Abstract
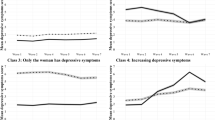
Depression represents a significant global public health challenge, and marital status has been recognized as a potential risk factor. However, previous investigations of this association have primarily focused on Western samples with substantial heterogeneity. Our study aimed to examine the association between marital status and depressive symptoms across countries with diverse cultural backgrounds using a large-scale, two-stage, cross-country analysis. We used nationally representative, de-identified individual-level data from seven countries, including the USA, the UK, Mexico, Ireland, Korea, China and Indonesia (106,556 cross-sectional and 20,865 longitudinal participants), representing approximately 541 million adults. The follow-up duration ranged from 4 to 18 years. Our analysis revealed that unmarried individuals had a higher risk of depressive symptoms than their married counterparts across all countries (pooled odds ratio, 1.86; 95% confidence interval (CI), 1.61–2.14). However, the magnitude of this risk was influenced by country, sex and education level, with greater risk in Western versus Eastern countries (β = 0.36; 95% CI, 0.16–0.56; P < 0.001), among males versus females (β = 0.25; 95% CI, 0.003–0.47; P = 0.047) and among those with higher versus lower educational attainment (β2 = 0.34; 95% CI, 0.11–0.56; P = 0.003). Furthermore, alcohol drinking causally mediated increased later depressive symptom risk among widowed, divorced/separated and single Chinese, Korean and Mexican participants (all P < 0.001). Similarly, smoking was as identified as a causal mediator among single individuals in China and Mexico, and the results remained unchanged in the bootstrap resampling validation and the sensitivity analyses. Our cross-country analysis suggests that unmarried individuals may be at greater risk of depression, and any efforts to mitigate this risk should consider the roles of cultural context, sex, educational attainment and substance use.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
27,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
118,99 € per year
only 9,92 € per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data from the NHANES are available at https://www.cdc.gov/nchs/nhanes/index.htm. Data from the WLS are available on the application at https://wls.wisc.edu/. Data from the APMS are available on the application at https://ukdataservice.ac.uk/find-data/. Data from the MHAS are available on the application at https://www.mhasweb.org/Home/index.aspx. Data from KLoSA are available on the application at https://survey.keis.or.kr/eng/klosa/klosa01.jsp. Data from TILDA are available on the application at https://tilda.tcd.ie/. Data from CHARLS are available on the application at https://charls.pku.edu.cn/. Data from the IFLS are available on the application at https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS.html.
Code availability
The computational code for causal mediation analysis with bootstrap resampling is shared at https://github.com/Li-OmicsLab/Causal_NHB.
References
Malhi, G. S. & Mann, J. J. Depression. Lancet 392, 2299–2312 (2018).
Li, J. et al. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry 19, 249–250 (2020).
Charlson, F. J., Baxter, A. J., Cheng, H. G., Shidhaye, R. & Whiteford, H. A. The burden of mental, neurological, and substance use disorders in China and India: a systematic analysis of community representative epidemiological studies. Lancet 388, 376–389 (2016).
Zheng, X. et al. Dissecting the mediating and moderating effects of depression on the associations between traits and coronary artery disease: a two-step Mendelian randomization and phenome-wide interaction study. Int. J. Clin. Health Psychol. 23, 100394 (2023).
Friedrich, M. J. Depression is the leading cause of disability around the world. JAMA 317, 1517 (2017).
The cooperative human. Nat. Hum. Behav. 2, 427–428 (2018).
Krajc, K. et al. Marital status and survival in cancer patients: a systematic review and meta-analysis. Cancer Med. 12, 1685–1708 (2023).
de Oliveira, C. M. et al. Relationship between marital status and incidence of type 2 diabetes mellitus in a Brazilian rural population: the Baependi Heart Study. PLoS ONE 15, e0236869 (2020).
Wong, C. W. et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart 104, 1937–1948 (2018).
Leung, C. Y. et al. Association of marital status with total and cause-specific mortality in Asia. JAMA Netw. Open 5, e2214181 (2022).
Ensel, W. M. The role of age in the relationship of gender and marital status to depression. J. Nerv. Ment. Dis. 170, 536–543 (1982).
Kessler, R. C. & Essex, M. Marital status and depression: the importance of coping resources. Soc. Forces 61, 484–507 (1982).
Bebbington, P. Marital status and depression: a study of English national admission statistics. Acta Psychiatr. Scand. 75, 640–650 (1987).
Giannelis, A. et al. Examining the association between family status and depression in the UK Biobank. J. Affect. Disord. 279, 585–598 (2021).
Karney, B. R. Socioeconomic status and intimate relationships. Annu. Rev. Psychol. 72, 391–414 (2021).
Jang, S. N. et al. Marital status, gender, and depression: analysis of the baseline survey of the Korean Longitudinal Study of Ageing (KLoSA). Soc. Sci. Med. 69, 1608–1615 (2009).
Ambugo, E. A. Cross-country variation in the sociodemographic factors associated with major depressive episode in Norway, the United Kingdom, Ghana, and Kenya. Soc. Sci. Med. 113, 154–160 (2014).
Schaan, B. Widowhood and depression among older Europeans-the role of gender, caregiving, marital quality, and regional context. J. Gerontol. B 68, 431–442 (2013).
Bulloch, A. G. M., Williams, J. V. A., Lavorato, D. H. & Patten, S. B. The depression and marital status relationship is modified by both age and gender. J. Affect. Disord. 223, 65–68 (2017).
Prince, M. J. et al. Depression symptoms in late life assessed using the EURO-D scale: effect of age, gender and marital status in 14 European centres. Br. J. Psychiatry 174, 339–345 (1999).
St John, P. D. & Montgomery, P. R. Marital status, partner satisfaction, and depressive symptoms in older men and women. Can. J. Psychiatry 54, 487–492 (2009).
Shmulewitz, D. et al. The World Health Organization risk drinking levels measure of alcohol consumption: prevalence and health correlates in nationally representative surveys of U.S. adults, 2001–2002 and 2012–2013. Am. J. Psychiatry 178, 548–559 (2021).
Li, Y. et al. Physical activity, smoking, alcohol consumption and depressive symptoms among young, early mature and late mature people: a cross-sectional study of 76,223 in China. J. Affect. Disord. 299, 60–66 (2022).
Hinata, A. et al. Education, household income, and depressive symptoms in middle-aged and older Japanese adults. BMC Public Health 21, 2120 (2021).
Zhang, H. et al. The applied principles of EEG analysis methods in neuroscience and clinical neurology. Mil. Med. Res. 10, 67 (2023).
Herhaus, B., Kersting, A., Brahler, E. & Petrowski, K. Depression, anxiety and health status across different BMI classes: a representative study in Germany. J. Affect. Disord. 276, 45–52 (2020).
Lee, J. W., Shin, W. K. & Kim, Y. Impact of sex and marital status on the prevalence of perceived depression in association with food insecurity. PLoS ONE 15, e0234105 (2020).
Srivastava, S., Debnath, P., Shri, N. & Muhammad, T. The association of widowhood and living alone with depression among older adults in India. Sci. Rep. 11, 21641 (2021).
Pan, L. et al. Association of depressive symptoms with marital status among the middle-aged and elderly in rural China—serial mediating effects of sleep time, pain and life satisfaction. J. Affect. Disord. 303, 52–57 (2022).
Yan, X. Y., Huang, S. M., Huang, C. Q., Wu, W. H. & Qin, Y. Marital status and risk for late life depression: a meta-analysis of the published literature. J. Int. Med. Res. 39, 1142–1154 (2011).
Zhang, H. & Li, T. The role of willingness to sacrifice on the relationship between urban Chinese wives’ relative income and marital quality. J. Sex. Marital Ther. 41, 314–324 (2015).
Rostami, A., Ghazinour, M. & Richter, J. Marital satisfaction: the differential impact of social support dependent on situation and gender in medical staff in Iran. Glob. J. Health Sci. 5, 151–164 (2013).
Freak-Poli, R., Kung, C. S. J., Ryan, J. & Shields, M. A. Social isolation, social support, and loneliness profiles before and after spousal death and the buffering role of financial resources. J. Gerontol. B 77, 956–971 (2022).
Arias-de la Torre, J. et al. Prevalence and variability of current depressive disorder in 27 European countries: a population-based study. Lancet Public Health 6, e729–e738 (2021).
Rai, D., Zitko, P., Jones, K., Lynch, J. & Araya, R. Country- and individual-level socioeconomic determinants of depression: multilevel cross-national comparison. Br. J. Psychiatry 202, 195–203 (2013).
Curhan, K. B. et al. Just how bad negative affect is for your health depends on culture. Psychol. Sci. 25, 2277–2280 (2014).
De Vaus, J., Hornsey, M. J., Kuppens, P. & Bastian, B. Exploring the East–West divide in prevalence of affective disorder: a case for cultural differences in coping with negative emotion. Pers. Soc. Psychol. Rev. 22, 285–304 (2018).
Kross, E., Gard, D., Deldin, P., Clifton, J. & Ayduk, O. ‘Asking why’ from a distance: its cognitive and emotional consequences for people with major depressive disorder. J. Abnorm. Psychol. 121, 559–569 (2012).
Santini, Z. I. et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health 5, e62–e70 (2020).
Cohen, A. K., Nussbaum, J., Weintraub, M. L. R., Nichols, C. R. & Yen, I. H. Association of adult depression with educational attainment, aspirations, and expectations. Prev. Chronic Dis. 17, E94 (2020).
Patria, B. The longitudinal effects of education on depression: finding from the Indonesian National Survey. Front. Public Health 10, 1017995 (2022).
Molarius, A. & Granstrom, F. Educational differences in psychological distress? Results from a population-based sample of men and women in Sweden in 2012. BMJ Open 8, e021007 (2018).
Dinescu, D. et al. Is marriage a buzzkill? A twin study of marital status and alcohol consumption. J. Fam. Psychol. 30, 698–707 (2016).
Lindstrom, M. Social capital, economic conditions, marital status and daily smoking: a population-based study. Public Health 124, 71–77 (2010).
Romaniuk, M. et al. The relationship between chronic PTSD, cortical volumetry and white matter microstructure among Australian combat veterans. Mil. Med. Res. 9, 50 (2022).
Daviet, R. et al. Associations between alcohol consumption and gray and white matter volumes in the UK Biobank. Nat. Commun. 13, 1175 (2022).
Boksa, P. Smoking, psychiatric illness and the brain. J. Psychiatry Neurosci. 42, 147–149 (2017).
Jeong, J. E., Joo, S. H., Hahn, C., Kim, D. J. & Kim, T. S. Gender-specific association between alcohol consumption and stress perception, depressed mood, and suicidal ideation: the 2010–2015 KNHANES. Psychiatry Investig. 16, 386–396 (2019).
Horwitz, A. G., Zhao, Z. & Sen, S. Peak-end bias in retrospective recall of depressive symptoms on the PHQ-9. Psychol. Assess. 35, 378–381 (2023).
Salmon, C. et al. Marital status and prostate cancer incidence: a pooled analysis of 12 case–control studies from the PRACTICAL consortium. Eur. J. Epidemiol. 36, 913–925 (2021).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Radloff, L. S. The CES-D Scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, e58067 (1977).
Roberts, J., Lenton, P., Keetharuth, A. D. & Brazier, J. Quality of life impact of mental health conditions in England: results from the adult psychiatric morbidity surveys. Health Qual. Life Outcomes 12, 6 (2014).
Aguilar-Navarro, S. G., Fuentes-Cantu, A., Avila-Funes, J. A. & Garcia-Mayo, E. J. Validity and reliability of the screening questionnaire for geriatric depression used in the Mexican Health and Age Study. Salud Publica Mex. 49, 256–262 (2007).
Cho, M. J. & Kim, K. H. Use of the Center for Epidemiologic Studies Depression (CES-D) Scale in Korea. J. Nerv. Ment. Dis. 186, 304–310 (1998).
Kilburn, K. et al. Examination of performance of the Center for Epidemiologic Studies Depression Scale Short Form 10 among African youth in poor, rural households. BMC Psychiatry 18, 201 (2018).
Boey, K. W. Cross-validation of a short form of the CES-D in Chinese elderly. Int. J. Geriatr. Psychiatry 14, 608–617 (1999).
Cristobal-Narvaez, P., Haro, J. M. & Koyanagi, A. Longitudinal association between perceived stress and depression among community-dwelling older adults: findings from the Irish Longitudinal Study on Ageing. J. Affect. Disord. 299, 457–462 (2022).
Andresen, E. M., Malmgren, J. A., Carter, W. B. & Patrick, D. L. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am. J. Prev. Med. 10, 77–84 (1994).
Peltzer, K. & Pengpid, S. The prevalence and social determinants of hypertension among adults in Indonesia: a cross-sectional population-based national survey. Int. J. Hypertens. 2018, 5610725 (2018).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Br. Med. J. 327, 557–560 (2003).
Valente, M. J., Rijnhart, J. J. M., Smyth, H. L., Muniz, F. B. & MacKinnon, D. P. Causal mediation programs in R, Mplus, SAS, SPSS, and Stata. Struct. Equ. Model. 27, 975–984 (2020).
Acknowledgements
We thank each of the survey teams and study participants who made this analysis possible. This study was supported by grants from Macao Polytechnic University (RP/FCSD-02/2022 and RP/FCA-14/2023, H.H.Y.T. and K.L.) and a special grant for COVID-19 prevention and control from the Department of Education, Shanxi Province (J.L.). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
X.Z., L.S.W., C.W. and K.L. conceived and designed the study. X.Z., H.H.Y.T., A.X., C.K.L., Y.S., G.L., W.M., M.Z., Y.H. and J.L. collected and analysed the data. X.Z., H.H.Y.T., A.X. and K.L. drafted the paper. M.Z., Y.H., L.S.W., C.W. and K.L. critically reviewed and edited the paper. All authors reviewed and approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Human Behaviour thanks Amanda Hughes, Azra Ramezankhani and Fan Wang and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–14 and Tables 1–9.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhai, X., Tong, H.H.Y., Lam, C.K. et al. Association and causal mediation between marital status and depression in seven countries. Nat Hum Behav 8, 2392–2405 (2024). https://doi.org/10.1038/s41562-024-02033-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41562-024-02033-0
This article is cited by
-
Mediating effect of intolerance of uncertainty between feeling of unsafety and depression/well-being among a sample of Lebanese adults
Archives of Public Health (2025)
-
Association between chronic diseases and depressive inclinations among rural middle-aged and older adults
Scientific Reports (2025)