Abstract
Blastocystis hominis and Cystoisospora belli are considered to be common opportunistic intestinal protozoa in HIV/AIDS patients. In order to investigate the prevalence and genetic characteristics of B. hominis and C. belli in HIV/AIDS patients, a total of 285 faecal samples were individually collected from HIV/AIDS patients in Guangxi, China. B. hominis and C. belli were investigated by amplifying the barcode region of the SSU rRNA gene and the internal transcribed spacer 1 (ITS-1) region of the rRNA gene, respectively. Chi-square test or Fisher’s exact test were conducted to assess the risk factors related to B. hominis and C. belli infection. The prevalence of B. hominis and C. belli was 6.0% (17/285) and 1.1% (3/285) respectively. Four genotypes of B. hominis were detected, with ST3 (n = 8) and ST1 (n = 6) being predominant, followed by ST6 (n = 2) and ST7 (n = 1). Females had a statistically higher prevalence of B. hominis (11.6%) than males (4.2%). The statistical analysis also showed that the prevalence of B. hominis was significantly associated with age group and educational level. Our study provides convincing evidence for the genetic diversity of B. hominis, which indicates its potential zoonotic transmission and is the first report on the molecular characteristics of C. belli in HIV/AIDS patients in China.
Similar content being viewed by others
Introduction
Globally, HIV infection is an important public health problem. There were approximately 37.6 million people infected with HIV and 1.5 million newly infected worldwide according to the Joint United Nations Programme on HIV/AIDS (UNAIDS) by the end of 20201. In China, the epidemiological status of HIV is alarming, posing tremendous challenges for its control and prevention. It was reported that approximately 9,58,000 people live with HIV by the end of October in 2019 with 1,31,000 new infection from January to October2. It is estimated that about 1.1 million people die of AIDS every year, and of which 80% death due to AIDS-related infections3. Because of the downregulated immune system of HIV-infected patients, they are highly susceptible to opportunistic pathogens, such as viruses, bacteria, and parasites, of which intestinal parasites are particularly common in HIV-infected patients4,5. Diarrhea caused by such intestinal parasites weakens the absorption of antiretroviral drugs and causes nutritional absorption disorders; both exacerbate the condition of HIV/AIDS patients and lower their quality of life3,6.
Blastocystis hominis, a globally distributed intestinal parasite, was first detected in a human faecal sample in 1911 and mainly parasitizes the large intestine of humans, causing various gastrointestinal symptoms including nausea, abdominal pain, diarrhea, and flatulence, and occasional parenteral symptoms7,8. It is estimated that about one billion people in the world are infected with B. hominis, whose prevalence is much higher in developing countries (30.0%–100.0%) than in developed countries (1.5%–20.0%)9,10,11. To date, B. hominis harbours at least 26 genotypes, of which 10 genotypes, namely ST1–ST9 and ST12, have been found in humans12,13,14. ST3 is reportedly the most common genotype that causes gastrointestinal symptoms13. Although the prevalence of B. hominis in HIV/AIDS patients has been reported worldwide, the genetic diversity of B. hominis in HIV/AIDS patients is rarely documented by empirical data. So far, just three studies of B. hominis in HIV/AIDS patients have been carried out in Anhui, Hunan, and Yunnan provinces, China, for which the prevalence of B. hominis was 16.2%, 9.9%, and 3.7%, respectively14.
Cystoisospora belli (formerly Isospora belli), originally described by Zaman in 196815, also has a global distribution but it is more common in tropical and subtropical countries, such as India, Nigeria, and Ethiopia16. Importantly, C. belli has been frequently detected in patients with HIV, Human T-lymphotropic Virus Type I (HLTLV1), Alzheimer’s disease, and colorectal cancer, as well as those having undergone liver and renal transplantation17,18,19,20. In those HIV/AIDS patients with diarrhea symptoms, the prevalence of C. belli could reach up to 20%21. Although it occurs worldwide, C. belli is a generally overlooked parasite, and one not well studied in China. Hence, further study of this parasite is imperative.
Several cluster studies of B. hominis and C. belli in HIV/AIDS patients have been conducted, especially in low- and middle-income countries16,22,23. But, surprisingly, comparable reports are quite limited for China, especially for C. belli. To our best knowledge, the molecular study presented here is the first on this parasite in China.
Guangxi Zhuang Autonomous Region (hereon Guangxi), a provincial-level autonomous region, is located in southern China and borders Vietnam in the southwest. It has a subtropical monsoon climate with abundant rainfall and light. In 2020, the total population of the registered residence in Guangxi was ~ 50 million. It has been reported that the prevalence of HIV/AIDS in Guangxi was 6.6% in 2013, 8.4% in 2014, and 11.2% in 2015, all of which were higher than the corresponding numbers for the general population in China (0.05%)24,25. Furthermore, by the end of 2017, Guangxi had reported 124,282 cases of HIV/AIDS, indicating an increase of 78.7% since June 2011 (69,548 cases) and ranking it as second in terms of HIV seropositive cases among the 31 provinces of China26,27. Since the Guangxi leads this country in the number of HIV/AIDS patients, investigating their intestinal parasites is of great public health significance28. In our previous research, Microsporidia, Cryptosporidium, and Giardia were respectively detected with prevalence of 11.6%, 0.7%, and 2.8% in those participants5,29,30. Both B. hominis and C. belli are recognized as the pathogens that most often cause opportunistic infections in HIV/AIDS patients, posing a prominent threat to the public health13,16. Accordingly, the present study aimed to assess the prevalence in addition to genetic characteristics and risk factors of B. hominis and C. belli in HIV/AIDS patients of Guangxi, China.
Methods
Ethics approval and consent to participate
The present study obtained the approval from the Ethics Committee of the National Institute of Parasitic Diseases, Chinese Centre for Disease Control and Prevention (reference no. 2012–12) and all methods were conducted in accordance with the relevant guidelines and regulations as provided in the Declaration of Helsinki. All the patients enrolled in the study were given an oral explanation of the objectives, procedures and potential risks for collection of their faecal samples. Adult participants signed the written informed consent personally. All participants were over the age of 20, so no parental consent was required.
Sample size calculation
Due to the lack of prevalence of C. belli in China, the sample size was calculated based on the prevalence of B. hominis. The required sample sized was determined using the formula31:\(n = \frac{{{\rm Z}_{\alpha }^{2} p\left( {1 - p} \right)}}{{^{{\delta^{2} }} }}\), where \(\alpha\) = 0.05, \(\delta\) = 0.05, and \(p\) = the estimated prevalence of B. hominis among HIV/AIDS patients, which was taken as 16.2%32. The resulting sample size was 209 patients. Considering that an estimated 10% of the patients might fail to participate in the study, the final sample size was increased to 230 patients. Finally, a total of 285 HIV/AIDS patients registered in nine hospitals in Guangxi were enrolled into the present study.
Questionnaire, faecal sample collection, and processing
From July 2013 to July 2014, fresh faecal samples (one per patient) were collected, with an in-person, structured questionnaire survey conducted face-to-face to collect the patients’ demographic information (gender, age, education level, occupation), behavioral information (whether drinking boiled water or not, whether receiving HAART treatment or not), HIV transmission route, clinical symptoms (diarrhea), and CD4+ cell count.
The collected fresh faecal samples (≥ 200 mg) were first stored at 4 °C with 2.5% potassium dichromate, and then sent to the laboratory of National Institute of Parasitic Diseases, Chinese Centre for Disease Control and Prevention. There, all samples were washed three times with deionized water at 14 000 rpm for 10 min, to remove the potassium dichromate. Then, DNA was extracted from 180 to 220 mg of each faecal sample, by using QIAamp DNA Stool Mini Kit (Qiagen, Hilden, Germany) and following the manufacturer’s instructions. For a higher DNA yield, the lysis temperature was adjusted to 95 °C according to the manufacturer’s recommendation. The final amount of DNA was 200 μl per sample, stored at –30 °C until the PCR analysis.
Detection of B. hominis and C. belli
PCR was used to amplify the barcode region of the SSU rRNA gene of B. hominis, using primer sets as described by Scicluna33, while C. belli was detected with the primer sets based on the ITS-1 region of the rRNA gene designed by Reza et al.17. All DNA samples were analyzed at least three times. Either B. hominis-positive DNA or C. belli-positive DNA and nuclease-free water served as the positive and negative controls, respectively. The PCR products (5 μl) were checked by 2% gel electrophoresis, and the products of an expected size (approximately 600 bp for B. hominis and 450 bp for C. belli) were analyzed using an ABI 3730 DNA Analyzer and Big Dye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems). ContigExpress program, a component of the Vector NTI Suite 6.0 (https://www.winsite.com/vector /vector + nti/) was used for sequence assembly and wave peak evaluation. The sequences obtained were searched using the BLAST tool (https://blast.ncbi.nlm.nih. gov/Blast.cgi/) in GenBank databases and aligned with representative sequence of B. hominis or C. belli, respectively.
Phylogenetic and statistical analysis
Phylogenetic trees for B. hominis and C. belli were constructed in MEGA 6.0 (http://mega.software.net), based on 1000 bootstrap replicates, using the sequences obtained in this study and representative sequences downloaded from NCBI.
SPSS V20.0 software (https://spss.en.softonic.com/) was used to statistically analyze the data. Chi-square test or Fisher’s exact test was implemented to compare the prevalence between groups classified by gender, age, education level, occupation, whether drinking boiled water or not, whether receiving HAART treatment or not, HIV transmission route, diarrhea, and CD4+ cell count. Differences were regarded as statistically significant at P < 0.05.
Results
Basic information of the study participants
Of the 285 HIV/AIDS patients enrolled, 75.8% (216/285) were males and 24.2% (69/285) were females. Most were farmers (76.1%, 217/285). Patients with a high school and above education accounted for 43.5% (124/285) of the population sample, followed by junior high school (43.2%, 123/285), and then primary school and below (13.3%, 38/285). Of the 285 individuals surveyed, 168 were tested for CD4+ cell counts: 29.2% (49/168) had a count ≥ 200, while for the majority (70.8%; 119/168) the count was less than 200. Basic information of this study population appears in Table 1.
Prevalence of B. hominis and C. belli
Overall, the prevalence of these two parasites was 6.7% (19/285); 5.1% (11/216) of males and 11.6% (8/69) of females were positive for at least one of the two protozoan species. Considering B. hominis, its general prevalence was 6.0% (17/285), being 4.2% (9/216) in males and 11.6% (8/69) in females. Among these 17 cases of B. hominis infection, 10 cases underwent the CD4+ cell count test whereas the other 7 did not. The prevalence of B. hominis was 5.9% (7/119) in those patients with a CD4+ cell count < 200 and 6.1% (3/49) in those with a count ≥ 200. Diarrhea symptoms were self-reported in 2 of the 17 cases of B. hominis infection (Table 1).
The prevalence of C. belli was 1.1% (3/285), and all the three infected individuals were males. Moreover, co-infection of C. belli with B. hominis was observed in a farmer aged 50 who had bacterial pneumonia.
Analysis of risk factors of B. hominis and C. belli
All 285 participants properly completed the survey questionnaire. They were divided into different groups by gender, age, education level, occupation, whether drinking boiled water or not, whether receiving HAART treatment or not, HIV transmission route, diarrhea, and CD4+ cell count. Univariate analysis revealed that three factors were associated with B. hominis infection in HIV/AIDS patients: gender (χ2 = 3.904, P = 0.048), age (χ2 = 8.443, P = 0.015), and educational level (χ2 = 51.944, P = 0.000). By contrast, the remaining risk factors tested were not associated with patients’ infection of B. hominis (all P-values > 0.05; Table 1).
Univariate analysis showed a statistically significant correlation between the prevalence of C. belli and different education levels (P = 0.002). No significant differences, however, were found between groups formed by other risk factors (all P-values > 0.05; Table 1).
Molecular characteristics of B. hominis and C. belli
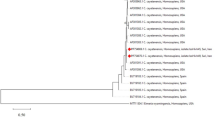
According to the sequence analysis of 17 B. hominis isolates, four genotypes were identified: ST3 (47.0%, n = 8), ST1 (35.3%, n = 6), ST6 (11.8%, n = 2) and ST7 (5.9%, n = 1) (Table 2). Among sequences obtained here, four novel sequences identified as ST1 shared a high identity (99.3%) to the sequence previously identified from chicken (AB070993). The remaining ST1 and ST3 isolates showed 100% homology with other known isolates: namely for ST1, KY681140 (human) and MF186699 (goat); for ST3, KX618192 (human), MH784407 (human), MN658570 human), MT042796 (human), MT042789 (human) and KT438691 (human). The ST6 and ST7 sequences were respectively identical to the known reference sequences KY964514 (turkey) and KF447169 (human) (Fig. 1).
Phylogenetic tree of Blastocystis hominis based on the barcode region of the SSU rRNA gene sequence. MEGA 6.0 software (http://www.megasoftware.net/) was used for this analysis, by applying the neighbor-joining distance method with 1000 bootstrap replicates. Individual GenBank accession numbers precede localities, followed by hosts and genotypes. The numbers on the branches are percentage bootstrapping values from 1000 replicates. The scale-bars indicate the number of substitutions per site. Squares indicate B. hominis identified from faecal DNA samples in this study.
The sequences of the three C. belli isolates showed 100% homology with isolates (HM630352) previously identified from an HIV/AIDS patient in Argentina (Fig. 2).
Phylogenetic tree of Cystoisospora belli based on the ITS-1 region of rRNA gene sequences. This tree was constructed by the neighbor-joining distance method with 1000 bootstrap replicates, in MEGA 6.0 software (http://www.megasoftware.net/). Individual GenBank accession numbers precede localities, followed by hosts and species. The numbers on the branches are percentage bootstrapping values from 1000 replicates. The scale-bars indicate the number of substitutions per site. Squares represent C. belli sequences from this study.
Discussion
Blastocystis hominis and C. belli are common, opportunistic intestinal protozoa in immunocompromised individuals, especially in HIV/AIDS patients. We determined that the overall prevalence of both species was 6.7% (19/285), with B. hominis at least fivefold more prevalent (6.0%, 17/285) than C. belli (1.1%, 3/285). As far as we know, this is the first molecular investigation of B. hominis in HIV/AIDS patients in Guangxi, China, and of C. belli in China.
Blastocystis hominis is found globally, but its prevalence in HIV/AIDS patients among countries varies tremendously, from 0.9 to 72.4%4. A higher prevalence that reached 88.7% was observed in indigenous children from the Colombian Amazon Basin34. Due to the controversial pathogenicity of B. hominis, less attention has been paid to it than to Cryptosporidium, Giardia and Microsporidia in China. Nevertheless, a waterborne outbreak of B. hominis in China that afflicted 1122 people highlighted the public health significance of this intestinal parasite35. Therefore, detection of B. hominis is imperative in China.
Generally, few studies of B. hominis relying on molecular approaches have been conducted in China. Genotypes of B. hominis were analyzed in seven provinces, cities or autonomous regions—Heilongjiang, Guangxi, Yunnan, Zhejiang, Shanghai, Xinjiang and Chongqing—among different population groups, for which its prevalence ranged from 3.7% to 36.6%14,36,37,38,39,40,41,42,43,44,45,46,47(Table 3). We found an occurrence of B. hominis in HIV/AIDS patients of 6.0%, lower than that in Fuyang, Anhui Province (16.2%)48, yet slightly higher than that in Tengchong, Yunnan Province (3.7%)14. In other countries, a higher prevalence of B. hominis in HIV/AIDS patients was reported for Peru (24.6%)49, Rome (25.0%)50, Bogota (25.2%)51 and Indonesia (72.4%)4, whereas lower values characterized Nepal (0.9%)52 and India (3.3%)53. Such disparate infection rates may arise from multiple factors, including the research scope, the selected subjects, their living environment as well as local social, economic, and cultural conditions. For example, low socio-economic conditions coupled to a humid and high temperature climate can increase the transmission of B. hominis54. In addition, diagnostic methods differ in their sensitivity and specificity in detecting B. hominis. Molecular approaches based on PCR were shown to be superior to traditional microscopic examination of faecal samples55. In southwestern Iran, B. hominis occurred in 12.3% and 19.0% of humans according to the Formol-Ether technique and PCR, respectively56. In another study of newly arrived immigrants in Qatar, the prevalence of B. hominis was 7.6% when assessed by coproscopic methods but much higher (65.2%) by RT-PCR57. In other work, in HIV-infected patients, microscopic examination suggested a B. hominis prevalence of 21.8% but according to PCR it was 25.0%50.
In line with the study conducted in Fuyang, Anhui Province, China48, we found that women were more likely to get infected with B. hominis than men. Differences in nutritional status and access to medical facilities between men and women may be responsible for the increased risk of parasite infection among women58. Individuals with an education level of primary schools and below have the highest infection rate of B. hominis in Guangxi, hence a limited education and poor awareness of hygiene may contribute to the high infection rate in specific groups. Prevalence in patients grouped by occupation, CD4+ cell count, HIV transmission route, and whether they were receiving HAART treatment or not, all showed no statistical differences. Previous studies suggested that people with a CD4+ cell count less than 200 are more susceptible to B. hominis56, and that drinking raw (untreated) water can increase its infection risk45. Moreover, three waterborne outbreaks of B. hominis have been reported22,35, but in the present study the prevalence was similar between boiled water drinkers and raw water drinkers. This result may have two explanations. First, there is no B. hominis in the water of this area; second, the ratio of boiled water drinkers was high, accounting for 93.3%.
Currently, the pathogenicity of B. hominis remains contentious, as the parasite has been detected in symptomatic and asymptomatic individuals. In the former, diarrhea, abdominal pain, irritable bowel syndrome, constipation, and flatulence are usually reported7,8. Mounting evidence shows immunocompromised individuals are more likely to suffer gastrointestinal symptoms related to B. hominis. A study performed in cancer patients in China uncovered a significant association between B. hominis infection and diarrhea37. Similarly, for HIV-infected patients positive association between B. hominis infection and flatulence was demonstrated50. A variety of clinical symptoms could be related to different B. hominis genotypes that can excrete different protease enzymes59. For example, Poirier et al. showed that ST7 may be responsible for irritable bowel syndrome60, while in Iran ST3 may be associated with gastrointestinal disorder61. Although ST3 was the predominant genotype identified in our study, no statistical association was observed between B. hominis infection and diarrhea.
Presently, B. hominis is known to harbour at least 26 genotypes11,12. Ten genotypes (ST1–ST9 and ST12) were found in humans, among which ST3 was the most common37. The ST1–ST8 have been identified both in humans and various animals, highlighting their capability for zoonotic transmission12,13,14. We know of nine genotypes of B. hominis detected so far in HIV/AIDS patients worldwide: ST1–ST7, ST9 and ST1214,36,45,50,56,62,63,64 (Table 4). In our study, four genotypes of B. hominis were identified—ST1, ST3, ST6 and ST7—with ST3 the dominant one (47.1%; 8/17), a result consistent with that of studies in HIV/AIDS patients in southwestern Iran and cancer patients in China37,56. All the genotypes have zoonotic potential according to the latest research: both ST1 and ST3 are considered the most abundant genotypes 13,56 and are widely associated with animals, such as non-human primates, dogs and pigs65,66. ST6, detected in indigenous children in the Colombian Amazon Basin34, and ST7, detected in HIV/AIDS patients in China’s Yunnan Province and in Iran14,64, have been identified from cattle, rodents, birds, chickens, and pigs65,66. Additionally, B. hominis is viewed as a waterborne pathogen, given its identification in different water bodies including river, wastewater, drinking water, school ponds, and canal water and the three waterborne outbreaks of B. hominis infection documented in Italy, China, and Nepal that drew garnered attention to this parasite22. Hence, future research should focus on investigating the prevalence and genetic diversity of B. hominis in both animals and water in our study area to better understand its transmission dynamics.
The prevalence of C. belli in HIV/AIDS patients varies from country to country, even so within the different areas of the same region16. Infection by C. belli happens worldwide, especially in tropical and subtropical regions such as India, Iran, Brazil and Ethiopia, but mostly these were sporadic cases or small aggregate outbreaks16,17,21. Here, in Guangxi, C. belli was detected in three participants, at a prevalence of 1.1%, which is close to that reported for HIV/AIDS patients in Ethiopia (1.3%) 67, but lower than that of HIV/AIDS patients in India (16.5%)68 and higher than of patients in Burkina Faso (0.7%)69. Severe diarrhea due to C. belli infection has been reported in immunocompromised patients17,70. Contrary to our expectation, the three C. belli-infected individuals all reported no diarrhea symptoms. In this study, non-diarrheal individuals accounted for 89.8% (256/285) of the sampled population, which may induce the low prevalence, given that patients with diarrhea often show a high prevalence of C. belli (25.0%)71.
Here we found that people with a primary school and below education level were more prone to infection by this protist. Yet no statistical link was discernable between its prevalence and the many other risk factors examined. Similarly, a study in Nigeria also could not link isosporiasis to either the gender or age of hosts 72.
Conclusions
The present study revealed the prevalence, genetic characteristics, and risk factors of B. hominis and C. belli in HIV/AIDS patients in Guangxi, China. Our data indicated the zoonotic transmission of B. hominis in this area and relationships between B. hominis infection and gender, age, and educational level. Furthermore, our study provided new insight into the molecular characteristics of C. belli, providing the first molecular data for this parasite in China. Future studies should be focus on investigating B. hominis and C. belli in animals and water in the Guangxi area to figure out the sources and routes of these protozoans’ transmission.
Data availability
The datasets generated and/or analysed during the current study are not publicly available in order to protect participant confidentiality. The gene sequences identified in this study were submitted to GenBank with accession numbers MK922974, MK930346, MK930362, MK934329-MK934342, and MK935345-MK935347.
References
United Nations Programme on HIV/AIDS Global HIV/AIDS statistics: 2020 fact sheet. Available from https://www.unaids.org/en/resources/fact-sheet.
He, N. Emerging changes and characteristics of the HIV epidemic in China [in Chinese]. Shanghai. J. Prev. Med. 31, 963–967 (2019).
Smith, P. D. et al. Intestinal infections in patients with the acquired immunodeficiency syndrome (AIDS). Etiology and response to therapy. Ann. Int. Med. 108, 328–333 (1988).
Kurniawan, A. et al. Intestinal parasitic infections in HIV/AIDS patients presenting with diarrhoea in Jakarta Indonesia. Trans. R. Soc. Trop. Med. Hyg. 103, 892–898 (2009).
Liu, H. et al. Infection by and genotype characteristics of Enterocytozoon bieneusi in HIV/AIDS patients from Guangxi Zhuang autonomous region China. BMC. Infect. Dis. 17, 684–692 (2017).
Eshetu, T. et al. Intestinal parasitosis and their associated factors among people living with HIV at university of Gondar hospital Northwest-Ethiopia. Ethiop. J. Health. Sci. 27, 411–420 (2017).
Ibarra, C. et al. Parasitosis and irritable bowel syndrome. Rev. Chilena. Infectol. 33, 268–274 (2016).
Ibrahim, A. N., Al-Ashkar, A. M. & Nazeer, J. T. Additional glance on the role of Dientamoeba fragilis & Blastocystis hominis in patients with irritable bowel syndrome. Iran. J. Parasitol. 13, 100–107 (2018).
Parija, S. C. & Jeremiah, S. Blastocystis: Taxonomy, biology and virulence. Trop. Parasitol. 3, 17–25 (2013).
Abdulsalam, A. M. et al. Subtype distribution of Blastocystis isolates in Sebha Libya. PLoS ONE 8, e84372 (2013).
El, S. D. et al. Children of senegal river basin show the highest prevalence of Blastocystis sp ever observed worldwide. BMC. Infect. Dis. 14, 164 (2014).
Maloney, J. G., Lombard, J. E., Urie, J. N., Shivley, C. B. & Santin, M. Zoonotic and genetically diverse subtypes of Blastocystis in US pre-weaned dairy heifer Calves. Parasitol. Res. 118, 575–582 (2019).
Barbosa, C. V. et al. Intestinal parasite infections in a rural community of Rio de Janeiro (Brazil): Prevalence and genetic diversity of Blastocystis subtypes. PLoS ONE 13, e0193860 (2018).
Teng, X. J. et al. The epidemiological characteristics and influencing factors for Blastocystis hominis infection among human immunodeficiency virus seropositive individuals in Tengchong of Yunnan Province. Chin. J. Parasitol. Parasit. Dis. 36, 129–134 (2018).
Zaman, V. Observations on human Isospora. Trans. R. Soc. Trop. Med. Hyg. 62, 556–557 (1968).
Wang, Z. D. et al. Prevalence of Cryptosporidium, Microsporidia and Isospora infection in HIV-infected people: a global systematic review and meta-analysis Parasit. Vectors 11, 28 (2018).
Shafiei, R., Najjari, M., Kargar, K. A. & Hatam, G. Severe diarrhea due to Cystoisospora belli infection in an HTLV-1 woman. Iran. J. Parasitol. 11, 121–125 (2016).
Usluca, S., Inceboz, T., Unek, T. & Aksoy, U. Isospora belli in a patient with liver transplantation. Turkiye. Parazitol. Derg. 36, 247–250 (2012).
Ünal, N. et al. Isosporiasis in an elderly patient with chronic diseases: case report. Turkiye. Parazitol. Derg. 37, 222–224 (2013).
Mahmoudvand, H., Sepahvand, A., Khatami, M. & Moayyedkazemi, A. Prevalence and associated risk factors of Cystoisospora belli and Cyclospora cayetanensis infection among Iranian patients with colorectal cancer. J. Parasit. Dis. 43, 402–405 (2019).
Marcos, L. A. & Gotuzzo, E. Intestinal protozoan infections in the immunocompromised host. Curr. Opin. Infect. Dis. 26, 295–301 (2013).
Plutzer, J. & Karanis, P. Neglected waterborne parasitic protozoa and their detection in water. Water Res. 101, 318–332 (2016).
Teng, X. J., Chen, J. X. & Tian, L. G. Epidemic status of HIV/AIDS with intestinal protozoa infection. Chin. J. Parasitol. Parasit. Dis. 6, 607–614 (2017).
Lan, G. H. et al. HIV, syphilis and behavioral risk factors among men who have sex with men in a drug-using area of southwestern China. Medicine (Baltimore) 97, e0404 (2018).
China MOH, UN AIDS & WHO. HIV/AIDS epidemic estimation in China, 2011 [in Chinese]. Chin. J. AIDS. STD. 14: 1–5 (2012).
Zhao, T. T. et al. Cognitive disorders in HIV-infected and AIDS patients in Guangxi China. J. Neurovirol. 21, 32–42 (2015).
Yang, X. Y. et al. Immunological and virologic outcomes of people living with HIV in Guangxi, China: 2012–2017. PLoS ONE 14, e0213205 (2019).
Wu, Z. Y. China’s AIDS Prevention and treatment faces new situation and new challenges. Chin. J. Public. Health. 27, 1505–1507 (2011).
Wang, Z. F. et al. Preliminary study on infection status and gene types of Cryptosporidium among HIV/AIDS patients in Guangxi. Chin. J. Schisto. Control. 28, 550–553 (2016).
Liu, H., Xu, N., Shen, Y. J., Hu, Y. & Cao, J. P. Infection and genotype of Giardia lamblia among HIV/AIDS patients in Guangxi. Chin. J. Parasitol. Parasit. Dis. 37, 321–325 (2019).
Nsagha, D. S. et al. Intestinal parasitic infections in relation to CD4(+) T cell counts and diarrhea in HIV/AIDS patients with or without antiretroviral therapy in Cameroon. BMC. Infect. Dis. 16, 9 (2016).
Tian, L. G. et al. Co-infection of HIV and intestinal parasites in rural area of China. Parasit. Vectors. 5, 36 (2012).
Scicluna, S. M., Tawari, B. & Clark, C. G. DNA barcoding of blastocystis. Protist 157, 77–85 (2006).
Sánchez, A. et al. Molecular epidemiology of Giardia, Blastocystis and Cryptosporidium among indigenous children from the Colombian Amazon Basin. Front. Microbiol. 8, 248 (2017).
Wu, G. H. et al. Investigation of an epidemic outbreak of blastocystiasis. Chin. J. Parasitic. Dis. Control. 13, 25–27 (2000).
Li, L. H. et al. Molecular epidemiology of human Blastocystis in a village in Yunnan province China. Parasitol. Int. 56, 281–286 (2007).
Zhang, W. Z. et al. Genotyping of Enterocytozoon bieneusi and subtyping of Blastocystis in Cancer Patients: relationship to diarrhea and assessment of zoonotic transmission. Front. Microbiol. 8, 1835 (2017).
Zhan, T. Z. et al. PCR-based genotype classification of Blastocystis hominis isolates from college students of Guangxi. Chin. J. Parasitol. Parasit. Dis. 32, 209–211 (2014).
Yan, Y. M. et al. Genetic variability of Blastocystis hominis isolates in China. Parasitol. Res. 99, 597–601 (2006).
Zhang, S. X. et al. Epidemiological characteristics of Blastocystis hominis in urban region, southwestern China. Chin. J. Zoonoses. 32, 424–428 (2016).
Yu, Y., Wu, X. P., Chu, Y. H., Zhang, Y. N. & Tian, L. G. A case of Blastocystis hominis (subtype 3) infection confirmed by PCR and in vitro culture. Chin. J. Parasitol. Parasit. Dis. 33, inside back cover (2015).
Zhan, T. Z., Shi, H. H., He, S. S. & Liu, T. Genotype analysis and isoenzyme patterns of ten isolates of Blastocystis hominis from Guangxi. Chin. J. Parasitol. Parasit. Dis. 30, 36–40 (2012).
Li, L. H. et al. Cross-sectional surveys and subtype classification of human Blastocystis isolates from four epidemiological settings in China. Parasitol. Res. 102, 83–90 (2007).
Gong, B. Y. et al. Prevalence and subtype distribution of Blastocystis in ethnicminority groups on both sides of the China-Myanmar border, and assessment of risk factors. Parasite 26, 46 (2019).
Zhang, S. X., Kang, F. Y., Chen, J. X., Tian, L. G. & Geng, L. L. Risk factors for Blastocystis infection in HIV/AIDS patients with highly activeantiretroviral therapy in Southwest China. Infect. Dis. Poverty. 8, 89 (2019).
Qi, M. et al. Genetic diversity of Blastocystis in kindergarten children in southern Xinjiang China. Parasit. Vectors. 13, 15 (2020).
Kang, J. M. et al. Prevalence and risk factors of Blastocystis hominis infection in inpatients in Jiangjin District Chongqing City. Chin. J. Schisto. Control. 31, 479–485 (2019).
Tian, L. G. et al. Survey on Blastocystis hominis infection in HIV positive individuals in Fuyang City Anhui Province. Chin. J. Schisto. Control. 24, 303–306 (2012).
Chincha, O. et al. Parasite intestinal infection and factors associated with coccidian infection in adults at public hospital in Lima Peru. Rev. Chilena. Infectol. 26, 440–444 (2009).
Sulekova, F. L. et al. Molecular characterization of Blastocystis subtypes in HIV-positive patients and evaluation of risk factors for colonization. BMC. Infect. Dis. 19, 876 (2019).
Flórez, A. C., García, D. A., Moncada, L. & Beltrán, M. Prevalence of microsporidia and other intestinal parasites in patients with HIV infection, Bogota, 2001. Biomedica. 23, 274–282 (2003).
Ghimire, A. et al. Enteric parasitic infection among HIV-infected patients visiting Tribhuvan University Teaching Hospital Nepal. BMC. Res. Notes. 9, 204 (2016).
Mohandas, S. R., Sud, A. & Malla, N. Prevalence of intestinal parasitic pathogens in HIV-seropositive individuals in Northern India. Jpn. J. Infect. Dis. 55, 83–84 (2002).
Javanmard, E. et al. Impacts of human development index and climate conditions on prevalence of Blastocystis: A systematic review and meta-analysis. Acta. Trop. 185, 193–203 (2018).
Won, E. J. et al. Multiplex real-time PCR assay targeting eight parasites customized to the Korean population: potential use for detection in diarrheal stool samples from gastroenteritis patients. PLoS ONE 11, e0166957 (2016).
Piranshahi, A. R., Tavalla, M. & Khademvatan, S. Genomic analysis of Blastocystis hominis isolates in patients with HIV-positive using locus SSU-rDNA. J. Parasit. Dis. 42, 28–33 (2018).
Abu-Madi, M., Boughattas, S., Behnke, J. M., Sharma, A. & Ismail, A. Coproscopy and molecular screening for detection of intestinal protozoa. Parasit. Vectors. 10, 414 (2017).
Kaur, V. Tropical diseases and women. Clin. Dermatol. 15, 171–178 (1997).
Kurt, Ö., Doğruman Al, F. & Tanyüksel, M. Eradication of Blastocystis in humans: really necessary for all?. Parasitol. Int. 65, 797–801 (2016).
Poirier, P., Wawrzyniak, I., Vivarès, C. P., Delbac, F. & ElAlaoui, H. New insights into Blastocystis spp.: a potential link with irritable bowel syndrome. PLoS Pathog. 8, e1002545 (2012).
Khademvatan, S. et al. PCR-based molecular characterization of Blastocystis hominis subtypes in southwest of Iran. J. Infect. Public. Health. 11, 43–47 (2018).
Di Cristanziano, V. et al. Lower prevalence of Blastocystis sp infections in HIV positive compared to HIV negative adults in Ghana. PLoS ONE 14, e0221968 (2019).
Tan, T., Ong, S. C. & Suresh, K. G. Genetic variability of Blastocystis sp isolates obtained from cancer and HIV/AIDS patients. Parasitol. Res. 105, 1283–1286 (2009).
Khoshnood, S., Rafiei, A., Saki, J. & Alizadeh, K. Prevalence and genotype characterization of Blastocystis hominis among the Baghmalek people in southwestern Iran in 2013–2014. Jundishapur. J. Microbiol. 8, e23930 (2015).
Stensvold, C. R. et al. Subtype distribution of Blastocystis isolates from synanthropic and zoo animals and identification of a new subtype. Int. J. Parasitol. 39, 473–479 (2009).
Iguchi, A. et al. Infectivity of different genotypes of human Blastocystis hominis isolates in chickens and rats. Parasitol. Int. 56, 107–112 (2007).
Kiros, H., Nibret, E., Munshea, A., Kerisew, B. & Adal, M. Prevalence of intestinal protozoan infections among individuals living with HIV/AIDS at Felegehiwot Referral Hospital, Bahir Dar Ethiopia. Int. J. Infect. Dis. 35, 80–86 (2015).
Dash, M., Padhi, S., Panda, P. & Parida, B. Intestinal protozoans in adults with diarrhea. N. Am. J. Med. Sci. 5, 707–712 (2013).
Sangaré, I. et al. Prevalence of intestinal opportunistic parasites infections in the University hospital of Bobo-Dioulasso Burkina Faso. Infect. Dis. Poverty. 4, 32 (2015).
Marathe, A. & Parikh, K. Severe diarrhoea due to Cystoisospora belli in renal transplant patient on immunosuppressive drugs Indian. J. Med. Microbiol. 31, 185–187 (2013).
Casmo, V., Lebbad, M., Maungate, S. & Lindh, J. Occurrence of Cryptosporidium spp. and Cystoisospora belli among adult patients with diarrhoea in Maputo. Mozambique. Heliyon. 4, 769 (2018).
Olusegun, A. F., Okaka, C. E. & Luiz, D. M. R. Isosporiasis in HIV/AIDS patients in Edo State Nigeria. Malays. J. Med. Sci. 16, 41–44 (2009).
Acknowledgements
We thank the staff at the Guangxi Zhuang Autonomous Region Center for Disease Control and Prevention for their assistance with the samples’ collection and case investigations.
Funding
This work was supported by the Fifth Round of Three-Year Public Health Action Plan of Shanghai (No. GWV-10.1-XK13 to JC), the National Science and Technology Major Program of China (No. 2018ZX10713001-004 to YS), and the Chinese Special Program for Scientific Research of Public Health (No. 201502021 to JC). The funders in our study had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.S. and J.C. conceptualized and designed the study. Z.W. and D.Z. collected the samples. N.X., Z.J., H.L., and Y.J. performed the experiments. N.X., Z.J., H.L., Y.S., and J.C. analyzed the data. Y.S., and J.C. contributed the reagents/materials/analysis tools. N.X. wrote the manuscript. YS and JC revised the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, N., Jiang, Z., Liu, H. et al. Prevalence and genetic characteristics of Blastocystis hominis and Cystoisospora belli in HIV/AIDS patients in Guangxi Zhuang Autonomous Region, China. Sci Rep 11, 15904 (2021). https://doi.org/10.1038/s41598-021-94962-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-94962-3
This article is cited by
-
Unveiling Blastocystis epidemiology in Morocco: subtype diversity among clinical patients with and without gastrointestinal manifestations in the Meknes region
Parasitology Research (2024)
-
Major depletion of insulin sensitivity-associated taxa in the gut microbiome of persons living with HIV controlled by antiretroviral drugs
BMC Medical Genomics (2024)