Abstract
Some cases of chronic rhinosinusitis (CRS) require surgical treatment and postoperative nasal packing, but bleeding and adhesion are common complications after nasal surgery. Biodegradable drug-loaded implants hold great therapeutic options for the treatment of CRS, but little data are available regarding the safety and efficacy of a novel drug-loaded haemostatic sponge (DLHS) in the sinus. The aim of this study was to investigate the safety and efficacy of DLHS in the sinus. We conducted a prospective, randomized, controlled, double-blind clinical trial. In this clinical trial, 49 patients were enrolled and randomly divided into 2 groups: group A (n = 25) had the DLHS containing 1 mg budesonide and 0.67 mg sodium hyaluronate placed into the sinus, and group B (n = 24) had the Nasopore placed after ESS. Endoscopic follow-up was performed for 12 weeks, and the findings were classified using the discharge, inflammation, polyps/oedema (DIP) endoscopic appearance scores. All patients completed questionnaires to evaluate their sinonasal symptoms by using the sinonasal outcome test-22 (SNOT-22) Chinese version and visual analogue scale (VAS). Serum cortisol concentration in group A was measured prior to surgery and at days 1, 3, 7, and 14 after nasal surgery. Comparing group A and group B, at 2 weeks, no significant differences were observed in either objective or subjective parameters. The mean value of VAS for rhinorrhoea and DIP for oedema and the mean value of nasal adhesion were significantly lower in Group A than in Group B at 6 and 12 weeks, but a significant difference did not occur in SNOT-22 and VAS for dysosmia between the two groups at 6 and 12 weeks. The mean serum cortisol concentrations in group A at the follow-up were within normal limits without remarkable fluctuations. This study demonstrates the safety and efficacy of a novel biodegradable DLHS with the possibility of being used in CRS patients, and this sponge may reduce inflammation and minimize adhesions via controlled local drug delivery without measurable systemic exposure.
Similar content being viewed by others
Introduction
Chronic rhinosinusitis (CRS) is a long-term mucosal inflammatory disease. In China, the prevalence rate of CRS is up to 8%, and approximately 20% of patients with CRS require surgical treatment1,2. Endoscopic sinus surgery (ESS) is perhaps the most commonly performed surgery for managing CRS3; however, bleeding and adhesion are common complications after nasal surgery and postoperative adhesion can result in persistent CRS symptoms after ESS4. In the setting of ESS, interest in the development of biomaterials stems from the desire to decrease postoperative surgical complications and improve patient outcomes. Some substantial research and development of implantable spacers can deliver continuous, high-potency anti-inflammatory medications directly to the sinus mucosa after ESS in the hopes of haemostasis, adhesion prevention, and topical medication delivery to prevent disease relapse and reduce the need for systemic therapy5.
Given the inflammatory nature of CRS, corticosteroids have proven to be an effective treatment for CRS, and they have a minimal risk profile and are typically regarded as the mainstay of medical treatment for this condition6,7; therefore, corticosteroids are often recommended as the drugs of choice by the current CRS guidelines8. Meanwhile, sodium hyaluronate (SH) supplementation added to standard corticosteroids seems to play an important role in improving postoperative healing, particularly in allergic CRS9. In the nasal mucosa, SH is involved in the regulation of vasomotor tone and gland secretion and stimulates mucociliary clearance10.
Recent studies have shown that soaking packing materials -Nasopore (Polyganics BV) with mometasone furoate (MF) during surgery improves the endoscopic appearance of the sinus during the healing process of CRS after ESS11. However, the amount of MF released from nasal packing materials is uncontrolled and inconsistent, which may result in erratic outcomes when using this treatment strategy. For these reasons, nasal drug-loading implants that release the drug locally to the affected site for a prolonged period of time and with a prolonged mucosal contact time appear to be an option that may assist in solving some of these problems12. Chitosan is a bioactive polymer with a wide variety of applications due to its functional properties, such as antibacterial activity13, wound dressing, tissue engineering and therapeutic drug delivery14. Therefore, chitosan, SH and budesonide (BUD) were used as the main materials to make a drug-loaded haemostatic sponge (DLHS) in the hope of diminishing bleeding, preventing adhesion, maintaining ostial patency, reducing postoperative inflammation and promoting mucosal healing after ESS. Considering that the DLHS and the Nasopore are both degradable haemostatic sponges, we compared the clinical safety and effectiveness of the DLHS (experiment) with that of the Nasopore (control). The present prospective, double-blind, controlled study was conducted with the aim of assessing the safety and effectiveness of DLHS in patients with CRS.
Materials and methods
Device description
DLHS, shown in Fig. 1, is a sterile, bioabsorbable, chitosan-based implant developed by our team for use as a sinonasal dressing after ESS. Each DLHS measures 4 cm × 2 cm × 1.5 cm, contains 1 mg BUD and 0.67 mg SH and is designed to provide controlled local delivery of corticosteroids over 14 days. Our previous experimental study15 showed that the morphological analysis regarding the sample composition results shows that the DLHS possesses good characteristics and favourable bioabsorbability and biocompatibility.
Clinical trial
Ethical considerations
In this double-blind, randomized, prospective trial, we studied CRS patients with ESS who were admitted to the Department of Otolaryngology, Ningbo Municipal Hospital of TCM between January 2021 and June 2021. This study was approved and recorded by the Medical Ethics Committee of Ningbo Municipal Hospital of TCM, China (no. KY20201114), all experiments were performed in accordance with relevant guidelines and regulations. It has been registered in the Chinese Clinical Trial Registry (No. ChiCTR2000041549) on 28/12/2020. All the participants gave their written informed consent to participate in the study.
Design of the study
In this study, a total of 49 patients diagnosed with CRS with or without nasal polyps were included in this study, including 29 males and 20 females aged 19–65 years. The inclusion criteria were a diagnosis of CRS according to the criteria defined in the European Position Paper on Rhinosinusitis and Nasal Polyps 202016. Subjects with previous sinonasal surgery, sinonasal malignancy, autoimmune disease, cystic fibrosis, pregnancy, diabetes, hypersensitivity to any ingredient used for the nasal douches and women of fertile age not taking contraceptives were excluded. The recruited patients were randomized on a 1:1 basis to be assigned to two intervention groups (group A and group B) and given the treatments. The planned surgical intervention required bilateral ethmoidectomy with middle meatal antrostomy. Concurrent septoplasty and surgical treatment of the other paranasal sinuses was permitted. Group A (n = 25) had the DLHS placed into the sinus cavity, and Group B (n = 24) had the Nasopore placed after ESS. All surgeries were performed by the same operator, and the packing-materials was cleaned by operator 2 weeks after surgery in both groups and patients were treated with nasal irrigation and BUD nasal spray for 10 weeks.
At enrolment, all patients completed questionnaires to evaluate their sinonasal symptoms by using the sinonasal outcome test-22 (SNOT-22) Chinese version and visual analogue scale (VAS)17,18, and they underwent nasal endoscopy. The patients were reassessed with the same tests after 2, 6 and 12 weeks of treatment. The operator, who did not participate in the postoperative outcome evaluation, and the postoperative grader were blinded to each other’s findings. The SNOT-22 is a validated, disease-specific tool for measuring health-related quality of life in patients affected by CRS. It includes a list of 22 sinonasal symptoms, and within each test, the patient must indicate the severity perceived in the last 2 weeks with a score ranging from 0 (symptoms not present) to 5 (maximum severity of the symptom). It was used to score the impact of CRS on the patients' quality of life and to measure the outcomes of nasal therapy in the two groups before and after treatment. The patients were also asked to evaluate the degree of their nasal blockage, dysosmia and rhinorrhoea by means of VAS: the patient had to mark a score ranging from 0 (symptoms not present) to 10 (maximum severity imaginable). Nasal endoscopy was performed using a rigid 0° or 30° endoscope, and the findings were classified using the discharge, inflammation, polyps/oedema (DIP) endoscopic appearance scores19. Each category was scored from 0 to 10. For the discharge category, a score of 0 indicates absent discharge, 5 indicates thick mucus, and 10 indicates purulent discharge. For the inflammation category, 0 indicates no inflammation, 5 indicates moderate inflammation, and 10 indicates severe inflammation. For the polyp/oedema category, a score of 0 indicates normal mucosa, 5 indicates marked oedema/no polyps, and 10 indicates polyps filling the nasal cavity.
These subjects underwent a series of blood samples to assess their plasma cortisol concentrations over time. A morning blood sample was taken from the patients at baseline prior to surgery and at days 1, 3, 7, and 14. Within 10 min of collection, the samples were centrifuged, the serum was placed in Vacutainers, and the samples were immediately frozen at – 80 ℃ after collection and thawed immediately before use for a total of 1–2 freeze–thaw cycles. Serum cortisol concentrations were measured with sandwich ELISA kit and Labsystems Multiskan MS (Finland).
Statistical analysis
All data are presented as the mean ± standard deviation. Statistical analyses were performed using Student’s t test. *P < 0.05 was considered statistically significant. Statistical analyses were performed using the SPSS® version 22.0 statistical software package.
Ethics approval and consent to participate
This study was approved and recorded by the Medical Ethics Committee of Ningbo Municipal Hospital of TCM, China (no. KY20201114).
Consent for publication
All patients gave written informed consent to participate in the study extension.
Results
A total of 49 patients were enrolled in the study, and all the patients completed all the study visits. As shown in Table 1, there were no significant differences between the two study arms for all preoperative objective and subjective evaluation scores. Complete bilateral ethmoidectomy was performed in all patients, and the DLHS and Nasopore sponges were successfully deployed in all sinuses. Subjective and objective scores were observed during the twelve weeks of follow-up in both treatment arms. By 2 weeks, the DLHS material had basically degraded and could be cleaned easily with an aspirator, and no additional surgeries were required to remove them.
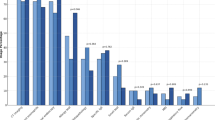
Table 2 provides the comparison of the evaluation scores between the groups at 2, 6, and 12 weeks postsurgery. The outcome measured in the two groups is presented as the mean difference in score in the table. Eventually, considering all of the enrolled patients together, no differences were observed between Group A and Group B for the objective parameters and the following subjective parameters for 2 weeks. In contrast, the mean value of VAS for rhinorrhoea and DIP for discharge, polyps/oedema, and the mean value of nasal adhesion were significantly lower in Group A than in Group B at 6 weeks. Polypoid mucosal changes did not occur in all sinuses in group A and group B at 12 weeks, but the results for DIP for oedema and the mean value of nasal adhesion changed significantly between Group A and Group B. The significant difference did not occur in the DIP for discharge but occurred in VAS for rhinorrhea between the two groups at 12 weeks.
The evaluation scores obtained at different times postsurgery were compared between Group A and Group B, and the comparison is shown in Figs. 2 and 3. In Group A, DIP (Discharge, Inflammation, and Polys/Oedema) and SNOT-22 scores at 6 weeks were significantly different than those at 2 weeks, but in Group B, the difference was not significant. In Group A and Group B, the score at discharge at 12 weeks was significantly different than that at 6 weeks. Unfortunately, no significant improvement in olfactory function was observed in either group during the 12-week treatment period.
Moreover, the mean serum cortisol concentrations at baseline and at the follow-up time points were within normal limits without remarkable fluctuations, and there was no significant difference between the two groups, as shown in Fig. 4, which indicated no evidence of adrenal suppression.
Discussion
The DLHS should be primarily used to control haemorrhage but should also help to prevent adhesion formation, promote drainage of the sinus mucosa and wound healing and have superior clinical treatment effects. The ideal drug-loaded biomaterial should be bioabsorbable, biocompatible, and efficacious in controlled drug release20. CS was chosen as one of the main components of the material because of its good biocompatibility, biodegradation, antibacterial activity, and potential haemostatic ability21. Corticosteroids remain the standard in the treatment of nasal polyps, as they reduce the eosinophilic infiltrates and type 2 inflammation that are central to CRS22.
Biodegradable implants are made up of biodegradable polymeric materials that degrade in vivo over a short period of time. In the present trial, the DLHS material had basically degraded at 2 weeks, and no bleeding occurred in any patient in the two groups during the treatment period. The data analysis shows that there was significant improvement in early postoperative healing of the nasal cavities that received both types of nasal packing after ESS. However, a statistically significant difference in adhesion formation was noted, with the sinuses receiving DLHS having a low adhesion rate of 4% compared to 25% for group B (p < 0.001). The results of the DIP endoscopic appearance scores for Polys/Oedema and VAS for rhinorrhoea changed significantly between Group A and Group B at 12 weeks; however, the effect of the group on the difference in SNOT-22 scores between the two groups was not significant at 12 weeks and may take a longer time to observe. These data suggest that there was a significant improvement in the postoperative healing in nasal cavities receiving DLHS nasal packing following ESS up to 12 weeks postoperatively. It is consequently possible to speculate that the application of corticosteroids and SH release through nasal DLHS material degradation improved the recovery of the nasal mucosa. Therefore, these findings might mean that Group A had a better treatment effect and may have lower rates of postoperative recurrence because of a lower level of mucosal oedema.
In this regard, drug loading implants are surgically inserted into the DLHS and help heal the affected tissue by releasing loaded drugs locally and continuously in a controlled manner for the desired period of time, which can not only be utilized for haemostasis and adhesion prevention but can also bypass medication noncompliance or systemic side effects. Reducing inflammation and polyp formation has the potential to decrease the need for additional steroid intervention in the postoperative packing period23. Systemic safety was assessed in the Group A with bilaterally placed DLHS. Serum cortisol concentration was measured prior to surgery and at days 1, 3, 7, and 14. The results support the prediction that indwelling DLHS would not have effects in suppressing the adrenal–pituitary axis due to the highly localized delivery over a long period of 2 weeks.
This study has several limitations. Both groups of patients had poor postoperative outcomes of olfactory dysfunction at the 12-week follow-up examination, but whether DLHS is beneficial for patients with olfactory disorders requires long-term observation. Meanwhile, the follow-up time of this study is short, and the evaluation of DLHS on the long-term polyp recurrence rate and treatment outcomes need further observation.
Conclusion
The results of the present study show that in patients affected by CRS, treatment with DLHS presents good effectiveness and safety when compared with an analogous therapy utilizing the Nasopore. Sinonasal symptoms were evaluated by using the SNOT-22 and VAS, and the effectiveness and safety of reducing inflammation, adhesions and mucosal oedema changes was judged 2–12 weeks after ESS without negligible potential for systemic corticosteroid-related complications. These results indicate that the DLHS possesses a high potential for achieving better anti-inflammatory properties with reliable biosafety, biodegradability and biocompatibility.
Data availability
All data and materials are available on request from the corresponding author, M.X. upon reasonable request.
References
McCormick, J. P. et al. Phenotypes in chronic rhinosinusitis. Curr. Allergy Asthma Rep. 8(5), 1505–1511. https://doi.org/10.1016/j.jaip.2019.12.021 (2020).
Fujieda, S. et al. Eosinophilic chronic rhinosinusitis. Allergol. Int. 68(4), 403–412. https://doi.org/10.1016/j.alit.2019.07.002 (2019).
Wang, T. C. et al. Absorbable and nonabsorbable packing after functional endoscopic sinus surgery: Systematic review and meta-analysis of outcomes. Eur. Arch. Otorhinolaryngol. 272(8), 1825–1831. https://doi.org/10.1007/s00405-014-3107-2 (2015).
Miller, R. S. et al. The clinical effects of hyaluronic acid ester nasal dressing (Merogel) on intranasal wound healing after functional endoscopic sinus surgery. Otolaryngol. Head Neck Surg. 128(6), 862–869. https://doi.org/10.1016/S0194-59980300460-1 (2003).
Massey, C. J. et al. Biomaterials in rhinology. Otolaryngol. Head Neck Surg. 154(4), 606–617. https://doi.org/10.1177/0194599815627782 (2016).
Fokkens, W. J. EPOS2020: A major step forward. Rhinology 58(1), 1. https://doi.org/10.4193/Rhin20.401 (2020).
Small, C. B. et al. Onset of symptomatic effect of mometasone furoate nasal spray in the treatment of nasal polyposis. J. Allergy Clin. Immunol. 121(4), 928–932. https://doi.org/10.1016/j.jaci.2007.11.018 (2008).
Wang, C. et al. Effect of budesonide transnasal nebulization in patients with eosinophilic chronic rhinosinusitis with nasal polyps. J. Allergy Clin. Immunol. 135(4), 922-929.e6. https://doi.org/10.1016/j.jaci.2014.10.018 (2015).
Cantone, E. & Iengo, M. Effect of sodium hyaluronate added to topical corticosteroids in chronic rhinosinusitis with nasal polyposis. Am. J. Rhinol. Allergy 30(5), 340–343. https://doi.org/10.2500/ajra.2016.30.4344 (2016).
Savietto, E. et al. Effectiveness of micronized nasal irrigations with hyaluronic acid/isotonic saline solution in non-polipoid chronic rhinosinusitis: A prospective, randomized, double-blind, controlled study. Am. J. Otolaryngol. 41(4), 102502. https://doi.org/10.1016/j.amjoto.2020.102502 (2020).
Zhao, K. Q. et al. Effects of mometasone furoate-impregnated biodegradable nasal dressing on endoscopic appearance in healing process following endoscopic sinus surgery: A randomized, double-blind, placebo-controlled study. Int Forum Allergy Rhinol. 8(11), 1233–1241. https://doi.org/10.1002/alr.22213 (2018).
Parikh, A. et al. Drug-eluting nasal implants: Formulation, characterization, clinical applications and challenges. Pharmaceutics 6(2), 249–267. https://doi.org/10.3390/pharmaceutics6020249 (2014).
Muxika, A. et al. Chitosan as a bioactive polymer: Processing, properties and applications. Int. J. Biol. Macromol. 105(Pt 2), 1358–1368. https://doi.org/10.1016/j.ijbiomac.2017.07.087 (2017).
Zhang, Y. et al. Biomacromolecules as carriers in drug delivery and tissue engineering. Acta Pharmaceut. Sin. B 8(1), 34–50. https://doi.org/10.1016/j.apsb.2017.11.005 (2018).
Wang, L. S. et al. Properties and effects of a drug-loaded haemostatic sponge. JOM 75(12), 5619–5627. https://doi.org/10.1007/s11837-023-05948-7 (2023).
Fokkens, W. J. et al. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58(29), 1–464. https://doi.org/10.4193/Rhin20.600 (2020).
Rimmer, J. et al. European position paper on diagnostic tools in rhinology. Rhinology 57(28), 1–41. https://doi.org/10.4193/Rhin19.410 (2019).
Zhao, L. et al. Severity of rhinosinusitis: Comparison between visual analog scale given by patients and otorhinolaryngologists. Am. J. Rhinol. Allergy 34(6), 734–741. https://doi.org/10.1177/1945892420923934 (2020).
Psaltis, A. J. et al. Modification of the Lund-Kennedy endoscopic scoring system improves its reliability and correlation with patient-reported outcome measures. Laryngoscope 124(10), 2216–2223. https://doi.org/10.1002/lary.24654 (2014).
Patel, V. S. et al. Biocompatibility and pharmacokinetics of fluticasone-eluting sinus implant in a rabbit model. Am. J. Rhinol. Allergy 31(6), 382–388. https://doi.org/10.2500/ajra.2017.31.4481 (2017).
Song, F. et al. Chitosan-based multifunctional flexible hemostatic bio-hydrogel. Acta Biomater. 136, 170–183. https://doi.org/10.1016/j.actbio.2021.09.056 (2021).
Shen, J. et al. Mometasone furoate sinus implant—a new targeted approach to treating recurrent nasal polyp disease. Expert Rev. Clin. Pharmacol. 11(12), 1163–1170. https://doi.org/10.1080/17512433.2018.1549485 (2018).
Murr, A. H. et al. Safety and efficacy of a novel bioabsorbable, steroid-eluting sinus stent. Int. Forum Allergy Rhinol. 1(1), 23–32. https://doi.org/10.1002/alr.20020 (2011).
Acknowledgements
The authors acknowledge Professor Wang Rong's team of Institute of Biomedical Engineering, Ningbo Institute of Materials Technology and Engineering, Chinese Academy of Sciences for their technical support.
Funding
This work was supported by the research project of Zhejiang Chinese Medicine University (Grant n. 2021FSYYZY09), and Ningbo Municipal Public Welfare Fund Project, China, (grant n. 2023S020).
Author information
Authors and Affiliations
Contributions
"X.J., J.M. and M.X. performed all the experiments, analyzed the data, and wrote the draft of the manuscript. M.X. designed the research plan, conceived the project, and obtained financial support. J.W., W.W. and D.W. supported in the clinical taskst. All authors reviewed the manuscript".
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, X., Meng, J., Wang, J. et al. Safety and effectiveness of a drug-loaded haemostatic sponge in chronic rhinosinusitis: a randomized, controlled, double-blind study. Sci Rep 14, 21968 (2024). https://doi.org/10.1038/s41598-024-64669-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64669-2