Abstract
Identification of obstructive coronary artery disease (OCAD) in patients with chest pain is a clinical challenge. The value of corrected QT interval (QTc) for the prediction of OCAD has yet to be established. We consecutively enrolled 1741 patients with suspected angina. The presence of obstructive OCAD was defined as ≥ 50% diameter stenosis by coronary angiography. The pre-test probability was evaluated by combining QTc prolongation with the CAD Consortium clinical score (CAD2) and the updated Diamond-Forrester (UDF) score. OCAD was detected in 661 patients (38.0%). QTc was longer in patients with OCAD compared with those without OCAD (444 ± 34 vs. 429 ± 28 ms, p < 0.001). QTc was increased by the severity of OCAD (P < 0.001). QTc prolongation was associated with OCAD (odds ratio (OR), 2.27; 95% confidence interval (CI), 1.81–2.85). With QTc, the C-statistics increased significantly from 0.68 (95% CI 0.66–0.71) to 0.76 (95% CI 0.74–0.78) in the CAD2 and from 0.64 (95% CI 0.62–0.67) to 0.74 (95% CI 0.72–0.77) in the UDF score, respectively. QT prolongation predicted the presence of OCAD and the QTc improved model performance to predict OCAD compared with CAD2 or UDF scores in patients with suspected angina.
Similar content being viewed by others
Introduction
Identification of obstructive coronary artery disease (OCAD) in patients with chest pain is a clinical challenge, particularly in the outpatient clinic. Careful history taking, physical examination and resting electrocardiography (ECG) are important measures in determining initially whether or not to recommend specific tests and invasive coronary angiography (CAG)1. Although an abnormal repolarization pattern or presence of Q wave on resting ECG are signs of OCAD, resting ECG should not be used to rule out myocardial ischemia, since it is often normal even in patients with severe OCAD1. Updated Diamond-Forrester (UDF) and CAD consortium (CAD2) scores have been used to predict OCAD, based on age, sex, typical symptoms and cardiovascular risk factors, but not ECG findings2,3,4.
Corrected QT (QTc) interval based on resting ECG is a useful marker to stratify patients with increased risk of ventricular arrhythmia5. QT prolongation has been reported to predict cardiovascular mortality and sudden cardiac death5,6. Various factors including aging, sex, medications and cardiovascular diseases are associated with QT prolongation7,8. Myocardial ischemia increased the repolarization heterogeneity of ventricle, and prolonged the duration of electrocardiographic QT interval9. In acute coronary syndrome, acute myocardial ischemia was strongly correlated with prolonged QTc interval10,11. Although studies have investigated the relation between OCAD and QTc interval12,13, it is still unclear whether OCAD is associated with QTc interval in patients with stable angina. We hypothesized that QT prolongation is one of the parameters for the detection of significant OCAD in patients with chest pain.
Therefore, we investigated the association between QTc interval and OCAD. We evaluated the incremental diagnostic value of QT prolongation in conventional tests to identify patients with significant OCAD in clinical practice.
Results
Baseline characteristics of population
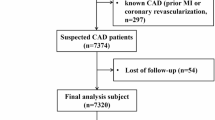
A total of 1829 consecutive patients visited the outpatient clinic with suspected angina. However, 88 patients were excluded from this study for the following reasons: atrial fibrillation (n = 62); and bundle branch block (n = 26). Finally, our study analyzed 1741 patients (M/F, n = 661/1080; mean age, 61 ± 11 years). Table 1 describes the clinical characteristics of the total study population. Obesity, hypertension, and diabetes mellitus (DM) were observed in 818 (47.0%), 909 (52.2%), and 366 (21.0%) patients, respectively. The mean value of QTc interval was 434.5 ± 31.3 ms. OCAD on CAG was found in 661 patients (38.0%). One-, two-, and three-vessel diseases were diagnosed in 450 (25.8%), 172 (9.9%), and 39 (2.2%) patients, respectively. Stenosis ranging from 50 to 70%, 70% to 90%, and more than 90% was detected in 196 (11.3%), 286 (16.4%), and 179 (10.3%) cases, respectively.
In the OCAD, the mean age tended to be older (p < 0.001) and more men were observed compared with non-OCAD (p = 0.004) patients. In the OCAD, the prevalence of hypertension, diabetes mellitus, and current smoking was higher (all p < 0.001). However, obesity and family history of CAD were not different between patients with and without OCAD. Patients with OCAD were treated with a higher number of cardiovascular medications except for calcium channel blockers compared with patients manifesting non-OCAD.
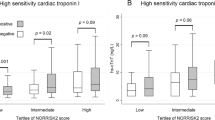
QTc interval and OCAD
There was a significant difference in QTc interval between non-OCAD and OCAD groups (non-OCAD vs. OCAD: 429.0 ± 27.8 vs. 443.5 ± 34.4 ms, p < 0.001). The heart rate on ECG was higher in the OCAD compared with non-OCAD (p < 0.001) patients. The QTc interval was increased according to the degree of stenosis and the number of vessels. The linear trend was statistically significant after adjusting for multiple covariates (all p for linear trend < 0.001) (Fig. 1 and Table 2). The optimal cutoff points of QTc to predict OCAD were 422 and 451 ms in men (AUC, 0.584; confidence interval (CI) 0.543–0.624; P < 0.001) and women (AUC, 0.676; CI 0.648–0.703; P < 0.001), respectively.
Table 3 presents the predictive value of QTc interval for OCAD. The additional predictive values of QTc interval were evaluated incorporating in CAD2 and UDF scores. In the CAD2 model, factors such as age, men, typical chest pain, DM and smoking status were independently associated with OCAD. When QTc interval was included in CAD2 model, it was significantly associated with the presence of OCAD (QTc interval; odd ratio (OR), 1.14; CI 1.09–1.18; P < 0.001, QT prolongation; OR, 2.27; CI 1.81–2.85; P < 0.001). In the UDF model, all components including age, sex and typical chest pain were independently associated with OCAD, and the addition of QTc interval was also significantly associated with OCAD (QTc interval; OR, 1.14; CI 1.10–1.19; P < 0.001, QT prolongation; OR, 2.34; CI 1.87–2.93; P < 0.001).
CAD2 and UDF scores, and new QTc risk score
Based on continuous ROC analysis, the AUC for CAD2 was 0.680 (CI 0.655–0.705), and for UDF it was 0.643 (CI 0.617–0.669). Figure 2 presents the comparison between CAD2, UDF scores and QTc risk score. After incorporating QTc interval as a component of risk score, the new QTc risk score exhibited significantly higher AUC compared with CAD2 score (0.758, CI 0.738–0.781, p < 0.001). The QTc risk score was also associated with a significantly higher AUC compared with UDF score (0.742, CI 0.719–0.766, p < 0.001).
Sex differences in the association of QTc interval and OCAD
The QTc interval was longer in women than in men (439.4 ± 31.6 vs. 424.7 ± 11.6 ms, p < 0.001). Occasionally, OCAD on CAG was significantly more prevalent in men than in women (250, 42.7% vs. 411, 35.6%, p < 0.001). In both men and women, QTc was significantly prolonged in patients diagnosed with OCAD compared with those without OCAD (men; 429.3 ± 31.0 vs. 421.3 ± 25.4 ms, p = 0.001, women; 452.1 ± 33.6 vs 432.4 ± 28.2 ms, p < 0.001).
Figure 1 illustrates the association between QTc interval and the severity of OCAD in men and women. In both sexes, QTc interval was increased according to the degree of stenosis and the number of vessels (all p < 0.001), and this linear trend was more prominent in women compared with men (p for interaction; number: 0.014, stenosis: 0.001).
Risk scores for the evaluation of pre-test probability of OCAD were compared in men and women. In men, AUC of CAD2 and UDF was 0.654 (CI 0.610–0.698) and 0.628 (CI 0.583–0.673). The AUC of QTc risk score was not significantly different compared with CAD2 or UDF. However, in women, the QTc risk score significantly improved AUC of CAD2 from 0.693 (CI 0.662–0.724) to 0.793 (CI 0.766–0.820) (p < 0.001), and AUC of UDF from 0.648 (CI 0.616–0.680) to 0.780 (CI 0.752–0.808) (p < 0.001) (Fig. 3).
Discussion
This is the first study demonstrating the predictive value of QT prolongation for the identification of significant OCAD in patients with suspected angina. The study findings were as follows: (1) The mean value of QTc interval was prolonged in patients with OCAD compared with non-OCAD. (2) The QTc interval was increased linearly according to the severity of OCAD, especially in women. (3) Compared with other pretest probability models, the new score, QTc risk score including QTc interval significantly improved the predictability compared with the traditional risk model such as CAD2 or UDF scores.
Physicians frequently encounter patients presenting with chest pain in the outpatient clinic. In these patients, clinical risk profiling is required and numerous diagnostic strategies exist. The previous risk scores were based on age, sex, typical symptoms and cardiovascular risk factors2,3,4,14,15. The rapid risk scores facilitated the identification of high-risk patients; however, many patients were misdiagnosed. Patients misdiagnosed as non-cardiac chest pain constituted nearly a third of cardiovascular deaths and acute coronary syndromes during follow-up16. Therefore, it is imperative to develop an accurate and effective predictive model for patients with cardiac chest pain.
In the era of multimodality imaging, the role of anatomical imaging and functional testing has been investigated17. Recently, coronary computed tomographic angiography (CCTA) improved the pre-test probability with high accuracy18. However, CCTA is associated with radiation hazards, nephrotoxicity due to contrast agents and high costs1. ECG is the first, simple, cost-effective and universal “bedside” tool for the evaluation of cardiac chest pain1. Among the various parameters of ECG, QTc interval can be easily calculated. Therefore, this study evaluated the incremental predictive value of QTc interval beyond the traditional risk scores.
Acute myocardial ischemia has been reported to increase repolarization heterogeneity of myocardium and prolong the QTc interval11. Several possible mechanisms have been suggested. Because sympathetic and neurohormonal systems are associated with QT prolongation19, the increased catecholamine levels in ischemic myocardium may result in QT prolongation6. Acute myocardial ischemia also alters the myocardial response to catecholamine or cholinergic stimulation, and disturbances associated with potassium or calcium ion channels9,20. Beyond the basic mechanisms, several clinical studies reported the association between myocardial ischemia and QTc interval. Nowinski et al. reported that transient myocardial ischemia during balloon inflation in elective coronary angioplasty induced significant changes in ventricular repolarization represented by increased QT interval21. It suggests that QTc interval may be an early marker of myocardial ischemia. In 206 consecutive patients reporting to the emergency department for acute chest pain, QTc interval correlated with underlying myocardial ischemia based on functional stress test10.
Compared with acute coronary syndrome setting, the role of QTc interval in patients with stable angina has been rarely investigated. In the eighties, Kramer et al. reported the association between the degree of OCAD and QTc interval only in patients with reduced left ventricular function; however, the study, which included a relatively small sample, did not control various factors affecting QTc interval12. More recently, Stankovic et al. demonstrated that QTc interval and myocardial contraction duration on echocardiography were related to the presence of OCAD22. Our findings about QTc interval and OCAD are consistent with previous studies. The study demonstrates that QTc interval is strongly correlated with the presence and severity of OCAD, suggesting the additional probability of QTc interval to detect significant OCAD in prospective-design, real world study population. QT prolongation also predicted the development of clinical outcomes. The QTc interval before angiography was longer in nonsurvivors than in survivors, and development of QTc prolongation was more frequently observed in patients with sudden death (61%) and acute myocardial infarction (26%) than in those with non-cardiac death (0%)23. In patients with chronic ischemic heart disease, QT prolongation was associated with mortality and sudden death24.
Although the current study demonstrated the significant impact of OCAD on QTc interval in women, the underlying pathophysiology has yet to be elucidated. Several possible causes have been suggested. First, diastolic disturbances are the earliest mechanical abnormalities associated with ischemia, and abnormal prolongation of the QTc may be a reflection of these changes25,26. We previously reported that the severity of CAD was associated with left ventricular diastolic dysfunction, which was more predominant in women27. The prominent association between CAD and diastolic dysfunction in women may be one of the mechanisms. Second, increased catecholamine levels and high sympathetic tone are associated with the development of atherosclerosis and left ventricular concentric remodeling28. Therefore, enhanced sympathetic tone and autonomic imbalance are closely linked to QT prolongation6. Decreased estrogen levels accelerate the progression of autonomic neuropathy in post-menopausal women29. Our study demonstrated that the heart rate was much higher in women compared with men, and increased heart rate may be one of the signs underlying increased sympathetic tone, which is linked to QT prolongation in this population with a mean age of about 65 years. An augmented pulsatile load in elderly women may induce pronounced myocardial remodeling, potentially due to sex differences in gene expression of extracellular matrix, and may be the mechanism underlying vulnerable myocardium in women30.
This study is a prospective, nation-wide, multicenter and real-world study with adequate sample size. The study utilizes invasive CAG as a gold standard for the evaluation of the severity of OCAD in all patients. It is hard to decide to proceed further diagnostic management including CAG to identify OCAD in patients with chest pain, particularly in the outpatient clinic. Our study provides an insight into the association between QTc interval and OCAD in patients with suspected angina. The simple measurement of QTc interval facilitates the identification and stratification of patients with severe OCAD. Therefore, the role of QTc interval as a therapeutic marker in ischemia management may be investigated in future studies.
Our study has several limitations. First, QTc interval is variable even in same patients depending on medical conditions such as timing of ECG, cardiovascular medications and comorbidities. However, in this study, ECG was performed in all patients during the first visit to outpatient clinic before CAG. Furthermore, after controlling multivariate covariates including cardiovascular medications, the association between the QTc interval and OCAD was significant. Nonetheless, electrolyte imbalance and the use of certain medications, such as quinolones, which may influence the QTc interval, were not investigated. This is another limitation of the current study. The KoROSE study is an on-going prospective study; therefore, long-term data including the changes in QTc interval and newly developed cardiovascular events will be investigated in future studies. Second, the impact of myocardial ischemia in functional stress test on QTc interval has yet to be evaluated. Finally, the number of women was relatively larger than men in the present study, which may attenuate the association between QT prolongation and OCAD in men.
Conclusion
QT prolongation independently predicted the presence of OCAD and was strongly correlated with the severity of OCAD. The QTc improved model performance to predict OCAD compared with CAD2 or UDF scores in patients with suspected angina and had incremental diagnostic value for the prediction of OCAD as a new risk score.
Methods
Subjects
We included 1829 consecutive patients from the Korean Women’s Chest Pain Registry (KoROSE) who underwent invasive CAG. KoROSE is a prospective, nation-wide, multicenter study enrolling patients with suspected angina visiting outpatient clinic. The protocol of this cohort has been previously described27,31. Consecutive patients who visited 11 tertiary hospitals were registered from January 2012 to May 2018. Exclusion criteria were as follows: structural heart disease, previous myocardial infarction, or any coronary revascularization, chronic kidney disease on dialysis, malignancy, or inflammatory diseases. For accurate evaluation of QTc interval, patients with atrial fibrillation, bundle branch block and pacemaker were additionally excluded. This study was approved by the institutional review boards of Korea University Anam Hospital, Guro Hospital, Ansan Hospital, Seoul National University Boramae Hospital, Chonnam National University Hospital, Gachon Medical School Gil Medical Center, and Hanllym University Chuncheon Sacred Heart Hospital. Written informed consent was obtained from all study subjects. This study was performed in accordance with the declaration of Helsinki.
Clinical, demographics and anthropometrics parameters besides medical history were recorded. Detailed history including clinical presentation of chest pain and physical examination was evaluated by attending physicians. The typicality of chest pain was evaluated according to the clinical guidelines1.
Electrocardiography
ECG was performed using a standard 12-lead ECG recording at 25 mm/s immediately after physical examination. The QT interval was measured from the beginning of the QRS complex until the end of the T wave. Bazett’s formula was used to correct the QT interval for heart rate (QTc interval = QT interval/√RR interval)7. QT prolongation was defined as the best cutoff value indicating OCAD using receiver operating characteristic (ROC) analysis.
Invasive coronary angiography
Using a standard protocol, a skilled clinician performed invasive CAG via radial or femoral artery. OCAD was defined as ≥ 50% stenosis in a proximal or middle epicardial coronary artery, or a major branch. The stenosis of OCAD was classified as 50–70%, 70–90%, and ≥ 90% and based on the number of vessels involved, it was classified into one-, two-, and three-vessel disease.
Risk scores to predict obstructive coronary artery disease
In each subject, the risk scores for the prediction of OCAD were calculated. The UDF score consists of age, sex and typicality of chest pain2. The CAD2 score additionally includes hypertension, diabetes mellitus, dyslipidemia and smoking status3. The new score with QTc prolongation, QTc risk score was calculated using multiple logistic regression analysis of QTc interval along with the components of UDF and CAD2 scores.
Patient and public involvement
Patients and public were not involved in the design, conduct, reporting or dissemination of this research.
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and categorical variables were presented as frequencies (percentages). The clinical differences between sexes were compared using the chi-squared or Student's t-test according to the presence of OCAD. To determine the cutoff value of QTc interval for the prediction of OCAD, a ROC curve analysis was used to estimate sensitivity and specificity. The QTc interval cutoff values were determined based on maximum Youden index (J) in men and women. Multivariate logistic regression analysis was used to investigate the impact of QT prolongation on OCAD after adjustment for age, gender, symptom typicality, cardiovascular risk factors and QT prolongation. We also calculated the predictive power of the 3 scores for OCAD according to the area under the curve (AUC) in each score and compared using the Delong test for paired AUC32. A P value < 0.05 was considered statically significant. IBM SPSS (Version 24, IBM, NY, USA) and R version 3.0.2 (R development core team, Vienna, Austria) were utilized for statistical analysis.
References
Knuuti, J. et al. 2019 ESC Guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 41(3), 407–477 (2020).
Genders, T. S. et al. A clinical prediction rule for the diagnosis of coronary artery disease: Validation, updating, and extension. Eur. Heart J. 32(11), 1316–1330 (2011).
Genders, T. S. et al. Prediction model to estimate presence of coronary artery disease: Retrospective pooled analysis of existing cohorts. BMJ 344, e3485 (2012).
Baskaran, L. et al. A comparison of the updated Diamond-Forrester, CAD Consortium, and CONFIRM history-based risk scores for predicting obstructive coronary artery disease in patients with stable chest pain: The SCOT-HEART Coronary CTA Cohort. JACC Cardiovasc. Imaging. 12(7 Pt 2), 1392–1400 (2019).
Straus, S. M. et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J. Am. Coll. Cardiol. 47(2), 362–367 (2006).
Beinart, R. et al. The QT interval is associated with incident cardiovascular events: The MESA study. J. Am. Coll. Cardiol. 64(20), 2111–2119 (2014).
Bednar, M. M., Harrigan, E. P., Anziano, R. J., Camm, A. J. & Ruskin, J. N. The QT interval. Prog. Cardiovasc. Dis. 43(5 Suppl 1), 1–45 (2001).
Puddu, P. E., Bernard, P. M., Chaitman, B. R. & Bourassa, M. G. QT interval measurement by a computer assisted program: A potentially useful clinical parameter. J. Electrocardiol. 15(1), 15–21 (1982).
Jiménez Candil, J. & Martín, L. C. QT interval and acute myocardial ischemia: Past promises, new evidences. Rev. Esp. Cardiol. 61(6), 561–563 (2008).
Jimenez-Candil, J. et al. Relationship between the QTc interval at hospital admission and the severity of the underlying ischaemia in low and intermediate risk people studied for acute chest pain. Int. J. Cardiol. 126(1), 84–91 (2008).
Stierle, U. et al. Relation between QT dispersion and the extent of myocardial ischemia in patients with three-vessel coronary artery disease. Am. J. Cardiol. 81(5), 564–568 (1998).
Krämer, B., Brill, M., Brühn, A. & Kübler, W. Relationship between the degree of coronary artery disease and of left ventricular function and the duration of the QT-interval in ECG. Eur. Heart J. 7(1), 14–24 (1986).
Arab, D., Valeti, V., Schünemann, H. J. & López-Candales, A. Usefulness of the QTc interval in predicting myocardial ischemia in patients undergoing exercise stress testing. Am. J. Cardiol. 85(6), 764–766 (2000).
Min, J. K. et al. Medical history for prognostic risk assessment and diagnosis of stable patients with suspected coronary artery disease. Am. J. Med. 128(8), 871–878 (2015).
Versteylen, M. O., Joosen, I. A., Shaw, L. J., Narula, J. & Hofstra, L. Comparison of Framingham, PROCAM, SCORE, and Diamond Forrester to predict coronary atherosclerosis and cardiovascular events. J. Nucl. Cardiol. 18(5), 904–911 (2011).
Sekhri, N., Feder, G. S., Junghans, C., Hemingway, H. & Timmis, A. D. How effective are rapid access chest pain clinics? Prognosis of incident angina and non-cardiac chest pain in 8762 consecutive patients. Heart 93(4), 458–463 (2007).
Douglas, P. S. et al. Outcomes of anatomical versus functional testing for coronary artery disease. N. Engl. J. Med. 372(14), 1291–1300 (2015).
SCOT-HEART Investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): An open-label, parallel-group, multicentre trial. Lancet 385(9985), 2383–2391 (2015).
Lindgren, L. et al. Haemodynamic and catecholamine responses to induction of anaesthesia and tracheal intubation: Comparison between propofol and thiopentone. Br. J. Anaesth. 70(3), 306–310 (1993).
De Lorenzo, A. Prolongation of the QT interval and myocardial ischemia are more pieces of the “metabolically unhealthy obesity” puzzle. Am. J. Cardiol. 120(5), 891 (2017).
Nowinski, K., Jensen, S., Lundahl, G. & Bergfeldt, L. Changes in ventricular repolarization during percutaneous transluminal coronary angioplasty in humans assessed by QT interval, QT dispersion and T vector loop morphology. J. Intern. Med. 248(2), 126–136 (2000).
Stankovic, I. et al. Myocardial mechanical and QTc dispersion for the detection of significant coronary artery disease. Eur. Heart. J. Cardiovasc. Imaging. 16(9), 1015–1022 (2015).
Puddu, P. et al. Can the mode of death be predicted in patients with angiographically documented coronary artery disease?. Clin. Cardiol. 6(8), 384–395 (1983).
Puddu, P. E. & Bourassa, M. G. Prediction of sudden death from QTc interval prolongation in patients with chronic ischemic heart disease. J. Electrocardiol. 19(3), 203–211 (1986).
Hauser, A. M., Gangadharan, V., Ramos, R. G., Gordon, S. & Timmis, G. C. Sequence of mechanical, electrocardiographic and clinical effects of repeated coronary artery occlusion in human beings: Echocardiographic observations during coronary angioplasty. J. Am. Coll. Cardiol. 5(2 Pt 1), 193–197 (1985).
Wohlgelernter, D. et al. Regional myocardial dysfunction during coronary angioplasty: Evaluation by two-dimensional echocardiography and 12 lead electrocardiography. J. Am. Coll. Cardiol. 7(6), 1245–1254 (1986).
Cho, D. H. et al. Sex differences in the relationship between left ventricular diastolic dysfunction and coronary artery disease: From the Korean Women’s Chest Pain Registry. J. Womens Health. 27(7), 912–919 (2018).
Curtis, B. M. & O’Keefe, J. H. Jr. Autonomic tone as a cardiovascular risk factor: The dangers of chronic fight or flight. Mayo Clin. Proc. 77(1), 45–54 (2002).
Moodithaya, S. S. & Avadhany, S. T. Comparison of cardiac autonomic activity between pre and post menopausal women using heart rate variability. Indian J. Physiol. Pharmacol. 53(3), 227–234 (2009).
Cheng, S. et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: Longitudinal observations from the Framingham Heart Study. Circulation 122(6), 570–578 (2010).
Cho, D. H. et al. Gender differences in the presentation of chest pain in obstructive coronary artery disease: Results from the Korean Women’s Chest Pain Registry. Korean J. Intern. Med. 35(3), 582 (2020).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics 44(3), 837–845 (1988).
Acknowledgements
We thank all the patients participating in this study.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
D.H.C. participated in analysis of the data, and wrote the manuscript. J.M.C. performed statistical analysis. M.N.K., H.D.K., S.J.H., C.W.Y., H.L.K., Y.H.K., J.O.N., H.J.Y., M.S.S., K.S.H., M.A.K., W.J.S. and S.M.P. participated in recruitment of the patients. S.M.P., W.J.S. designed this study cohort. S.M.P. designed the main conceptual idea, and revised the manuscript for important intellectual content and approved the final version as a primary investigator.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cho, DH., Choi, J., Kim, MN. et al. Incremental value of QT interval for the prediction of obstructive coronary artery disease in patients with chest pain. Sci Rep 11, 10513 (2021). https://doi.org/10.1038/s41598-021-90133-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-90133-6
This article is cited by
-
QTc interval prolongation impact on in-hospital mortality in acute coronary syndromes patients using artificial intelligence and machine learning
The Egyptian Heart Journal (2024)
-
The optimal QTc selection in patients of acute myocardial infarction with poor perioperative prognosis
BMC Cardiovascular Disorders (2023)