form before the study.
Patients with PD were divided into PD with (PD-RBD) and without possible RBD (PD-nRBD) two subgroups according to the International Classification of Sleep Minimum diagnostic criteria for RBD in Disorders Revised (ICSD⁃R)19 and the scale of the RBD Single-Question Screen (RBD1Q)20. PD with RBD patients had limb or body movement which is associated with dream mentation. In addition, at least one of the following occurs: harmful or potentially harmful sleep behaviors; dreams appear to be “acted out”; sleep behaviors disrupt sleep continuity19. All PD with RBD patients screened positive on the scale of RBD1Q, which showed good sensitivity (93.8%) and specificity (87.2%) in diagnosing RBD20. This questionnaire may reliably detect RBD, with psychometric properties favorably comparable to those reported for longer questionnaires. For the evaluation of the severity of clinical RBD, Stavanger Sleepiness Questionnaire (SSQ) was used based on previous studies21,22,23,24. SSQ was rated as follows: 0= physical and verbal behaviors are not present during sleep, 1 = mild physical restlessness and/or vocalizations, for example, talking, crying, or laughing, while sleep, 2 = moderate physical and verbal restlessness, for example, shouting, during sleep, tend to awake partner, 3 = severe physical, for example, hitting, may injure partner or him/herself, and verbal restlessness while asleep24. Moreover, according to the HY stages, PD patients were divided into early PD (HY 1-2) and advanced PD (HY 2.5-4) groups.
MR image acquisition
All participants were scanned using a 3.0 T MRI scanner (Philips, Achieva TX). Sequences included diffusion tensor imaging (TR/TE = 5472/93 ms; b = 1000 s/mm2, FOV = 24 cm × 24 cm, matrix=128 × 128, MPG = 31 directions, 3 mm slice thickness without slice gap), high-resolution T1-weighted 3D (repetition time/echo time (TR/TE) = 7.4/3 ms; flip angle (FA) = 8°; field of view (FOV) = 24 cm × 24 cm; and 1.2 mm slice thickness without slice gap), T2-weighted (T2WI, TR/TE = 2500/100 ms; FOV = 24 cm × 24 cm, 5 mm slice thickness, and 1.5 mm slice gap), and fluid-attenuated inversion recovery (FLAIR; TR/TE = 8000/140 ms; TI = 2400 ms; FOV = 24 cm × 24 cm, and 4 mm slice thickness without slice gap).
DTI-ALPS processing
DTI images were processed using DTI studio. The software creates images of the diffusion tensor, which consisted of a color-coded fractional anisotropy (FA) map and a diffusivity map. We used the DTI-ALPS processing method described by Taoka et al.9 group. On a color-coded FA map, we placed a 5-mm-diameter spherical region of interest (ROI) in the area of the projection and association fibers at the level of the lateral ventricle body in the left hemisphere. The diffusivity in the x-axis, y-axis, and z-axis directions was calculated on each image. ALPS-index is measured by the ratio of the average values of the x-axis diffusivity in the area of the projection fibers (Dxproj) and the x-axis diffusivity in the area of the association fibers (Dxassoc) to the average value of the y-axis diffusivity in the area of the projection fibers (Dyproj) and the z-axis diffusivity (Dzacoc) of the association fibers area, as shown below:
ALPS index = mean (Dxproj, Dxassoc)/mean (Dyproj, Dzassoc). We calculated ALPS-index in the left hemisphere since all the participants were right-handed. Lower ALPS-index represents the more severe glymphatic system dysfunction.
MRI-visible EPVS measurement
Enlarged perivascular spaces (EPVS) represent structural alteration of impaired glymphatic system, which were defined as punctate hyperintensities on T2WI at the same level of the lateral ventricle body, usually 1–3 mm in diameter25. We did not count isolated single large invaginations of cerebrospinal fluid round perforating vessels. EPVS in basal ganglia (BG) and centrum semiovale (CSO) were calculated in this study. EPVS were rated as follows: 0 = no EPVS, 1 = < 10 EPVS, 2 = 11–20 EPVS, 3 = 21–40 EPVS, and 4 = > 40 EPVS. If there was an asymmetry between the sides, the hemisphere most affected was calculated25. EPVS was counted by two trained radiologists who were blinded to the clinical data.
Statistical analysis
Statistical analyses were performed with Statistical Package for the Social Sciences (SPSS) 27.0 software. Two-sample t-test and Chi-square test were conducted to compare the differences between PD and NC, and between PD-RBD and PD-nRBD groups. Moreover, analysis of variance was conducted to compare differences between PD-RBD, PD-nRBD, and NC. Spearman correlation analysis was used to evaluate the bivariate associations between parameters. We conducted the partial correlation analysis and analysis of covariance (ANCOVA) were conducted to control confounding factors. Binary logistic regression analysis was performed to investigate the relationship between RBD symptom based on RBD1Q and other clinical variables. Multivariate linear regression analysis was also carried out to explore the correlation between the ALPS-index and other parameters in different groups. Multivariate ordered logistic regression analysis was performed between the SSQ score and other variables in PD. P < 0.05 was regarded as statistically significant.
Results
Clinical data and differences in ALPS-index between groups
Ninety-one PD patients and 33 normal controls (NC) were recruited in our study. Clinical data and imaging findings of the participants are presented in Table 1. PD patients showed lower ALPS-index compared to NC after controlling for the effect of age (F = 7.835, p = 0.006). In addition, there was significant difference in ALPS-index between PD-RBD, PD-nRBD, and NC after controlling for the effect of age (F = 6.970, p = 0.001). Post hoc analysis indicated that PD-RBD group revealed reduced ALPS-index than PD-nRBD group and NC (p = 0.018, p = 0.001, respectively). While there was no markedly difference in ALPS-index between PD-RBD group and NC (Fig. 1). These three groups differed in education years (p = 0.001), but did not differ in age, sex ratio, and MMSE score (all p > 0.05).
Furthermore, PD-RBD group exhibited higher UPDRS part I (p = 0.040) and HAMD score (p = 0.011) than those in PD-non RBD group (Table 1). There were no significant differences in age, sex ratio, MMSE score, education years, LED, disease duration, UPDRS part II, III, IV, and total score, H-Y stages, HAMA, BG-EPVS, and CSO-EPVS scores between two PD subgroups (all p > 0.05). SSQ score was correlated with UPDRS part I (rs = 0.306, p = 0.003), part II (rs = 0.257, p = 0.014), HAMD (rs = 0.345, p = 0.001), and HAMA scores (rs = 0.216, p = 0.040) in Spearman correlation analysis. However, there were no significant differences between SSQ and these variables above in multivariate ordered logistic regression analysis.
Correlations between ALPS-index and other parameters in PD
Spearman correlation analysis revealed that ALPS-index was negatively associated with increasing age (rs = −0.266, p = 0.011) and RBD symptom based on RBD1Q (rs = −0.228, p = 0.030). ALPS-index was not found to be related to sex ratio, education years, disease duration, LED, UPDRS score, RBD severity based on SSQ, MMSE, HAMD, HAMA, BG-EPVS, and CSO-EPVS score (all p > 0.05). In the partial correlation analysis, after controlling the effect of age, ALPS-index still correlated with RBD symptom based on RBD1Q (r = −0.251, p = 0.017), and did not relate to sex ratio, education, disease duration, LED, UPDRS score, RBD severity based on SSQ, MMSE, HAMD, HAMA, and EPVS scores (all p > 0.05). In multivariate linear regression analysis, increasing age (β = −0.288, p = 0.007) and RBD symptom (β = −0.259, p = 0.014) were correlated with ALPS-index in PD patients. While ALPS-index did not relate to other clinical parameters in PD group (all p > 0.05).
Correlations between RBD symptom and other parameters in PD
In PD group, RBD symptom based on RBD1Q was related with higher UPDRS part I (rs = 0.298, p = 0.004) and HAMD score (rs = 0.308, p = 0.003), and lower ALPS-index (rs = −0.228, p = 0.030) in Spearman correlation analysis. Binary logistic regression revealed that RBD symptom based on RBD1Q was associated with lower ALPS-index (OR = 0.024, 95% CI 0.001–0.660, p = 0.027) and higher UPDRS part II score (OR = 1.134, 95% CI 1.02–1.26, p = 0.016). RBD severity based on SSQ did not show any significant correlations with the clinical and neuroimaging parameters.
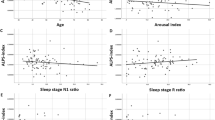
Correlations between ALPS-index and other parameters in PD-RBD and PD-nRBD group
In PD-RBD group, ALPS-index was negatively correlated with age (rs = −0.379, p = 0.004), and CSO-EPVS score (rs = −0.307, p = 0.023) (Fig. 2). In the partial correlation analysis, after controlling the effect of age, ALPS-index was still associated with CSO-EPVS score (r = −0.315, p = 0.020). While in PD-nRBD group, there were no markedly association between ALPS-index and clinical variables and EPVS scores (all p > 0.05).
Spearman correlation showed that ALPS-index was negatively correlated with age (rs = −0.379, p = 0.004) (a), and negatively related with CSO-EPVS score (rs = −0.307, p = 0.023) (b) in PD-RBD group. While these correlations were not significant in PD-nRBD group. PD-RBD PD with rapid eye movement sleep behavior disorder, PD-nRBD PD without rapid eye movement sleep behavior disorder, ALPS-index along the perivascular space-index, CSO-EPVS enlarged perivascular spaces in centrum semiovale.
Correlations between ALPS-index, RBD symptom, and other parameters in early and advanced PD
In early PD group (HY 1-2, n = 45), there were no significant differences in age, sex ratio, MMSE, education, disease duration, LED, UPDRS scores, H-Y stages, HAMD, HAMA, and EPVS scores between PD with and without RBD subgroups. No significant correlations between ALPS-index and clinical parameters, and between RBD symptoms and other parameters were found (all p > 0.05). In advanced PD group (HY 2.5–4, n = 46), PD-RBD patients showed lower ALPS-index (p = 0.036), higher UPDRS part I (p = 0.005), UPDRS total (p = 0.013), and HAMD score (p = 0.036) than those in PD-nRBD patients (Fig. 3). RBD symptom negatively associated with ALPS-index (p = 0.031), and positively correlated with UPDRS part I (p = 0.001), II (p = 0.036), total(p = 0.014), and HAMD score (p = 0.018) in the advanced PD group. Binary logistic regression showed that RBD symptom was associated with lower ALPS-index (OR = 0.013, 95% CI 0.000–0.967, p = 0.048) and higher UPDRS part I score (OR = 1.699, 95% CI 1.128–2.560, p = 0.011).
Discussion
In this study, we firstly provided evidences supporting the differences in ALPS-index between PD with and without RBD groups, after controlling for the effect of age. ALPS-index was negatively associated with RBD symptom in PD after controlling multiple variables. PD-RBD group exhibited higher UPDRS part I, II, total and HAMD score than those in PD-nRBD group. These correlations were more obvious in the advanced stage in PD, rather than in the early stage. In PD-RBD group, there were markedly correlations between ALPS-index and age, as well as CSO-EPVS score. Our findings provided evidence supporting the involvement of glymphatic system in the pathogenesis of PD with RBD.
Previous studies have investigated the relationships between ALPS-index and clinical variables in PD, including age, disease duration, disease severity, motor symptoms, cognitive impairment, FOG, and sleep12,26,27,28. Reduced ALPS-index may become a promising imaging biomarkers for predicting PD motor and cognitive function progression13,14. However, it has not been established as to whether glymphatic system dysfunction plays a vital role in PD with RBD. No significant difference in ALPS-index between PD with and without RBD was observed before18.
Recently, the relationship between glymphatic system and RBD has also received attention. There were some studies indicating that isolated RBD patients had lower ALPS index than controls17,18. Moreover, ALPS-index was significantly decreased in PD patients compared with RBD patients. However, the differences between PD and RBD is still controversial and limited29. In PD with RBD group, there was a negative relationship between ALPS-index and UPDRS III score. While in PD without RBD group, this association was not significant18. Our study firstly demonstrated that PD with RBD related with more severe glymphatic system dysfunction. PD with RBD also correlated with non-motor symptoms. Furthermore, the associations between impairment of glymphatic system and more severe disease severity and higher CSO-EPVS score were observed in the PD-RBD group. We hypothesized that there may be PD-RBD and PD-nRBD two subtypes. PD-RBD group showed more non-motor symptoms compared with PD-nRBD group, especially in the advanced stage.
Horsager et al. have proposed that PD comprised two subtypes, brain-first and body-first subtypes30. Premotor RBD has proven to be a predictive marker of the body-first subtype. The body-first subtype revealed a faster disease progression in motor dysfunction than those in the brain-first subtype31. Some patients in our study could not accurately recall the onset time of RBD, so they could not be strictly divided into brain-first and body-first subtypes. While our findings suggested that there may be two different subtypes in PD with respect to RBD symptom to some extent. Previous study suggested that glymphatic function may mediate the pathological role of toxic protein in cognitive decline of PD14. Similarly, we speculate that PD-RBD subtype exhibits more obvious reduced glymphatic activity, which will result in the decreasing clearance and increasing accumulation of the misfolding proteins such as α-syn, and eventually lead to worse non-motor symptoms. In addition, our findings supported that both ALPS-index and EPVS represented dysfunction of glymphatic system, and could be applied in the future study. This result is also consistent with our previous work10. ALPS-index and EPVS represent the glymphatic system from abnormal protein clearance ability and structural alteration aspects.
In addition, we calculated ALPS-index in the left hemisphere, not bilaterally, since all the participants were right-handed. Most previous studies chose left hemisphere to measure ALPS-index12,15,18,26,32,33. While there were some studies analyzing bilateral hemispheres separately16,28, or counted the mean value of ALPS-index from both sides13,14,27. There were no significant differences in the DTI-ALPS index between the left and right hemispheres in PD16. Moreover, some researchers speculated that the left hemisphere was more prone to aging-related alterations in PD28. Therefore, we believe that the value of ALPS-index in the left hemisphere could represent the function of glymphatic system.
Some limitations should be considered in this study. (1) The patients in PD-RBD groups did not undergo laboratory-based polysomnography (PSG). (2) We did not take pathological markers and aquaporin-4 (AQP4) levels and polarity into account. We plan to explore the relationship between glymphatic system, PD and RBD from the perspective of pathological markers, AQP4 levels, and polarity in the future. Animal experiments are also needed. It will make us better understand the effect of RBD in the mechanism of PD. (3) There is an overlap between the ALPS-index of PD and controls, and between different PD subgroups. This non-invasive method could not be used on an individual level to date. Larger sample size, multi-center, and longitudinal studies are warranted in the future. (4) The mean age of PD-RBD patients showed slightly higher than that of PD-nRBD patients, which did not reach statistical significance. Although we tried to use the partial correlation analysis to control the effect of age, caution is still warranted regarding their conclusion. (5) The timing of RBD onset relative to PD is crucial. However, some patients in our study could not accurately recall the onset time of RBD. We did not analyze the association between RBD duration and ALPS-index.
In conclusion, we provided neuroimaging evidence of glymphatic system dysfunction in PD with symptomatic RBD. PD with RBD patients correlated with more severe glymphatic system dysfunction, disease severity, and non-motor symptoms than those in PD without RBD patients. Studies combing pathological markers, AQP4, and glymphatic system function in PD with RBD are warranted in the future.
Data availability
Clinical and neuroimaging data can be shared on reasonable requests by contacting the corresponding authors.
References
George, S., Rey, N. L., Reichenbach, N., Steiner, J. A. & Brundin, P. alpha-Synuclein: the long distance runner. Brain Pathol. 23, 350–357 (2013).
Poewe, W. et al. Parkinson disease. Nat. Rev. Dis. Prim. 3, 17013 (2017).
De Almeida, C. M. O., Pachito, D. V., Sobreira-Neto, M. A., Tumas, V. & Eckeli, A. L. Pharmacological treatment for REM sleep behavior disorder in Parkinson disease and related conditions: a scoping review. J. Neurol. Sci. 393, 63–68 (2018).
Iliff, J. J. et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci. Transl. Med. 4, 147ra111 (2012).
Nakada, T., Kwee, I. L., Igarashi, H. & Suzuki, Y. Aquaporin-4 functionality and virchow-robin space water dynamics: physiological model for neurovascular coupling and glymphatic flow. Int. J. Mol. Sci. 18, 1798 (2017).
Miglis, M. G. et al. Biomarkers of conversion to alpha-synucleinopathy in isolated rapid-eye-movement sleep behaviour disorder. Lancet Neurol. 20, 671–684 (2021).
Buccellato, F. R., D’Anca, M., Serpente, M., Arighi, A. & Galimberti, D. The role of glymphatic system in Alzheimer’s and Parkinson’s disease pathogenesis. Biomedicines 10, 2261 (2022).
Si, X. et al. Matrix metalloproteinase-9 inhibition prevents aquaporin-4 depolarization-mediated glymphatic dysfunction in Parkinson’s disease. J. Adv. Res. 56, 125–136 (2024).
Taoka, T. et al. Evaluation of glymphatic system activity with the diffusion MR technique: diffusion tensor image analysis along the perivascular space (DTI-ALPS) in Alzheimer’s disease cases. Jpn J. Radio. 35, 172–178 (2017).
Ma, X. et al. Diffusion tensor imaging along the perivascular space index in different stages of Parkinson’s disease. Front. Aging Neurosci. 13, 773951 (2021).
Wardlaw, J. M. et al. Perivascular spaces in the brain: anatomy, physiology and pathology. Nat. Rev. Neurol. 16, 137–153 (2020).
Bae, Y. J. et al. Glymphatic function assessment in Parkinson’s disease using diffusion tensor image analysis along the perivascular space. Park. Relat. Disord. 114, 105767 (2023).
He, P. et al. Motor progression phenotypes in early-stage Parkinson’s disease: a clinical prediction model and the role of glymphatic system imaging biomarkers. Neurosci. Lett. 814, 137435 (2023).
He, P. et al. The association of the glymphatic function with Parkinson’s disease symptoms: neuroimaging evidence from longitudinal and cross-sectional studies. Ann. Neurol. 94, 672–683 (2023).
Qin, Y. et al. Neuroimaging uncovers distinct relationships of glymphatic dysfunction and motor symptoms in Parkinson’s disease. J. Neurol. 270, 2649–2658 (2023).
Meng, J. C. et al. Correlation of glymphatic system abnormalities with Parkinson’s disease progression: a clinical study based on non-invasive fMRI. J. Neurol. 271, 457–471 (2024).
Lee, D. A., Lee, H. J. & Park, K. M. Glymphatic dysfunction in isolated REM sleep behavior disorder. Acta Neurol. Scand. 145, 464–470 (2022).
Si, X. et al. Neuroimaging evidence of glymphatic system dysfunction in possible REM sleep behavior disorder and Parkinson’s disease. NPJ Park. Dis. 8, 54 (2022).
Vignatelli, L. et al. Interobserver reliability of ICSD-R minimal diagnostic criteria for the parasomnias. J. Neurol. 252, 712–717 (2005).
Postuma, R. B. et al. A single-question screen for rapid eye movement sleep behavior disorder: a multicenter validation study. Mov. Disord. 27, 913–916 (2012).
Gjerstad, M. D., Alves, G., Wentzel-Larsen, T., Aarsland, D. & Larsen, J. P. Excessive daytime sleepiness in Parkinson disease: is it the drugs or the disease?. Neurology 67, 853–858 (2006).
Aygun, D., Turkel, Y., Onar, M. K. & Sunter, T. Clinical REM sleep behavior disorder and motor subtypes in Parkinson’s disease: a questionnaire-based study. Clin. Neurol. Neurosurg. 119, 54–58 (2014).
Gjerstad, M. D., Boeve, B., Wentzel-Larsen, T., Aarsland, D. & Larsen, J. P. Occurrence and clinical correlates of REM sleep behaviour disorder in patients with Parkinson’s disease over time. J. Neurol. Neurosurg. Psychiatry 79, 387–391 (2008).
Marras, C., Rochon, P. & Lang, A. E. Predicting motor decline and disability in Parkinson disease: a systematic review. Arch. Neurol. 59, 1724–1728 (2002).
Doubal, F. N., MacLullich, A. M., Ferguson, K. J., Dennis, M. S. & Wardlaw, J. M. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke 41, 450–454 (2010).
Ruan, X. et al. Diffusion tensor imaging analysis along the perivascular space index in primary Parkinson’s disease patients with and without freezing of gait. Neuroscience 506, 51–57 (2022).
Cai, X. et al. Diffusion along perivascular spaces provides evidence interlinking compromised glymphatic function with aging in Parkinson’s disease. CNS Neurosci. Ther. 29, 111–121 (2023).
Shen, T. et al. Diffusion along perivascular spaces as marker for impairment of glymphatic system in Parkinson’s disease. NPJ Park. Dis. 8, 174 (2022).
Bae, Y. J. et al. Altered brain glymphatic flow at diffusion-tensor MRI in rapid eye movement sleep behavior disorder. Radiology 307, e221848 (2023).
Horsager, J. et al. Brain-first versus body-first Parkinson’s disease: a multimodal imaging case-control study. Brain 143, 3077–3088 (2020).
Xu, Z. et al. Disease progression in proposed brain-first and body-first Parkinson’s disease subtypes. NPJ Park. Dis. 10, 111 (2024).
Gu, L. et al. Noninvasive neuroimaging provides evidence for deterioration of the glymphatic system in Parkinson’s disease relative to essential tremor. Park. Relat. Disord. 107, 105254 (2023).
Chen, H. L. et al. Associations among cognitive functions, plasma DNA, and diffusion tensor image along the perivascular space (DTI-ALPS) in patients with Parkinson’s disease. Oxidative Med. Cell. Longev. 2021, 4034509 (2021).
Acknowledgements
We are grateful to all the patients who participated in this study. This study was supported by the fund of National Multi-disciplinary Cooperative Diagnosis and Treatment Capacity Project for Major Disease from the National Health Commission of the People’s Republic of China (FTJ-19-03).
Author information
Authors and Affiliations
Contributions
M.X.X., C.H.B. and S.W. contributed to conception and design of the study. M.X.X., L.Y.Y. and X.M.X. collected the clinical data, organized the database, and performed the statistical analysis. L.C.M. L.X.Y. and S.D.D. collected the neuroimaging data and conducted the analysis. M.X.X. wrote the first draft of the manuscript. C.M. C.H.B. and S.W. revised the manuscript. All authors approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, X., Liu, Y., Xie, M. et al. Parkinson’s disease with possible REM sleep behavior disorder correlated with more severe glymphatic system dysfunction. npj Parkinsons Dis. 11, 82 (2025). https://doi.org/10.1038/s41531-025-00962-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-025-00962-9