Abstract
Genome-wide association studies (GWASs) may help inform the etiology of infertility. Here, we perform GWAS meta-analyses across seven cohorts in up to 42,629 cases and 740,619 controls and identify 25 genetic risk loci for male and female infertility. We additionally identify up to 269 genetic loci associated with follicle-stimulating hormone, luteinizing hormone, estradiol and testosterone through sex-specific GWAS meta-analyses (n = 6,095–246,862). Exome sequencing analyses reveal that women carrying testosterone-lowering rare variants in some genes are at risk of infertility. However, we find no local or genome-wide genetic correlation between female infertility and reproductive hormones. While infertility is genetically correlated with endometriosis and polycystic ovary syndrome, we find limited genetic overlap between infertility and obesity. Finally, we show that the evolutionary persistence of infertility-risk alleles may be explained by directional selection. Taken together, we provide a comprehensive view of the genetic determinants of infertility across multiple diagnostic criteria.
Similar content being viewed by others
Main
Infertility, defined as the inability to achieve pregnancy within 12 months of regular unprotected sexual intercourse, affects one in six couples across the globe1. A range of demographic, environmental and genetic factors may drive infertility, including the age-related decline of sperm and oocyte quality and quantity, infectious diseases and rare Mendelian disorders such as cystic fibrosis. However, the exact cause remains undetermined in up to 28% of couples and 40% of women with infertility2. Given that current treatments such as in vitro fertilization pose physical, emotional and financial burdens on couples and healthcare systems, a richer understanding of the biology and pathophysiology of infertility is urgently necessary.
Heritable women’s reproductive health diseases such as endometriosis3 and polycystic ovary syndrome (PCOS)4 are thought to be responsible for a considerable proportion of female infertility, with PCOS in particular accounting for up to 80% of cases of anovulatory infertility4. It is hypothesized that sex-hormone dysregulation5,6 and obesity7, which often accompany reproductive diseases, may be involved in the etiology of infertility. Yet little is known about the genetic basis of reproductive hormones and infertility, which are not well phenotyped in men or women in large studies8,9. Moreover, negative selection against infertility naturally limits the frequency of risk alleles in the population. Genome-wide association studies (GWASs) have thus typically queried proxy measures of fertility such as childlessness10,11, which may partly arise from socioeconomic and behavioral factors.
We aggregated data from a range of sources, including primary care and hospital electronic health records and self-report, across seven cohorts with over 1.5 million participants, to perform GWAS meta-analyses for male infertility and five categories of female infertility. In addition, we report results from the largest sex-specific GWASs so far for five reproductive hormones. By aggregating these data with complementary rare-variant genetic association testing, we catalog the common and rare genetic contributions to infertility and reproductive hormone levels, quantify the extent of shared genetic architecture between these traits and prioritize genes for further functional investigation of the hormonal and non-hormonal drivers of infertility.
Results
Genome-wide meta-analyses identify new loci for infertility
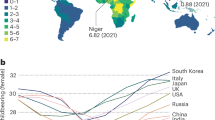
We identified female infertility of all causes (F-ALL), anatomical causes (F-ANAT), anovulation (F-ANOV), unknown causes (that is, idiopathic infertility as defined by exclusion of known causes of infertility (anatomical or anovulatory causes, PCOS, endometriosis or uterine leiomyomas)) (F-EXCL) or idiopathic infertility defined by inclusion of diagnostic codes for idiopathic infertility (F-INCL), as well as male infertility of all causes (M-ALL) in seven cohorts, primarily of European ancestry (EUR) (Fig. 1 and Supplementary Tables 1 and 2). The case–control ratio of all-cause female infertility ranged from 0.9% in the deCODE Genetics dataset to 11.7% in FinnGen, whereas the case–control ratio of male infertility was between 0.3% (UK Biobank (UKBB)) and 8.2% (Danish Biobank) (Fig. 1 and Supplementary Table 2). Anatomical female infertility was the least common cause of infertility in three of six cohorts (prevalence in UKBB of 0.01%, FinnGen of 0.8% and Estonian Biobank (EstBB) of 2.0%). Owing to varying sample ascertainment, the case–control ratio does not necessarily reflect the population prevalence of infertility.
a, The case numbers in each cohort contributing to GWAS meta-analyses (MA) for female (left) and male (right) infertility. The prevalence of all-cause infertility in each cohort (%) is noted on the bar plots. Danish, Danish Blood Donor Study/Copenhagen Hospital Biobank. Total case and control counts for each type of genetic analysis: all-ancestry GWAS meta-analysis, EUR-only GWAS meta-analysis and WES analyses (discovery, UKBB and replication, G&H and deCODE) are displayed. Male infertility in deCODE, with <100 cases, was excluded from GWAS meta-analysis. Note the different y-axis scales in each subplot. b, Downstream analyses performed for each type of genetic analysis: lead variants were identified via distance-based pruning for all-ancestry and EUR-only GWAS meta-analyses; colocalization, genetic correlations (genome wide and local), genetic overlap and selection analyses were only performed for EUR meta-analyses due to the need for ancestry-matched LD information; rare-variant and gene-burden discovery tests were performed with WES data for the UKBB EUR-ancestry subset and replicated in individuals with WES data in G&H and whole-genome sequencing (WGS) data in deCODE.
Novel genetic loci for infertility
We performed GWAS meta-analyses, testing up to 33 million genetic variants for associations with each of the above categories of infertility, in up to 42,629 cases and 740,619 controls in women, and 10,886 cases and 995,982 controls in men (Fig. 1 and Supplementary Table 2). We identified 22 unique genome-wide significant (P < 5 × 10−8) loci associated with at least one category of female infertility and three loci for male infertility (minor allele frequency (MAF) range 0.06–46%) (Fig. 2, Table 1 and Supplementary Fig. 1). Fourteen loci (63.6%) for female infertility reached nominal significance (P < 2.27 × 10−3, Bonferroni correction for 22 independent loci tested) in at least one other infertility category (Supplementary Note and Supplementary Fig. 19). There was no evidence for heterogeneity in lead variant effects across cohorts (Supplementary Note and Supplementary Table 3).
a, Genetic variants associated with F-ALL (top) and idiopathic infertility (unknown causes) defined by exclusion of known causes such as anatomical or anovulatory causes, PCOS, endometriosis and uterine leiomyomas (bottom). b, Genetic variants associated with M-ALL. Each point depicts a single SNP. The triangles represent SNPs that only reach genome-wide significance in all-ancestry GWAS meta-analyses. SNPs are annotated with the mapped gene. *The lead variant is reported in only one cohort. Summary statistics from whole-genome regression analyses were meta-analyzed using fixed-effect inverse-variance weighting in the METAL software to produce the displayed P values. The dashed line represents the multiple testing-corrected P value threshold of P < 5 × 10−8, accounting for ~1 million independent variants in the genome.
Among the variants associated with multiple subtypes of female infertility is rs9643050 (MAF of 6.01%), an intronic variant in PKHD1L1 (F-ALL, odds ratio (OR) (95% confidence interval (CI)) 1.13 (1.09–1.16); F-EXCL, OR 1.13 (1.09–1.17); F-INCL, OR 1.18 (1.11–1.25)). This variant is 76 kb upstream of EBAG9, an estrogen-responsive gene previously reported to have a recessive association with female infertility12,13 and thought to suppress maternal immune response during pregnancy14,15. We also identified an intronic variant in WNT4, rs61768001 (MAF of 16.5%), associated with three categories of female infertility (F-ALL, OR 1.10 (1.08–1.12); F-EXCL, OR 1.08 (1.06–1.11); F-INCL, OR 1.15 (1.11–1.19)). WNT4 is highly pleiotropic for female reproductive traits, as it is reported to associate with gestational length16, uterine fibroids17,18, endometriosis19,20, female genital prolapse21 and bilateral oophorectomy21. Such pleiotropy reflects the role of WNT4 as a key regulator of female reproductive organ development during embryogenesis22.
The nearest gene to the idiopathic infertility-associated variant rs111597692 (MAF of 3.23%; F-EXCL, OR 1.16 (1.10–1.22)) is TRHR, which encodes the thyrotropin-releasing hormone receptor. Mice with Trhr knockout display a phenotype similar to primary ovarian insufficiency23. The F-ANOV-associated variant rs72827480 (MAF of 40.1%, OR 1.10 (1.07–1.14)) colocalizes with a testis expression quantitative trait locus (eQTL) for INHBB in the GTEx Project (posterior probability (PP) of shared causal variant of 91.6%; Supplementary Table 4). INHBB encodes the beta subunit of inhibin B, which regulates hypothalamic, pituitary and gonadal hormone secretion24, and ovarian follicle and oocyte development25. rs111749498 (MAF of 2.73%, associated with F-ALL, OR 2.29 (1.72–3.04)) is near SLC47A2, which encodes a multidrug efflux pump that mediates excretion of the drug metformin, commonly used to manage infertility in women with PCOS26. Variants associated with all-cause female infertility are in genes enriched for expression in ovarian stromal cells (partitioned heritability P = 2.52 × 10−3; Supplementary Note).
The male infertility-associated variant rs75957543 (MAF of 1.25%, OR 1.67 (1.39–2.01)) is near UMODL1, which encodes the olfactorin protein, expressed along the migratory route of gonadotropin-releasing hormone neurons. Impairment of gonadotropin-releasing hormone migration is a feature of Kallmann’s syndrome, the most common genetic cause of hypogonadotropic infertility27. While mutations in UMODL1 have been shown to impact ovarian follicle development, granulosa cell apoptosis and female fertility in model organisms28,29, its role in male infertility remains unclear. Finally, an intronic variant in ENO4, which is expressed in the testis and may play a role in sperm motility30, is associated with male infertility (rs139862664, MAF of 0.72%, OR 2.58 (1.84–3.60)). Male mice with Eno4 knockout display infertility, abnormal sperm morphology and physiology and decreased testis weight, among other altered male reproductive tract phenotypes31.
Relationships with other female reproductive conditions
Genome wide, we observed positive genetic correlations (Fig. 3a) between endometriosis and F-ALL (rg (s.e.m.) = 0.585 (0.0785), P = 8.98 × 10−14) and F-INCL (rg = 0.710 (0.115), P = 5.94 × 10−10). We also observed positive correlation between F-ANOV and PCOS, the most common cause of anovulatory infertility (rg = 0.403 (0.131), P = 2.20 × 10−3). We tested for local bivariate genetic correlations between infertility and PCOS, endometriosis, heavy menstrual bleeding and uterine fibroids at 2,495 blocks across the genome, chosen to be approximately 1 Mb in length each, while minimizing linkage disequilibrium (LD) between blocks. Consistent with the genome-wide rg, we found positive local rg between female infertility and reproductive disorders at 11 regions (P < 1.91 × 10−5, Bonferroni adjustment for 2,618 local bivariate tests performed at regions with significant heritability of both traits in each pair tested; Fig. 4a and Supplementary Table 22). At 5/11 blocks, infertility was correlated with more than one reproductive condition, none of which had individual effects after conditioning upon the other associated reproductive disorders in the region (all P > 0.05; Supplementary Table 22).
SNP-based genetic correlations (rg) between significantly heritable phenotypes (Z > 4) were estimated using LD-score regression, performed using the LDSC software on a subset of 1 million HapMap3 SNPs. The points are colored by rg estimate, scaled by significance (−log10(P)), and labeled with the associated rg estimate if nominally significant without correction for multiple testing (P < 0.05). a, Genetic correlations among three definitions of female infertility (F-ALL, F-ANOV and F-INCL). b, Genetic correlations between female infertility traits and reproductive hormones testosterone, FSH and AMH (publicly available summary statistics) in female-specific analyses and TSH (publicly available summary statistics) from sex-combined analysis. c, Genetic correlations between female infertility traits and female reproductive conditions, with summary statistics generated from the largest available EUR-ancestry studies for each trait (Methods). d, Genetic correlations between female infertility traits and selected heritable phenotypes (Z > 4) in the UKBB, as generated by the Neale laboratory. Correlations with all heritable phenotypes can be found in Supplementary Table 12.
a, Local genetic correlations, estimated using LAVA, at 2,495 blocks across the genome. Each point represents a local bivariate genetic correlation between an infertility trait (F-ALL, F-ANOV or F-INCL) and reproductive hormone, reproductive condition or obesity-related trait. The dashed lines indicate significance (sig.) thresholds. The dashed line represents FDR-adjusted or Bonferroni-adjusted P values of 0.05. b, MiXeR estimates of polygenic overlap. The Venn diagrams indicate the estimated number (s.e.m.) of causal variants (in thousands) that explain 90% SNP heritability per component. The circle size reflects the degree of polygenicity. The bars outline the genome-wide genetic correlation (rG) and correlation in the shared polygenic component (rho). The colored portion of the bar is sized by the proportion of causal variants in the shared polygenic component as compared with all causal variants involved and colored by rho. Comp., comparative.
Furthermore, we used MiXeR32 to assess bivariate polygenic overlap, regardless of genome-wide genetic correlation, between infertility and reproductive conditions. We found that approximately 50% of causal single-nucleotide polymorphisms (SNPs) involved in endometriosis, and about 25% of causal SNPs involved in uterine fibroids were shared with the assessed infertility phenotypes, with varying degrees of genetic correlation in the shared component (Fig. 4b, Supplementary Table 24 and Supplementary Note). We noted that while there was substantial correlation in the shared component of F-ANOV and PCOS (rho (s.e.m.) of 0.878 (0.242)), only 97 (10.9%) of the 888 causal variants involved were shared; the majority (88.2%) of variants were unique to F-ANOV and only 8 variants (<1%) were unique to PCOS, suggesting that a small proportion of causal variants drive the genetic correlation between these traits (Fig. 4b and Supplementary Table 24).
We observed genome-wide negative correlation between F-ANOV and spontaneous dizygotic twinning, a heritable metric of female fecundity that captures the propensity for multiple ovulation33 (rg = −0.740 (0.182), P = 4.93 × 10−5). We also found substantial negative correlation in the shared polygenic component of these traits (rho (s.e.m.) = −0.920 (0.129)), with 32% (295) shared SNPs of the 912 total causal SNPs involved (Fig. 4b, Supplementary Table 24 and Supplementary Note).
Two loci associated with both endometriosis and female infertility (WNT4 and ESR1) may share the same putative causal variant (PP >93.6%; Supplementary Table 5). Variants in both these genes have previously been associated with endometriosis-related infertility34,35. GREB1 and SYNE1 also contain overlapping signals for infertility and endometriosis, but there is strong evidence against shared causal variants (PP >75%; Supplementary Table 5). Finally, three of eight loci for anovulatory infertility (INHBB, TTC28 and CHEK2) may share a causal variant with PCOS (PP >89.2%; Supplementary Table 5).
Evolutionary persistence of infertility-associated variants
The genome-wide SNP heritability estimates (on the liability scale, accounting for disease prevalence) for all categories of infertility were <10% (lowest for M-ALL at 1.12% (s.e.m. 0.93) and highest for F-ANOV at 9.54% (s.e.m. 2.16); Supplementary Table 6). This is lower than heritability estimates of two-thirds of all heritable binary phenotypes in the UKBB, with population prevalence similar to that of infertility (64 phenotypes with Z > 4 and prevalence <5%)36. We hypothesized that infertility risk-increasing alleles are subject to negative selection37, so we tested whether there was evidence for (1) variants associated with infertility in loci under historical or recent directional selection38 or (2) recent directional selection (over the past 2,000–3,000 years) measured by singleton density scores (SDSs)39 and balancing selection measured by standardized BetaScan2 scores40 at infertility loci (Supplementary Note).
While we found no genome-wide signature of directional selection against infertility (Supplementary Note), we observed extreme SDSs (in the highest 99.75th percentile of SNPs within 10 kb of a GWAS catalog variant) at the EBAG9 locus associated with female infertility, indicating recent positive selection (Fig. 5 and Supplementary Table 7).
Recent directional selection, as measured by trait-aligned SDSs (tSDSs) at the EBAG9 locus. The window of ±10 kb around the lead variant associated with F-ALL is displayed, along with the ___location of nearest gene TSSs. The tSDSs are aligned to the infertility risk-increasing allele, wherein a positive tSDS indicates positive selection for infertility risk-increasing allele at the locus. The dashed lines indicate 2.5th percentile (%ile) and 97.5th %ile of SDSs. Left: a locus plot depicting genomic position on the x axis and tSDS on the y axis. The lead variant rs1964514 (open circle) is not present in the tSDS dataset and thus is assigned a score of 0. Right: a scatter plot depicting relationship between −log10 of the GWAS P value for the variant association with F-ALL on the x axis and tSDS on the y axis.
Genetic determinants of reproductive hormone levels
Identification of novel reproductive hormone loci
As hormone dysregulation is central to many infertility diagnoses5,6, we conducted sex-specific GWAS meta-analyses of five reproductive hormones—follicle-stimulating hormone (FSH) (nfemale = 57,890, nmale = 6,095), luteinizing hormone (LH) (nfemale = 47,986, nmale = 6,769), estradiol (nfemale = 97,887, nmale = 39,165), progesterone (nfemale = 18,368) and total testosterone (nfemale = 246,862, nmale = 243,951)—collected at assessment center visits or identified through electronic health records, in six cohorts and publicly available summary statistics (Supplementary Table 9). We identified genome-wide significant loci associated with FSH (9 novel/2 previously known in females and 0/1 in males), LH (4/2 in females and 1/0 in males), estradiol (1/1 in females and 3/4 in males) and testosterone (39/118 in females and 67/206 in males), but found no genetic variants associated with progesterone (Supplementary Figs. 3, 4 and 20). Several of the reported signals we replicated are near genes encoding the hormone-specific subunits themselves, such as FSHB for FSH and LHB for LH, or enzymes for steroid-hormone metabolism, such as CYP3A7 for estradiol and HSD17B13 for testosterone (Supplementary Note).
Among the novel variants for testosterone in men were those near SPOCK1 (rs1073917: MAF of 30.7%, β (s.e.m.) = 0.0160 (0.0029), P = 4.69 × 10−8), which is a target for the androgen receptor41, and NR4A3 (rs10988865: MAF of 27.4%, β = 0.0161 (0.0029), P = 4.33 × 10−8), which coordinates the cellular response to corticotropin hormone- and thyrotropin hormone-releasing stimuli42 (Supplementary Table 10). Novel reproductive hormone variants associated with testosterone in women include those near LAMTOR4 (rs17250196: MAF of 5.13%, β = −0.131 (0.0067), P = 4.02 × 10−86), associated with hyperthyroidism23 and age at menarche and menopause43, and obesity-associated CCDC146 (rs138240474: MAF of 0.63%, β = −0.116 (0.0207), P = 2.03 × 10−8)44, which is expressed in the fallopian tubes and endometrium45.
Clinical measurements of FSH and LH may be used to diagnose premature menopause46, but our hormone GWASs based on these measurements were robust to this potential ascertainment bias (Supplementary Note). They were also robust to the inclusion of summary statistics from publicly available datasets and there was no evidence for heterogeneity in variant effects across cohorts (Supplementary Note).
Relationships with other heritable phenotypes
We observed no genome-wide genetic correlations between any category of female infertility and (1) any reproductive hormone in this study, (2) thyroid stimulating hormone (TSH) or (3) anti-Mullerian hormone (AMH), the latter two based on publicly available summary statistics47,48 (all P > 0.05, except the correlation between AMH and F-ANOV, rg (s.e.m.) = 0.748 (0.301), P = 0.0131; Fig. 3b). Consistent with the genome-wide results, we also found no evidence for local genetic correlations between any category of infertility and the above hormones (all P > 1.91 × 10−5; Fig. 4a, Supplementary Table 22 and Supplementary Note). The limited genetic correlation between infertility and reproductive hormones was mirrored in polygenic overlap analyses. The highest proportion of shared SNPs between these traits was 14.5% between F-ANOV and testosterone (209/1,444 variants shared, rho (s.e.m.) of 0.549 (0.252) in the shared polygenic component), followed by 14.0% between F-ANOV and AMH (123/881, rho (s.e.m.) of 0.993 (0.0301); Fig. 4b and Supplementary Table 24).
Mendelian randomization (MR) analyses indicated a genetically causal protective effect of FSH on risk of F-ALL (OR (95% CI) 0.776 (0.678–0.888), P = 2.15 × 10−4) and F-EXCL (0.716 (0.604–0.850), P = 1.26 × 10−4) (Supplementary Table 11). We found evidence for shared variants between hormones and infertility at the FSHB locus associated with FSH, LH and testosterone (PP >84.8% for colocalization with F-ANOV), and the ARL14EP locus associated with LH (PP 89.3% for colocalization with F-ANOV) (Supplementary Table 12). There was no evidence for colocalization at any of the >300 other genome-wide significant loci associated with infertility or reproductive hormones in our study (Supplementary Table 12).
Across 702 heritable phenotypes in the UKBB, we found 15 traits to be genetically correlated with female infertility, which we broadly group into: female reproductive conditions (such as having had a hysterectomy, rg (s.e.m.) = 0.481 (0.0963)), general illness (such as number of operations, rg = 0.266 (0.0588)), and cognitive test results (overall prospective memory test rg = 0.345 (0.0736) and overall fluid intelligence rg = −0.276 (0.0502)) (Fig. 3d and Supplementary Table 13). We found that 24 obesity-related traits, including body mass index (BMI), waist-to-hip ratio (WHR) and body fat percentage, were correlated with testosterone and FSH, but not with any category of female infertility (all P > 0.05; Fig. 3d, Supplementary Fig. 7 and Supplementary Table 13).
We found no evidence for local genetic correlations between any category of infertility and five obesity-related traits at 2,495 regions across the genome at a Bonferroni-adjusted significance threshold (all P > 1.91 × 10−5; Fig. 4a, Supplementary Table 22 and Supplementary Note). Polygenic analyses also revealed only limited overlap between infertility and obesity: fewer than 10% of causal SNPs involved were shared between infertility and any of the five obesity-related traits assessed (Fig. 4b, Supplementary Table 24 and Supplementary Note). The low overlap may reflect the polygenicity of obesity (between 4,050 and 11,000 causal variants), of which the majority (between 73.2% and 93.0%) are not involved in infertility (Supplementary Tables 23 and 24). Despite limited overlap, there was substantial negative correlation in the shared genetic components between F-INCL and comparative body size at age 10 years (451 shared SNPs of 4,385 involved, rho (s.e.m.) of −0.874 (0.143)) and adult BMI (393/11,185, rho (s.e.m.) of −0.640 (0.262)) (Fig. 4b and Supplementary Table 24).
Finally, MR analyses using genetic instruments for BMI, WHR and WHR adjusted for BMI (WHRadjBMI) indicated evidence for bidirectional causal relationships between infertility and abdominal obesity, independent of overall obesity. While genetically predicted WHRadjBMI was a risk factor for F-ALL (OR (95% CI) 1.10 (1.05–1.16), P = 1.71 × 10−4) and F-ANOV (OR 1.29 (1.16–1.45), P = 4.66 × 10−6), the latter was itself inferred to be causal for increased WHRadjBMI (β (s.e.m.) = 0.0547 (0.0133), P = 3.74 × 10−5) (Supplementary Table 11).
Rare-variant contribution to infertility and hormone levels
We analyzed the 450k UKBB exome-sequencing dataset to characterize the association between rare coding variation (MAF <1%) and binary traits with >100 cases (F-ALL (3,746 cases, 260,413 controls), F-EXCL (3,012 cases, 261,147 controls) and M-ALL (650 cases, 222,393 controls)), and quantitative traits with >10,000 participants (FSH-F (n = 20,800), LH-F (n = 16,391), estradiol-F (n = 54,609) and testosterone (nfemale = 197,038, nmale = 197,340)) (Fig. 1). Gene-burden analyses implicate the PLEKHG4 gene, which is highly expressed in the testis and ovary, for F-EXCL (burden test OR (95% CI) 1.04 (1.02–1.06) when aggregated across all variant annotations with MAF <1%, Cauchy P = 2.47 × 10−7) (Supplementary Table 14). This association did not replicate in the deCODE or Genes & Health (G&H) datasets (P > 0.05; Supplementary Tables 14, 20 and 21).
Novel genes implicated by gene-burden analyses
Gene-based analyses identify 18 genes associated with testosterone-F and 20 genes with testosterone-M (Cauchy combination P < 5 × 10−6), of which ten have not previously been implicated through GWASs (Supplementary Note). Across 43 gene–trait pairs with Cauchy P < 5 × 10−6 in UKBB, 13 (30.2%) replicate at nominal significance (P < 0.05) and two (4.65%) at Bonferroni-adjusted significance (P < 6.85 × 10−4) in either the deCODE or G&H datasets with consistent directions of effect (Supplementary Tables 14, 20 and 21).
We replicated the testosterone-F lowering associations of rare damaging variation in the hydroxysteroid dehydrogenase enzymes AKR1D1 (UKBB P = 1.76 × 10−8, deCODE P = 1.08 × 10−7, G&H P = 0.862) and AKR1C3 (UKBB P = 2.21 × 10−9, deCODE P = 1.12 × 10−6, G&H P = 8.75 × 10−8) in external cohorts (P < 6.85 × 10−4, Bonferroni adjustment for 43 independent gene–trait pairs) (Supplementary Tables 14, 20 and 21). We report the first known association of HSD11B1 with testosterone-F (burden test P = 1.93 × 10−6 when aggregated across missense variants with MAF <0.01%), with nominal replication in deCODE (P = 0.028); pathogenic variants in this gene are reported to cause hyperandrogenism due to cortisone reductase deficiency49 (Supplementary Fig. 11). We also report the association of testosterone-M with HSD17B2 (burden test P = 1.33 × 10−11 when aggregated across predicted loss-of-function (pLoF) variants with MAF <0.1%), which encodes the enzyme hydroxysteroid 17β-dehydrogenase 2 that regulates the biological potency of steroid hormones50 (Supplementary Fig. 11 and Supplementary Table 14). The association of rare damaging variation in HSD17B2 with lower testosterone nominally replicated in deCODE (P = 2.22 × 10−3) and G&H (P = 0.0481).
Infertility risk linked to rare hormone-associated variants
Two genes associated with testosterone in female UKBB participants were also associated with infertility risk (P < 1.00 × 10−3, Bonferroni adjustment for 50 unique genes): TRIM4 (F-ALL, burden test OR 1.03 (1.01–1.05), P = 4.05 × 10−4 across all variants with MAF <0.1%) and CYP3A43 (F-EXCL, burden test OR 1.02 (1.01–1.03), P = 4.84 × 10−4 across all variants with MAF <1%). Neither gene has previously been implicated in infertility.
Finally, we identified 29 unique genes carrying rare variants (MAF <1%) associated with testosterone in male or female participants in the UKBB, a majority of which had the same direction of effect in our EUR-ancestry GWAS meta-analyses excluding UKBB participants (Supplementary Table 15 and Supplementary Note). Nineteen of the 29 genes also contained nearby (±500 kb) common testosterone-associated variants from GWASs (MAF >1%), but at the majority (74%) of these loci, the effect of the rare variant was larger and remained upon conditioning on common variants (P < 1 × 10−7 after conditioning; Fig. 6a, Supplementary Table 15 and Supplementary Note).
a, The mean effect size versus allele frequency of genetic variants associated with total testosterone estimated using regression analyses. Variants discovered at genome-wide significance (P < 5 × 10−8) in GWAS meta-analyses (nfemale = 235,579, nmale = 235,096) and exome-wide significance (P < 1 × 10−7) in the UKBB WES analyses (nfemale = 197,038, nmale = 197,340) are plotted. The effect sizes are aligned to the minor allele, plotted against MAF on the log x axis. b, The effects of testosterone-associated rare variants (chr:pos:minor allele:major allele) on infertility in females (left: n cases/controls for F-ALL = 3,746/260,413; n cases/controls for F-EXCL = 3,012/261,147) and males (right: n cases/controls for M-ALL = 650/222,393) estimated using regression analyses. The effect sizes are aligned to the minor allele. Per gene, the variant with the lowest P value of all variants that reach exome-wide significance in UKBB WES analyses for testosterone is displayed, for all variants with nominally significant effects on infertility. Effect sizes (β and 95% CIs) for the variant effect on testosterone are to the left of each plot and effect sizes (ORs and 95% CIs) for the variant effect on infertility are to the right of each plot.
The 11 novel testosterone associations included a female testosterone-lowering missense variant in STAG3 (chr7:100204708:C:T, β = −0.284, P = 2.31 × 10−8). STAG3 is also associated with primary ovarian insufficiency in women51, and lack of Stag3 results in female infertility through the absence of oocytes in knockout mouse models23. We did not find a significant association between the STAG3 variant and female infertility in UKBB (P > 0.05). However, we observed increased risk of idiopathic infertility in women carrying a novel testosterone-lowering variant in GPC2 (chr7:100171569:G:A, F-EXCL OR 2.63 (1.40–4.92), P = 1.25 × 10−3) (Fig. 6b). GPC2 is highly expressed in the testis, and Gpc2-knockout mouse models display reduced adrenal gland size23. The gene has not previously been reported to be associated with testosterone or infertility. Taken together, our results indicate a potential role for infertility driven by rare hormone-disrupting variants.
Discussion
Our large-scale genetic investigation of infertility and related reproductive phenotypes in over 1.5 million individuals identified 22 genetic loci associated with female infertility, three with male infertility and novel variants associated with levels of the reproductive hormones FSH, LH, estradiol and total testosterone in men and women. Through rare-variant and gene-based analyses in the UKBB, we additionally identified 50 genes associated with testosterone levels, including the first reported hormone-associated variants in some members of the hydroxysteroid dehydrogenase enzyme family. Although there was evidence for distinct genetic architectures of infertility and reproductive hormones, we showed that individual genes containing rare protein-coding variants associated with testosterone (GPC2, CYP3A43 and TRIM4) were also associated with higher risk of infertility in the UKBB.
Previous efforts to catalog the genome-wide architecture of infertility have relied on proxy measures such as childlessness and number of children ever born10,11, which may be confounded by behavioral, socioeconomic and lifestyle factors. While we found modest genetic correlation between female infertility and age at first sexual intercourse (−18.8%), indicating that the latter captures some shared biology with fertility, our meta-analyses prioritize novel genes with putative roles in male and female gonads, such as TRHR for ovarian insufficiency and ENO4 for sperm motility, those responsible for development of the endocrine system, such as UMODL1, and pharmacogenetic interactions, such as the association of SLC47A2 with female infertility, potentially mediated by response to metformin.
The strong genetic correlation of 71% between idiopathic infertility and endometriosis may indicate that some proportion of idiopathic cases are due to underdiagnosis of endometriosis, whose early treatment may prevent future infertility52. Our subtype-specific analyses highlight the value in dissecting heterogeneous causes of infertility. For example, PCOS is a heritable cause of up to 80% of anovulatory infertility cases that may be treated through induced ovulation53. However, only three of eight loci for anovulatory infertility colocalize with known PCOS signals, the genetic correlation between these traits is only 40% and the majority (88%) of causal variants for anovulatory infertility are not shared with PCOS. These results suggest that other hypothalamic–pituitary–ovarian disorders, endocrinopathies (hypothyroidism, hyperprolactinemia and so on) and ovarian insufficiency may also contribute significantly to the genetic etiology of anovulatory infertility, and require treatments different from those for PCOS-associated infertility54. Weight loss for overweight patients is often recommended as beneficial for fertility55,56, but we did not find substantial genetic correlation between obesity and infertility. Our findings add genetic support to evidence from randomized controlled trials demonstrating limited fertility benefits from short-term weight loss in overweight and obese women57. Instead, we observed bidirectional causal relationships between abdominal obesity and anovulatory infertility, suggesting physiological feedback mechanisms whose complex interplay requires deeper study.
Our results indicate that balancing selection and recent positive selection at pleiotropic loci may explain the persistence of genetic factors for infertility. For example, the EBAG9 locus associated with female infertility is under directional selection, perhaps because EBAG9 plays a role in the adaptive immune memory response to infection58. A complementary role for EBAG9 may be in the placenta during early pregnancy, where reduction of EBAG9 levels is associated with inappropriate activation of the maternal immune system and results in fetal rejection15.
We employed a broad search strategy to maximize sample sizes for cases of infertility and reproductive hormone levels in our meta-analyses, which has its limitations. Diagnostic criteria for infertility vary by country and have changed over time1, which may explain the wide spread in the prevalence of infertility across cohorts. Reproductive hormone values in this study were assayed using different methodologies and at different ages and stages of the menstrual cycle in women. A majority of samples in our study were derived from the UKBB and measured during and postmenopause (ages 40–69 years), whereas infertility occurs premenopause, so we urge caution in interpreting the lack of correlation between these traits. Although we were able to adjust for covariates such as age, which can account for some of the effect of menopause on hormone levels, we did not have the data granularity to account for hormonal fluctuations during the menstrual cycle and pregnancy.
In this comprehensive large-scale investigation of the genetic determinants of infertility and reproductive hormones across men and women, we identified several genes associated with infertility and analyzed their effects on reproductive disease and selection pressures. We did not find evidence that reproductive hormone dysregulation and obesity are strongly correlated with infertility at the population level, but instead nominate individual hormone-associated genes with effects on fertility. Other genetic and non-genetic avenues must be explored to treat complex and heterogeneous fertility disorders that impact the physical, emotional and financial well-being of millions of individuals across the globe.
Methods
This research complies with all relevant ethical regulations. Each contributing study was approved by its respective board/committee as detailed in the Supplementary Note.
Study populations and phenotype identification
Binary traits (infertility)
Cases were identified in UKBB, Copenhagen Hospital Biobank and Danish Blood Donor Study, deCODE, EstBB, FinnGen and G&H (Supplementary Methods). We defined five categories of female infertility: F-ALL, F-ANOV, F-ANAT (including tubal, uterine and cervical origins), F-EXCL and F-INCL, and male infertility of all causes (M-ALL). Cases were identified through self-report (F-ALL, F-EXCL and M-ALL) and through primary- and secondary-care codes (Supplementary Table 1). Within each subtype, sex-matched controls were defined as individuals not identified as cases for that subtype. We additionally included publicly available multi-ancestry summary statistics from the Million Veteran Program (MVP) in meta-analyses of F-ALL (PheCode 626.8) and M-ALL (PheCode 609), downloaded from dbGaP59.
Quantitative traits (reproductive hormones)
Hormones were included from UKBB, Avon Longitudinal Study of Parents and Children (ALSPAC), deCODE, EstBB and G&H (Supplementary Note). We extracted measurements of FSH, LH, estradiol, progesterone and testosterone from biobank assessment centers or primary- and secondary-care records (Supplementary Table 16). If repeated measurements were available for an individual, we retained the recorded hormone value closest to the individual’s median hormone value over time. Each hormone was regressed on age, age2 and cohort-specific covariates specified below; the residuals from this regression were rank-based inverse normally transformed before GWAS.
Meta-analysis of GWAS summary statistics
Genome-wide association testing
Association analyses were performed separately within each ancestry and sex stratum for all strata with at least 100 cases (binary traits) or 1,000 individuals (quantitative traits). For binary traits, each variant passing quality control (QC) was tested for association under an additive model using REGENIE60 or Scalable and Accurate Implementation of GEneralized mixed model (SAIGE)61, with adjustments for age, age2 and cohort-specific covariates, with the Firth correction applied to control for inflation at rare variants and traits with low case–control ratios60,61. For quantitative traits, the rank-based inverse normally transformed hormone value was tested for association under an additive model using REGENIE60 or SAIGE61, with adjustments for cohort-specific genetic covariates. Any deviations from this GWAS protocol are noted in the Supplementary Note.
Meta-analysis
Before meta-analysis, summary statistics from all studies underwent thorough QC to retain variants that met the following criteria: (1) on the autosomes or X chromosome; (2) with imputation information score >0.8 (where available); (3) bi-allelic variants with A, C, G, T alleles; (4) with s.e.m. <10 and P values in (0, 1); and (5) without duplicate entries. Fixed-effects inverse-variance-weighted meta-analysis was performed using METAL62. We report results from EUR-ancestry and all-ancestry meta-analyses for each trait. Genome-wide significance was established at P < 5 × 10−8.
Identification of lead variants
Distance-based pruning was used to identify lead variants as the SNP with the lowest P value within each 1 Mb window at all loci with at least one genome-wide significant variant with P < 5 × 10−8. Lead hormone-associated variants were classified as novel or previously reported (Supplementary Note).
SNP-based heritability
The following analyses, which rely on population-specific LD patterns, were restricted to EUR-ancestry summary statistics with precomputed LD scores based on EUR-ancestry individuals in the 1000 Genomes dataset63, restricted to HapMap3 SNPs64. We estimated the SNP-based heritability (hG2) of a trait from GWAS summary statistics using LD-score regression as implemented in the LDSC software65. For infertility traits, the observed-scale heritability (hobs2) was converted to liability-scale heritability (hliab2), which accounts for the disease prevalence in the sample (k) and population (K), under the assumption that sample prevalence equals the population prevalence66.
Genetic correlations
Genome-wide genetic correlations
LDSC was used to estimate genetic correlations between infertility traits, hormone levels and a collection of other phenotypes in the UKBB in EUR-ancestry individuals. To simplify computation of rg across a large number of traits, we used an extension of the LDSC software that allows for simultaneous estimation of multiple genetic correlations67 (Supplementary Note).
Local genetic correlations
We applied LAVA v1.8.0 to assess bivariate correlations and perform multivariate regressions at local genomic regions68, using 1000 Genomes reference genotype data. Genomic loci that were created by partitioning the genome into 2,495 blocks of approximately 1 Mb each, while minimizing LD between blocks, were downloaded from ref. 69. As we quantified sample overlap between traits using cross-trait LDSC, the phenotypes assessed were restricted to those with significant genome-wide heritability (Z > 4): female infertility (F-ALL, F-ANOV and F-INCL), five reproductive conditions (endometriosis, PCOS, heavy menstrual bleeding, uterine fibroids and dizygotic twinning), four hormones (FSH-F, testosterone-F, TSH and AMH) and five obesity-related traits (BMI, body fat percentage, waist circumference, hip circumference and comparative body size at age 10 years). The target phenotype (female infertility: F-ALL, F-ANOV or F-INCL) was tested against all other traits.
At each genomic block, we filtered to phenotypes with sufficient local heritability (P < 2.00 × 10–5, family-wise error rate (FWER) controlled at 5% across 2,495 regions using the Bonferroni method, as recommended by the developers of LAVA68), resulting in 2,618 pairwise bivariate rg tests. At any regions where female infertility was correlated with multiple traits, we performed multiple regression to assess the independent predictive power of each trait. If traits were collinear in the region (local rg > 0.9), the trait with the greatest local rg with infertility was retained.
Polygenic overlap
We estimated polygenic overlap, irrespective of genetic correlation, using the causal mixture model MiXeR v1.3 (ref. 32) applied to GWAS summary statistics for female infertility (F-ALL, F-ANOV and F-INCL), five reproductive conditions (endometriosis, PCOS, heavy menstrual bleeding, uterine fibroids and dizygotic twinning), four reproductive hormones (FSH-F, testosterone-F, TSH and AMH) and five obesity-related traits (BMI, body fat percentage, waist circumference, hip circumference and comparative body size at age 10 years). For bivariate tests, the target phenotype (female infertility: F-ALL, F-ANOV or F-INCL) was tested against all other traits. GWAS summary statistics were formatted as for LDSC and LD structure was estimated using the 1000 Genomes project, as described previously32. Both univariate and bivariate models were fitted in two steps to ensure robust convergence, where the first ‘fast model’ estimates a set of parameters that are then constrained in the second ‘full model’. We only report estimates and s.e.m. for parameters from the ‘full model’, with the exception of Akaike information criterion (AIC) and Bayesian information criterion (BIC) from the first model, which are used to compare the univariate MiXeR model with LDSC regression, as recommended by the developers of MiXeR32. The number of causal variants is estimated from the fraction of total causal variants that cumulatively account for 90% of heritability in each component. Genome-wide genetic correlation estimates from MiXeR and LDSC were comparable as we used the same set of SNPs for both analyses; we calculated the P value for heterogeneity between these estimates using the z score for difference.
MR
Analyses were all performed with summary statistics from EUR-ancestry GWASs, using the TwoSampleMR v0.5.7 package70. Details of instrument construction, sensitivity analyses and MR methods are in the Supplementary Note.
Colocalization
The following analyses were all performed with summary statistics from EUR-ancestry GWASs, using the Bayesian framework implemented in the coloc v5.1.0 package71 under a single causal variant assumption72. Parameters for colocalization are provided in the Supplementary Note. We tested for colocalization between each female infertility category and each female-specific hormone trait (FSH, LH, estradiol and testosterone) at all genetic loci associated with at least one of the pair of traits tested. The single male infertility locus with common variants (MAF >1%) in the EUR-ancestry analysis did not contain enough significant associations (only 12 common variants with P < 1 × 10−6) for colocalization analyses. As we noticed that some lead variants for female infertility had previously been reported as associated with endometriosis and PCOS, we estimated the PP of colocalization of genetic signals between each category of female infertility and each of these two reproductive disorders. EUR-ancestry summary statistics for endometriosis and PCOS were obtained as described in ‘Genetic correlations’ section above. We assessed colocalization of genetic signals for female infertility with eQTLs for all proximal genes with transcription start sites (TSSs) within 1 Mb of an infertility lead variant. Publicly available eQTL data was downloaded from the GTEx project73.
Tissue and cell-type prioritization
We estimated the polygenic contributions of genes with tissue-specific expression profiles to the heritability of infertility and hormones using stratified LD-score regression (partitioned heritability analyses)65. We restricted these analyses to traits with highly significant heritability in EUR-ancestry analyses (Z > 7) (F-ALL, testosterone-F and testosterone-M), as recommended by the developers74.
Gene sets and LD scores for 205 tissues and cell types from the GTEx project database73 and the Franke laboratory single-cell database75 were downloaded from ref. 76. We established tissue-wide significance at −log10(P) >2.75, which corresponds to a false discovery rate (FDR) <5%.
As the ovary, a reproductive tissue of interest, is not well characterized in the GTEx project, we constructed annotation-specific LD scores for ovarian cell types from two publicly available single-cell RNA sequencing datasets (Supplementary Note).
Overlaps with genetic regions under selection
To avoid confounding by population stratification, selection look-ups were restricted to GWAS summary statistics from EUR-ancestry individuals. We assessed selection in three forms: (1) loci under directional selection, following guidelines described by Mathieson et al.11, (2) recent trait-wide directional selection using SDSs, following the protocol outlined by Field et al.39 and (3) balancing selection using standardized BetaScan2 scores40 (Supplementary Note).
WES analyses
Exome sequencing QC
QC outline
We first considered an initial set of ‘high-quality’ variants to evaluate the mean call rate and depth of coverage for each sample. We then ran a sample and variant level prefiltering step and calculated sample-level QC metrics. Using these metrics, we removed sample outliers based on median absolute deviation thresholds and excluded sites that did not pass variant QC according to Karzcewski et al.77. We then applied a genotype-level filter using genotype quality, depth and heterozygote allele balance. The resultant high-quality EUR call set consisted of 402,375 samples and 25,229,669 variants. For details, see Supplementary Note.
Variant annotation
We annotated variants using Variant Effect Predictor (VEP) v105 (corresponding to gencode v39)78 with the LOFTEE v1.04_GRCh38 (ref. 79) and dbNSFP80 plugins, annotating variants with CADD v1.6 (ref. 81) and REVEL using dbNSFP4.3 (ref. 82) and loss of function confidence using LOFTEE. Complete instructions and code for this step are provided in our VEP_105_LOFTEE repository83, which contains a docker/singularity container to ensure reproducibility of annotations. We then ran SpliceAI v1.3 (ref. 84) using the gencode v39 gene annotation file to ensure alignment between VEP and SpliceAI transcript annotations. We defined ‘canonical’ transcripts to be used for variant-specific annotations as follows: set MANE Select85 as the canonical, where available, and if a MANE Select transcript is not present, set canonical and restrict to protein-coding genes. For VEP 105, this is equivalent to selecting the ‘canonical’ transcript in protein-coding genes. Then, using the collection of missense, pLoF, splice metrics and annotations of variant consequence on the ‘canonical’ transcript, we determined a set of variant categories for gene-based testing (Supplementary Note).
Variant counts and average allele counts for each annotation, split by population label and binned by MAF are displayed in Supplementary Figs. 13 and 14, respectively.
Genetic association testing
We carried out rare-variant genetic association testing in the EUR-ancestry subset of the UKBB using SAIGE61, a mixed model framework that accounts for sample relatedness and case–control imbalance through a saddle-point approximation in binary traits. All rare-variant analysis was carried out on the UKBB Research Analysis Platform using SAIGE version wzhou88/saige:1.1.9 (ref. 61). In the sex-combined analyses, we account for age, sex, age2, age × sex, age2 × sex and the first 10 genetic principal components as fixed effects; and age, age2 and the first 10 principal components in sex-specific analyses. All continuous traits were inverse rank normalized before association testing.
For SAIGE step 0, we constructed a genetic relatedness matrix (GRM) using the UKBB genotyping array data. We LD pruned the genotyped data using PLINK (–indep-pairwise 50 5 0.05)86 and created a sparse GRM using 5,000 randomly selected markers, with relatedness cutoff of 0.05, using the createSparseGRM.R function within SAIGE. To generate a variance ratio file for subsequent steps in SAIGE, we extracted 1,000 variants each with minor allele count (MAC) <20 and MAC >20, and combined these markers to define a PLINK file for the variance ratio determination.
In SAIGE step 1 for each trait, the curated phenotype data and sparse GRM were used to fit a null model with no genetic contribution. All parameters were set at the defaults in SAIGE, except --relatednessCutoff 0.05, --useSparseGRMtoFitNULL TRUE and --isCateVarianceRatio TRUE. Tolerance for fitting the null generalized linear mixed model was set to 0.00001.
Rare-variant and gene-based testing
Following null model fitting, we carried out variant and gene-based testing in SAIGE step 2 using the variant categories described above, with the --is_single_in_groupTest TRUE flag. All other parameters were set to default, except --maxMAF_in_groupTest=0.0001,0.001,0.01, --is_Firth_beta TRUE, --pCutoffforFirth=0.1 and --is_fastTest TRUE. We included the following collection of group tests, using the annotations defined above (see ‘Variant annotation’ section).
-
High confidence pLoF
-
Damaging missense/protein altering
-
Other missense/protein altering
-
Synonymous
-
High confidence pLoF or damaging missense/protein altering
-
High confidence pLoF or damaging missense/protein altering or other missense/protein altering or synonymous
We then carried out Cauchy combination tests87 across these annotations for each gene.
Conditioning on nearby common variants
We conditioned rare variants that reached significance in exome-wide analyses (P < 1 × 10–7, Bonferroni adjustment for ~500,000 independent variants) on nearby common lead variants (±500 kb with MAF >1%), identified from the GWAS meta-analyses reported in this manuscript. The identified lead SNPs were included as covariates in SAIGE variant-based tests step 2.
Replication of exome-sequencing analyses
QC, variant annotation and genetic association testing at the gene level in the G&H whole-exome sequencing (WES) data were performed identically to UKBB, with any deviations noted below. The total sample size available was 44,028 (24,444 females and 19,584 males) with phenotype-specific sample sizes provided in Supplementary Tables 2 and 9. Sample sizes for WES analyses in G&H differ from sample sizes for GWASs because (1) further samples were added during the period between analyses and (2) not all G&H samples with genotyping have been exome sequenced as yet. A total of 4,723,926 variants passed QC. Genetic association analysis covariates were age, sex, age2 and the first 20 genetic principal components as fixed effects; and age, age2 and the first 20 principal components in sex-specific analyses.
Variant annotation, gene-burden models and association analyses performed in deCODE are described in the Supplementary Note.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Cohorts may be contacted individually for access to raw data. Meta-analysis summary statistics for all phenotypes are available through the GWAS Catalog study accession nos. GCST90483463 to GCST90483502.
Code availability
All code used in this study is available via GitHub at https://github.com/lindgrengroup/infertility_hormones and via Zenodo at https://doi.org/10.5281/zenodo.14528258 (ref. 88).
References
Infertility Prevalence Estimates, 1990–2021 (World Health Organization, 2023); https://www.who.int/publications/i/item/978920068315
Matzuk, M. M. & Lamb, D. J. The biology of infertility: research advances and clinical challenges. Nat. Med. 14, 1197–1213 (2008).
Bonavina, G. & Taylor, H. S. Endometriosis-associated infertility: from pathophysiology to tailored treatment. Front. Endocrinol. 13, 1020827 (2022).
Hoeger, K. M., Dokras, A. & Piltonen, T. Update on PCOS: consequences, challenges, and guiding treatment. J. Clin. Endocrinol. Metab. 106, e1071–e1083 (2021).
Vannuccini, S. et al. Infertility and reproductive disorders: impact of hormonal and inflammatory mechanisms on pregnancy outcome. Hum. Reprod. Update 22, 104–115 (2016).
Concepción-Zavaleta, M. et al. Assessment of hormonal status in male infertility. An update. Diabetes Metab. Syndr. 16, 102447 (2022).
Silvestris, E., de Pergola, G., Rosania, R. & Loverro, G. Obesity as disruptor of the female fertility. Reprod. Biol. Endocrinol. 16, 22 (2018).
A life-course approach to women’s health. Nat. Med. 30, 1 (2024).
Eisenberg, M. L. et al. Male infertility. Nat. Rev. Dis. Prim. 9, 49 (2023).
Barban, N. et al. Genome-wide analysis identifies 12 loci influencing human reproductive behavior. Nat. Genet. 48, 1462–1472 (2016).
Mathieson, I. et al. Genome-wide analysis identifies genetic effects on reproductive success and ongoing natural selection at the FADS locus. Nat. Hum. Behav. 7, 790–801 (2023).
Heyne, H. O. et al. Mono- and biallelic variant effects on disease at biobank scale. Nature 613, 519–525 (2023).
Ruotsalainen, S. et al. Inherited infertility: mapping loci associated with impaired female reproduction. Am. J. Hum. Genet. 111, 2789–2798 (2024).
Wicherek, L. et al. The placental RCAS1 expression during stillbirth. Reprod. Biol. Endocrinol. 3, 24 (2005).
Ohshima, K., Nakashima, M., Sonoda, K., Kikuchi, M. & Watanabe, T. Expression of RCAS1 and FasL in human trophoblasts and uterine glands during pregnancy: the possible role in immune privilege. Clin. Exp. Immunol. 123, 481–486 (2001).
Zhang, G. et al. Genetic associations with gestational duration and spontaneous preterm birth. N. Engl. J. Med. 377, 1156–1167 (2017).
Välimäki, N. et al. Genetic predisposition to uterine leiomyoma is determined by loci for genitourinary development and genome stability. eLife 7, e37110 (2018).
Rafnar, T. et al. Variants associating with uterine leiomyoma highlight genetic background shared by various cancers and hormone-related traits. Nat. Commun. 9, 3636 (2018).
Luong, H. T. et al. Fine mapping of variants associated with endometriosis in the WNT4 region on chromosome 1p36. Int. J. Mol. Epidemiol. Genet. 4, 193–206 (2013).
Rahmioglu, N. et al. The genetic basis of endometriosis and comorbidity with other pain and inflammatory conditions. Nat. Genet. 55, 423–436 (2023).
Kurki, M. I. et al. FinnGen provides genetic insights from a well-phenotyped isolated population. Nature 613, 508–518 (2023).
Bernard, P. & Harley, V. R. Wnt4 action in gonadal development and sex determination. Int. J. Biochem. Cell Biol. 39, 31–43 (2007).
Groza, T. et al. The International Mouse Phenotyping Consortium: comprehensive knockout phenotyping underpinning the study of human disease. Nucleic Acids Res. 51, D1038–D1045 (2023).
Ying, S. Y. Inhibins and activins: chemical properties and biological activity. Proc. Soc. Exp. Biol. Med. 186, 253–264 (1987).
Chada, M. et al. Inhibin B, follicle stimulating hormone, luteinizing hormone, and estradiol and their relationship to the regulation of follicle development in girls during childhood and puberty. Physiol. Res. 52, 341–346 (2003).
Morley, L. C., Tang, T. M. H. & Balen, A. H. on behalf of the Royal College of Obstetricians and Gynaecologists. Metformin therapy for the management of infertility in women with polycystic ovary syndrome. Scientific impact paper no. 13. BJOG 124, e306–e313 (2017).
Wray, S. Development of gonadotropin-releasing hormone-1 neurons. Front. Neuroendocrinol. 23, 292–316 (2002).
Wang, W. et al. Reduce fertility and skewed sex ratio in mice lacking Umodl1. Fertil. Steril. 94, S187 (2010).
Wang, W. et al. Overexpression of Uromodulin-like1 accelerates follicle depletion and subsequent ovarian degeneration. Cell Death Dis. 3, e433 (2012).
Nawaz, S. et al. A variant in sperm-specific glycolytic enzyme enolase 4 (ENO4) causes human male infertility. J. Gene Med. 26, e3583 (2024).
Nakamura, N. et al. Disruption of a spermatogenic cell-specific mouse enolase 4 (eno4) gene causes sperm structural defects and male infertility. Biol. Reprod. 88, 90 (2013).
Frei, O. et al. Bivariate causal mixture model quantifies polygenic overlap between complex traits beyond genetic correlation. Nat. Commun. 10, 2417 (2019).
Mbarek, H. et al. Genome-wide association study meta-analysis of dizygotic twinning illuminates genetic regulation of female fecundity. Hum. Reprod. 39, 240–257 (2024).
Paskulin, D. D., Cunha-Filho, J. S., Paskulin, L. D., Souza, C. A. B. & Ashton-Prolla, P. ESR1 rs9340799 is associated with endometriosis-related infertility and in vitro fertilization failure. Dis. Markers 35, 907–913 (2013).
Mafra, F., Catto, M., Bianco, B., Barbosa, C. P. & Christofolini, D. Association of WNT4 polymorphisms with endometriosis in infertile patients. J. Assist. Reprod. Genet. 32, 1359–1364 (2015).
Walters, R. Updating SNP heritability results from 4,236 phenotypes in UK Biobank. Neale Lab at the Broad Institute of Harvard & MIT http://www.nealelab.is/blog/2019/10/24/updating-snp-heritability-results-from-4236-phenotypes-in-uk-biobank (2019).
Tropf, F. C. et al. Human fertility, molecular genetics, and natural selection in modern societies. PLoS ONE 10, e0126821 (2015).
Mathieson, I. et al. Genome-wide patterns of selection in 230 ancient Eurasians. Nature 528, 499–503 (2015).
Field, Y. et al. Detection of human adaptation during the past 2000 years. Science 354, 760–764 (2016).
Siewert, K. M. & Voight, B. F. BetaScan2: standardized statistics to detect balancing selection utilizing substitution data. Genome Biol. Evol. 12, 3873–3877 (2020).
Rytinki, M. et al. Dynamic SUMOylation is linked to the activity cycles of androgen receptor in the cell nucleus. Mol. Cell. Biol. 32, 4195–4205 (2012).
Terashima, R., Tani, T., Sakakibara, K., Kurusu, S. & Kawaminami, M. Thyrotropin-releasing hormone stimulates NR4A3 expression in the pituitary thyrotrophs of proestrus rats. Endocr. J. 70, 805–814 (2023).
Kichaev, G. et al. Leveraging polygenic functional enrichment to improve GWAS power. Am. J. Hum. Genet. 104, 65–75 (2019).
Pulit, S. L. et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum. Mol. Genet. 28, 166–174 (2019).
Mountjoy, E. et al. An open approach to systematically prioritize causal variants and genes at all published human GWAS trait-associated loci. Nat. Genet. 53, 1527–1533 (2021).
NICE: Menopause, Diagnosis and Management—from Guideline to Practice (BMS, 2022); https://thebms.org.uk/wp-content/uploads/2022/12/09-BMS-TfC-NICE-Menopause-Diagnosis-and-Management-from-Guideline-to-Practice-Guideline-Summary-NOV2022-A.pdf
Verdiesen, R. M. G. et al. Genome-wide association study meta-analysis identifies three novel loci for circulating anti-Müllerian hormone levels in women. Hum. Reprod. 37, 1069–1082 (2022).
Williams, A. T. et al. Genome-wide association study of thyroid-stimulating hormone highlights new genes, pathways and associations with thyroid disease. Nat. Commun. 14, 6713 (2023).
Draper, N. et al. Mutations in the genes encoding 11β-hydroxysteroid dehydrogenase type 1 and hexose-6-phosphate dehydrogenase interact to cause cortisone reductase deficiency. Nat. Genet. 34, 434–439 (2003).
Saloniemi, T., Jokela, H., Strauss, L., Pakarinen, P. & Poutanen, M. The diversity of sex steroid action: novel functions of hydroxysteroid (17β) dehydrogenases as revealed by genetically modified mouse models. J. Endocrinol. 212, 27–40 (2012).
Caburet, S. et al. Mutant cohesin in premature ovarian failure. N. Engl. J. Med. 370, 943–949 (2014).
de Ziegler, D., Borghese, B. & Chapron, C. Endometriosis and infertility: pathophysiology and management. Lancet 376, 730–738 (2010).
Thessaloniki ESHRE/ASRM-sponsored PCOS Consensus Workshop Group. Consensus on infertility treatment related to polycystic ovary syndrome. Hum. Reprod. 23, 462–477 (2008).
Crosignani, P. G., Bianchedi, D., Riccaboni, A. & Vegetti, W. Management of anovulatory infertility. Hum. Reprod. 14, 108–119 (1999).
Gambineri, A. et al. Female infertility: which role for obesity? Int. J. Obes. Suppl. 9, 65–72 (2019).
Maheshwari, A., Stofberg, L. & Bhattacharya, S. Effect of overweight and obesity on assisted reproductive technology—a systematic review. Hum. Reprod. Update 13, 433–444 (2007).
Gaskins, A. J. Recent advances in understanding the relationship between long- and short-term weight change and fertility. F1000Res. 7, F1000 Faculty Rev-1702 (2018).
Rüder, C. et al. The tumor-associated antigen EBAG9 negatively regulates the cytolytic capacity of mouse CD8+ T cells. J. Clin. Invest. 119, 2184–2203 (2009).
Verma, A. et al. Diversity and scale: genetic architecture of 2068 traits in the VA Million Veteran Program. Science 385, eadj1182 (2024).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 53, 1097–1103 (2021).
Zhou, W. et al. Efficiently controlling for case–control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 50, 1335–1341 (2018).
Willer, C. J., Li, Y. & Abecasis, G. R. METAL: fast and efficient meta-analysis of genomewide association scans. Bioinformatics 26, 2190–2191 (2010).
1000 Genomes Project Consortium, et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
International HapMap 3 Consortium, et al. Integrating common and rare genetic variation in diverse human populations. Nature 467, 52–58 (2010).
Bulik-Sullivan, B. K. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Dempster, E. R. & Lerner, I. M. Heritability of threshold characters. Genetics 35, 212–236 (1950).
Bulik-Sullivan, B. et al. astheeggeggs/ldsc: ldsc rg vector (v1.0.0). Zenodo https://doi.org/10.5281/zenodo.10497662 (2024).
Werme, J., van der Sluis, S., Posthuma, D. & de Leeuw, C. A. An integrated framework for local genetic correlation analysis. Nat. Genet. 54, 274–282 (2022).
Werme, J. & de Leeuw, C. LAVA partitioning algorithm. GitHub https://github.com/cadeleeuw/lava-partitioning (2024).
Hemani, G. et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 7, e34408 (2018).
Giambartolomei, C. et al. Bayesian test for colocalisation between pairs of genetic association studies using summary statistics. PLoS Genet. 10, e1004383 (2014).
Wallace, C. Eliciting priors and relaxing the single causal variant assumption in colocalisation analyses. PLoS Genet. 16, e1008720 (2020).
GTEx Consortium. The Genotype-Tissue Expression (GTEx) project. Nat. Genet. 45, 580–585 (2013).
Finucane, H. K. et al. Partitioning heritability by functional annotation using genome-wide association summary statistics. Nat. Genet. 47, 1228–1235 (2015).
Pers, T. H. et al. Biological interpretation of genome-wide association studies using predicted gene functions. Nat. Commun. 6, 5890 (2015).
Finucane, H. K. et al. Heritability enrichment of specifically expressed genes identifies disease-relevant tissues and cell types. Nat. Genet. 50, 621–629 (2018).
Karczewski, K. J. et al. Systematic single-variant and gene-based association testing of thousands of phenotypes in 394,841 UK Biobank exomes. Cell Genom. 2, 100168 (2022).
McLaren, W. et al. The Ensembl variant effect predictor. Genome Biol. 17, 122 (2016).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
Liu, X., Li, C., Mou, C., Dong, Y. & Tu, Y. dbNSFP v4: a comprehensive database of transcript-specific functional predictions and annotations for human nonsynonymous and splice-site SNVs. Genome Med. 12, 103 (2020).
Rentzsch, P., Witten, D., Cooper, G. M., Shendure, J. & Kircher, M. CADD: predicting the deleteriousness of variants throughout the human genome. Nucleic Acids Res. 47, D886–D894 (2019).
Ioannidis, N. M. et al. REVEL: an ensemble method for predicting the pathogenicity of rare missense variants. Am. J. Hum. Genet. 99, 877–885 (2016).
Hill, B. & Palmer, D. S. vep105_loftee. Github https://github.com/BRaVa-genetics/vep105_loftee (2023).
Jaganathan, K. et al. Predicting splicing from primary sequence with deep learning. Cell 176, 535–548.e24 (2019).
Morales, J. et al. A joint NCBI and EMBL-EBI transcript set for clinical genomics and research. Nature 604, 310–315 (2022).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. Gigascience 4, 7 (2015).
Liu, Y. & Xie, J. Cauchy combination test: a powerful test with analytic p-value calculation under arbitrary dependency structures. J. Am. Stat. Assoc. 115, 393–402 (2020).
Venkatesh, S. S. et al. lindgrengroup/infertility_hormones. Zenodo https://doi.org/10.5281/zenodo.14528258 (2025).
Acknowledgements
We thank P. Palamara and Z. Kutalik for helpful discussions. We are grateful to the participants of all cohorts. This research has partly been conducted using the UKBB Resource under application no. 11867. G&H is/has recently been core-funded by Wellcome (WT102627, WT210561), the Medical Research Council (UK) (M009017, MR/X009777/1 and MR/X009920/1), Higher Education Funding Council for England Catalyst, Barts Charity (845/1796), Health Data Research UK (for London substantive site) and research delivery support from the NHS National Institute for Health Research Clinical Research Network (North Thames). G&H is/has recently been funded by Alnylam Pharmaceuticals, Genomics PLC; and a Life Sciences Industry Consortium of Astra Zeneca PLC, Bristol-Myers Squibb Company, GlaxoSmithKline Research and Development Limited, Maze Therapeutics Inc, Merck Sharp & Dohme LLC, Novo Nordisk A/S, Pfizer Inc, Takeda Development Centre Americas Inc. We thank Social Action for Health, Centre of The Cell, members of our Community Advisory Group and staff who have recruited and collected data from volunteers. We thank the NIHR National Biosample Centre (UK Biocentre), the Social Genetic and Developmental Psychiatry Centre (King’s College London), Wellcome Sanger Institute and Broad Institute for sample processing, genotyping, sequencing and variant annotation. We thank Barts Health NHS Trust, NHS Clinical Commissioning Groups (City and Hackney, Waltham Forest, Tower Hamlets, Newham, Redbridge, Havering, Barking and Dagenham), East London NHS Foundation Trust, Bradford Teaching Hospitals NHS Foundation Trust, Public Health England (especially D. Wyllie), Discovery Data Service/Endeavour Health Charitable Trust (especially D. Stables), Voror Health Technologies Ltd (especially S. Don) and NHS England (for what was NHS Digital) for GDPR-compliant data sharing backed by individual written informed consent. Most of all, we thank all of the volunteers participating in G&H. This study was funded by the European Union through the European Regional Development Fund project no. 2014-2020.4.01.15-0012 GENTRANSMED. Data analysis was carried out in part in the High-Performance Computing Center of University of Tartu. This research has partly been conducted using the ALSPAC resource under project no. B4568. The activities of the EstBB are regulated by the Human Genes Research Act, which was adopted in 2000 specifically for the operations of the EstBB. Individual-level data analysis in the EstBB was carried out under ethical approval 1.1-12/624 from the Estonian Committee on Bioethics and Human Research (Estonian Ministry of Social Affairs), using data according to release application 3-10/GI/10790 from the EstBB. This study was funded by the Estonian Research Council grants PRG1911 and by the Ministry of Education and Research Centres of Excellence grant TK214 Centre of Excellence for Personalised Medicine. We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. The UK Medical Research Council and Wellcome (grant ref. 217065/Z/19/Z) and the University of Bristol provide core support for ALSPAC. A comprehensive list of grants funding is available on the ALSPAC website (http://www.bristol.ac.uk/alspac/external/documents/grant-acknowledgements.pdf). Genome-wide genotyping data was generated by Sample Logistics and Genotyping Facilities at Wellcome Sanger Institute and LabCorp (Laboratory Corporation of America) using support from 23andMe. We acknowledge the contribution of the participants in the deCODE study. Patients and control subjects in FinnGen provided informed consent for biobank research, based on the Finnish Biobank Act. Alternatively, separate research cohorts, collected prior to when the Finnish Biobank Act came into effect (in September 2013) and start of FinnGen (August 2017), were collected based on study-specific consents and later transferred to the Finnish biobanks after approval by Fimea (Finnish Medicines Agency), the National Supervisory Authority for Welfare and Health. Recruitment protocols followed the biobank protocols approved by Fimea. The Coordinating Ethics Committee of the Hospital District of Helsinki and Uusimaa (HUS) statement number for the FinnGen study is Nr HUS/990/2017. The FinnGen study is approved by Finnish Institute for Health and Welfare (permit nos. THL/2031/6.02.00/2017, THL/1101/5.05.00/2017, THL/341/6.02.00/2018, THL/2222/6.02.00/2018, THL/283/6.02.00/2019, THL/1721/5.05.00/2019 and THL/1524/5.05.00/2020), Digital and population data service agency (permit nos. VRK43431/2017-3, VRK/6909/2018-3 and VRK/4415/2019-3), the Social Insurance Institution (permit nos. KELA 58/522/2017, KELA 131/522/2018, KELA 70/522/2019, KELA 98/522/2019, KELA 134/522/2019, KELA 138/522/2019, KELA 2/522/2020 and KELA 16/522/2020), Findata (permit numbers THL/2364/14.02/2020, THL/4055/14.06.00/2020, THL/3433/14.06.00/2020, THL/4432/14.06/2020, THL/5189/14.06/2020, THL/5894/14.06.00/2020, THL/6619/14.06.00/2020, THL/209/14.06.00/2021, THL/688/14.06.00/2021, THL/1284/14.06.00/2021, THL/1965/14.06.00/2021, THL/5546/14.02.00/2020, THL/2658/14.06.00/2021 and THL/4235/14.06.00/2021), Statistics Finland (permit nos. TK-53-1041-17 and TK/143/07.03.00/2020 (earlier TK-53-90-20) TK/1735/07.03.00/2021, TK/3112/07.03.00/2021) and Finnish Registry for Kidney Diseases permission/extract from the meeting minutes on 4 July 2019. The Biobank Access Decisions for FinnGen samples and data utilized in FinnGen Data Freeze 10 include THL Biobank BB2017_55, BB2017_111, BB2018_19, BB_2018_34, BB_2018_67, BB2018_71, BB2019_7, BB2019_8, BB2019_26, BB2020_1, BB2021_65, Finnish Red Cross Blood Service Biobank 7.12.2017, Helsinki Biobank HUS/359/2017, HUS/248/2020, HUS/150/2022 § 12, §13, §14, §15, §16, §17, §18, and §23, Auria Biobank AB17-5154 and amendment no. 1 (17 August 2020) and amendments BB_2021-0140, BB_2021-0156 (26 August 2021, 2 February 2022), BB_2021-0169, BB_2021-0179, BB_2021-0161, AB20-5926 and amendment no. 1 (23 April 2020) and its modification (22 September 2021), Biobank Borealis of Northern Finland_2017_1013, 2021_5010, 2021_5018, 2021_5015, 2021_5023, 2021_5017, 2022_6001, Biobank of Eastern Finland 1186/2018 and amendment 22 § /2020, 53§/2021, 13§/2022, 14§/2022, 15§/2022, Finnish Clinical Biobank Tampere MH0004 and amendments (21.02.2020 and 06.10.2020), §8/2021, §9/2022, §10/2022, §12/2022, §20/2022, §21/2022, §22/2022, §23/2022, Central Finland Biobank 1-2017, and Terveystalo Biobank STB 2018001 and amendment 25 August 2020, Finnish Hematological Registry and Clinical Biobank decision 18 June 2021, Arctic biobank P0844: ARC_2021_1001. We acknowledge the participants and investigators of FinnGen study. The FinnGen project is funded by two grants from Business Finland (HUS 4685/31/2016 and UH 4386/31/2016) and the following industry partners: AbbVie Inc., Astra Zeneca UK Ltd, Biogen MA Inc., Bristol-Myers Squibb (and Celgene Corporation & Celgene International II Sàrl), Genentech Inc., Merck Sharp & Dohme LCC, Pfizer Inc., GlaxoSmithKline Intellectual Property Development Ltd., Sanofi US Services Inc., Maze Therapeutics Inc., Janssen Biotech Inc, Novartis Pharma AG and Boehringer Ingelheim International GmbH. We acknowledge the following biobanks for delivering biobank samples to FinnGen: Auria Biobank (www.auria.fi/biopankki), THL Biobank (www.thl.fi/biobank), Helsinki Biobank (www.helsinginbiopankki.fi), Biobank Borealis of Northern Finland (https://www.ppshp.fi/Tutkimus-ja-opetus/Biopankki/Pages/Biobank Borealis-briefly-in-English.aspx), Finnish Clinical Biobank Tampere (www.tays.fi/en-US/Research_and_development/Finnish_Clinical_Biobank_Tampere), Biobank of Eastern Finland (www.ita-suomenbiopankki.fi/en), Central Finland Biobank (www.ksshp.fi/fi-FI/Potilaalle/Biopankki), Finnish Red Cross Blood Service Biobank (www.veripalvelu.fi/verenluovutus/biopankkitoiminta), Terveystalo Biobank (www.terveystalo.com/fi/Yritystietoa/Terveystalo-Biopankki/Biopankki/) and Arctic Biobank (https://www.oulu.fi/en/university/faculties-and-units/faculty-medicine/northern-finland-birth-cohorts-and-arctic-biobank). All Finnish Biobanks are members of BBMRI.fi infrastructure (www.bbmri.fi). Finnish Biobank Cooperative–FINBB (https://finbb.fi/) is the coordinator of BBMRI–ERIC operations in Finland. The Finnish biobank data can be accessed through the Fingenious services (https://site.fingenious.fi/en/) managed by FINBB. This study was based on the CHB reproduction protocol and DBDS (ethical approval NVK-1805807; NVK-1700407; SJ-740). S.S.V. was supported by the Rhodes Scholarships, Clarendon Fund, and the Medical Sciences Doctoral Training Centre at the University of Oxford. L.B.L.W. was supported by the Wellcome Trust. B.M.J. was funded by a Medical Research Council (MRC) Clinical Research Training Fellowship (CRTF) jointly supported by the UK MS Society (B.M.J.; grant reference: MR/V028766/1). A.P. is supported by Alma and K.A. Snellman Foundation. Contributions by A.E. and D.A.L. are supported by the UK Medical Research Council (MC_UU_00032/05) and the European Research Council under the European Union’s Horizon 2020 research and innovation program (grant agreement no. 101021566). D.A.L. is also supported by the British Heart Foundation (CH/F/20/90003). G.K. is funded by Wellcome (grant no. 220540/Z/20/A, ‘Wellcome Sanger Institute Quinquennial Review 2021–2026’). D.W., K.B. and H.S.N. acknowledge the Novo Nordisk Foundation (grant nos. NNF22OC0077221 and NNF23OC0087269, NNF17OC0027594 and NNF14CC0001 (D.W. and K.B.)), and the A.P. Moller Foundation. Y.-M.C. and S.B.S. are supported by NIH (1P50HD104224-01 and 2R37HD043341), the FDA (R01 FD007843), and the Gates Foundation (INV-024200). R.B. is supported by NIH (P50HD104224-01 and R01DE034452) and the Gates Foundation (INV-024200). C.M.L. is supported by the Li Ka Shing Foundation, NIHR Oxford Biomedical Research Centre, Oxford, NIH (1P50HD104224-01), Gates Foundation (INV-024200) and a Wellcome Trust Investigator Award (221782/Z/20/Z). This research was supported by the Wellcome Trust Core Award grant no. 203141/Z/16/Z with additional support from the NIHR Oxford BRC. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Consortia
Contributions
S.S.V. conceptualized the study, curated and analyzed data, supervised analyses and wrote the manuscript. L.B.L.W. conceptualized the study, curated and analyzed data and supervised analyses. D.S.P. and T.F. analyzed UKBB data and supervised analyses. N.A.B., B.H. and F.H.L. analyzed UKBB data. M.J.P. analyzed data. S.R. analyzed data and supervised analyses. P.D.R. analyzed Copenhagen Hospital Biobank and Danish Blood Donor Study (CHB/DBDS) data. M. Nyegaard supervised analyses of CHB/DBDS data. O.B.P., C.E., M.T.B., B.A.J., C.M., S.R.O., E.S., H.U., H.S.N., K.B., D.W. and A.J. provided resources from CHB/DBDS. B.M.J. and G.K. analyzed G&H data. D.A.v.H. supervised analyses and provided resources from G&H. J.F. analyzed EstBB data. R.M. supervised analyses and provided resources from EstBB. M.K.K. and A.P. analyzed FinnGen data. H.L. supervised analyses and provided resources from FinnGen. A.E. analyzed ALSPAC data. N.J.T., D.A.L. and A.F. supervised analyses and provided resources from ALSPAC. V.S. and G.T. analyzed deCODE data. H.H., I.J., I.O., A.H., T.S. and K.S. provided resources from deCODE. N.H. and D.I.B. provided resources. Y.-M.C., M.L. and R.B. contributed to defining phenotypes and provided clinical interpretation of results. S.B.S. provided clinical interpretation of results and acquired funding. T.L. supervised analyses, provided resources from EstBB, and wrote the manuscript. C.M.L. conceptualized the study and acquired funding. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Competing interests
L.B.L.W. is currently employed by Novo Nordisk Research Centre Oxford but, while she conducted the research described in this manuscript, was only affiliated to the University of Oxford. V.S., G.T., H.H., I.J. and K.S. are employees of deCODE genetics, a subsidiary of Amgen. C.M.L. is a part-time employee of Population Health Partners, owns equity in Population Health Partners and its subsidiaries, reports grants from Bayer AG and Novo Nordisk and has a partner who works at Vertex. The other authors declare no competing interests.
Peer review
Peer review information
Nature Genetics thanks the anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information
Supplementary Figs. 1–20 and Note
Supplementary Table 1
Supplementary Tables 1–25.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Venkatesh, S.S., Wittemans, L.B.L., Palmer, D.S. et al. Genome-wide analyses identify 25 infertility loci and relationships with reproductive traits across the allele frequency spectrum. Nat Genet 57, 1107–1118 (2025). https://doi.org/10.1038/s41588-025-02156-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41588-025-02156-8
This article is cited by
-
Genetic insights into infertility from large-scale analyses
Nature Genetics (2025)