Abstract
Hyperlipidemia significantly contributes to the risk of developing cardiovascular diseases. However, about half of the patients do not adhere to their antihyperlipidemic medications, leading to healthcare costs and premature mortality. This study's objective was to determine the prevalence and associated factors of non-adherence to antihyperlipidemic medications. The study covered hypertensive patients (21,451) aged 21–75 years, presenting to the primary and secondary healthcare facilities across Pakistan (covering 21 divisions) from January 2022 to April 2023. The outcome intended was non-adherence to antihyperlipidemic medication, which was assessed by SEAMS and pill-counting methods (non-adherence < 80%). The study found overall non-adherence to antihyperlipidemic medication of 60.6% across Pakistan, with the highest non-adherence rates found in Azad Jammu and Kashmir (71.9%) and the lowest in Islamabad (47.7%). Multivariable logistic regression analysis revealed that female, no health card (Sehat Sahulat Program government insurance), < 5 years of illness, < 5 daily medications, and dose frequency of twice daily revealed a positively significant association with non-adherence. While monthly income 51,000–100,000, graduation level of education, Muhajir, and hyperlipidemia with one comorbid condition had a significant negative association with the non-adherence. Antihyperlipidemic non-adherence is a multifaceted, multifactorial, profound problem requiring a multipronged approach.
Similar content being viewed by others
Introduction
The most prevalent kind of dyslipidemia is hyperlipidemia, a crucial risk factor for cardiovascular diseases (CVDs) and the leading cause of morbidity and mortality worldwide1. Hyperlipidemia accounts for one-third of all ischemic heart disorders worldwide, and the mortality rate is 2.6 million/year2. As a result, controlling hyperlipidemia is paramount for lowering cardiovascular disease risks. Lipid-lowering drugs like statins are frequently prescribed to reduce the risk of micro- and macro-cardiovascular problems linked to hyperlipidemia3,4,5.
Statins are the unambiguous first choice for treating hyperlipidemia6 and have been used widely as a medication to treat hyperlipidemia, specifically lowering low-density lipoprotein (LDL)7,8. The pharmacoeconomic studies have demonstrated that statins are the most cost-effective therapy for treating CVDs9,10 and reducing CVDs-related mortality11,12. Statins are a medication class that lowers cholesterol levels by blocking the HMG-CoA reductase enzyme. Statins are widely advised for the primary and secondary prevention of cardiovascular diseases13. Statins have been incorporated into WHO clinical practice guidelines for CVD prevention and control14 and have become the first-line therapy for reducing the risk of CVD mortality and morbidity13.
Medication adherence is the act or extent of conforming to a provider's recommendation/prescription based on timing, dosage, and frequency of medication use1. “A ratio of the number of drug doses taken to the number of doses prescribed over a given time period”15 is another definition. Medication non-adherence can be divided into two categories: primary and secondary non-adherence. Primary non-adherence is when the medication is not adhered to the first time it was prescribed. Prescription refills among patients who have previously finished their initial prescriptions are measured by secondary non-adherence16.
Good adherence is based on various factors such as the patient's socioeconomic and demographic factors, physician's and health system factors (cost and accessibility), and managing the drug side effects17,18. Patient behavior, such as ignoring medical advice, skipping doses, missing appointments, etc., may diverge from the guidelines established during therapy. Whether on purpose or accidentally, this could result in non-adherence. Therefore, non-adherence is the patient's refusal or resistance to adequately following any medical regimen or therapy19,20. Poor medication adherence refers to the amount of prescribed medication a patient takes and the time between starting and stopping a drug16.
Statin adherence in clinical practice remained below ideal even though the favorable effects of statin therapy have been documented over the previous 30 years21,22. Research shows that about half of CVD patients do not adhere to their healthcare provider's prescriptions, leading to reduced treatment efficacy23. It was found that 40–75% of patients stopped taking their statin therapy within the first year of starting it24,25. The effectiveness of statin medication was constrained by poor adherence26. Medication is not desirably effective for non-adherent patients27. It has been established that early termination of therapy shortly after treatment initiation contributes to non-adherence25. According to several studies, non-adherence to statin therapy was linked to an increased risk of cardiovascular and cerebrovascular morbidity, events, and mortality, considerably raising medical expenses21,22,28,29.
Positive health outcomes are primarily dependent on medication compliance. However, statin users' adherence patterns in Pakistan have not been thoroughly examined. Little information is available on the potential link between statin non-adherence among adult Pakistani patients. To attain therapeutic goals, it is necessary to understand the obstacles to drug adherence30.
Evidence is scarce regarding the non-adherence to antihyperlipidemic medication in the local context of Pakistan. With a nationally representative sample, the current study tried to fill this knowledge gap. The study aimed to find out the prevalence of non-adherence to antihyperlipidemic medication and the potential factors associated with this non-adherence in Pakistan.
Methods
Study design, settings, and participants
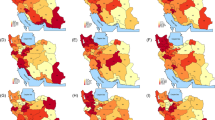
A cross-sectional study was carried out in Pakistan from January 2022 to April 2023. The study was a population-based national survey that included hyperlipidemic patients across Pakistan. This was a multi-hospital (multiple healthcare facilities were involved n = 205) study conducted in the public sector primary (Basic Health Unit (BHU)/Rural Healthcare Center (RHC)) and secondary (Tehsil Head Quarter (THQ)/District Head Quarter (DHQ) level health care facilities of all the provinces of Pakistan, namely; Punjab, Sindh, Baluchistan, and Khyber Pakhtunkhwa (KP) along with Pakistan's autonomous region Azad Jammu and Kashmir (AJ&K) and the federal capital Islamabad. All these regions will be called as provinces hereafter. Further sub-divisions of these provinces are termed divisions in Pakistan (further smaller sub-divisions are called districts, tehsils, and union councils). Our study included healthcare facilities at the divisional level in Pakistan. Included divisions were Lahore, Multan, Rawalpindi, Islamabad, Sahiwal, Sargodha, Gujranwala, Faisalabad, Dera Ghazi Khan (Punjab province), Karachi, Hyderabad, Larkana, Sukkar, and Mir pur Khas (Sindh province), Quetta (Baluchistan province), Peshawar, Bannu, Kohat and Dera Ismail Khan (KP province), AJ&K province and Islamabad (Fig. 1)31. Sahiwal is not shown separately; it is merged with Multan on the map; otherwise, it is a separate division. The Geographic Information System (GIS) basic map with Sahiwal as a separate division was inaccessible. Some divisions of Baluchistan and Federally Administered Tribal Areas (FATA) were not included due to the law and order/security situation there. See Fig. 1 below for the overall representations of the hospitals from the country. As evident, the sampled hospitals are from the entire country, which is a good representation of Pakistan.
Sampled health facilities from the divisions across Pakistan. (Figure constructed through Geoda subversion 1.16.0 (https://geodacenter.github.io/download.html)32.
Sampling procedure
The sampling procedure for the current study covered the entire country, where accessibility was not an issue. For this purpose, a multi-stage sampling technique was applied. In the first stage, all those accessible divisions were selected for the study. Within those divisions, the list of the hospitals was retrieved (see supplementary file for hospital links). The hospitals in each of the divisions were then stratified as primary-level healthcare facilities and secondary-level healthcare facilities. Random selection was made from these in each of the tiered healthcare facilities. During the last stage of sampling, consecutive patients in the daily outpatient department of the hospital fulfilling the inclusion criteria were selected and referred by the medical officer to the study team for a detailed interview.
Inclusion and exclusion criteria
Eligible participants were those already diagnosed with hyperlipidemia, taking lipid-lowering treatment/statins for at least six months for the primary or secondary prevention of CVD, in the age group 21–75 years, who can communicate in the Urdu language in any primary or secondary care setting. Participants aged less than 21 years or more than 75 years, self-reported pregnant females, participants with any mental disorder such as psychosis or dementia, history of cancer, and those who do not communicate in Urdu were excluded from the study.
Study outcome
The outcome of the current study was non-adherence to antihyperlipidemic medication in Pakistan. Non-adherence was measured using the Self-Efficacy for Appropriate Medication Scale (SEAMS) and pill count as self-reported measures. Self-reported pill count was the primary outcome, and SEAMS supported the outcome variable in the current study. Measuring medicine adherence involved two approaches: SEAMS score and pill counts, which enhanced the credibility of the assessment technique and produced more accurate results. A body of prior research on the topic has supported these methods33,34.
SEAMS is the most popular and valid tool used in health sciences to measure adherence/non-adherence. It is a proven cost and time-effective measure. The SEAMS is a 13-item medication adherence measure scale. The SEAMS uses a three-point response scale, with 1 representing a lack of confidence, 2 a moderate level of confidence, and 3 a high level of confidence. The Likert scale was used to evaluate the questionnaire. As a result, there were 13 questions and 3 viable options for each. The minimum score was 13, while the maximum was 39. Higher scores were linked to greater medication adherence and vice versa. In previous literature, no cut-off points were used for SEAMS scores33,35,36. The SEAMS tool was translated using the traditional “forward–backward” method from English into Urdu (SEAMS-U) in Pakistan. The translated version was validated using a practical sample of 1011 hyperlipidemic patients receiving treatment at a tertiary care hospital in Lahore, Pakistan. The internal consistency of the translated SEAMS-U was good (Cronbach’s alpha = 0.897). Cronbach’s alpha (Part 1) was 0.838, and (Part 2) was 0.789 by split-half reliability. The test–retest reliability was (Spearman’s P = 0.686, P < 0.001), and the intraclass correlation coefficient (ICC) score was 0.814. All ethical concerns pertaining to validity, dependability, and forward–backward translation were suitably and meticulously handled. The SEAMS Urdu–version is in the publication process.
The primary outcome of non-adherence to antihyperlipidemic medication in the current study was based on self-reported pill counting. In this method, participants were asked how many pills they had been prescribed for a specific period of time and how many pills they had actually taken. Based on this information, the non-adherence rates were computed using the pills consumed over a certain period divided by the pills prescribed for that period27. Based on the calculations, those with an adherence percentage of less than 80% were declared non-adherent, while those equal to or above 80% were classified as adherent. This cut-off is reported in the literature as well27,33,37, and this approach has a better accuracy38.
Additionally, sociodemographic variables were added to obtain information regarding age (in years), gender, ethnicity, education, income, and occupation; health-related factors were concomitant disease, duration of illness, number of daily medications, comorbidities and dose (mg), and per-day frequency of medication. Number of prescribed medicines, time of intake as either morning, afternoon, or evening, any side-effect, number of pills prescribed for the last fifteen days, number of pills taken, and any missed dose in the last fifteen days.
Data collection and statistical analysis
Data collection was preceded by administrative approvals from the concerned health facility in-charge. Data was collected after informed consent from the patients. Patients were consecutively approached from the outpatient department of the participating hospitals. For this purpose, the concerned doctors in the hospitals referred the patients to the study team after evaluating the inclusion and exclusion criteria. The interview was then conducted with the concerned patients in a separate room.
Data was entered in Microsoft Excel and later analyzed in Statistical Package for Social Sciences (SPSS) version 26 and R studio. Study variables were first evaluated using descriptive statistics. Continuous data is reported as mean (± standard deviation) and categorical variables as numbers (percentages). The generalized linear model (GLM) using multivariable binary regression analysis was employed to evaluate the effect of various sociodemographic and health-related factors on non-adherence to antihyperlipidemic medication. Multivariable binary regression analysis was applied to observe the predictors of non-adherence. The enter method was employed, and statistically significant variables (p-value < 0.05) from the Pearson product-moment correlation coefficient, t-test, and one-way analysis of variance (ANOVA) were retained in the logistic regression model. The significance level was kept at 5%.
Training/calibration and quality control
Medical Officers (MOs) from respective healthcare settings were recruited as master trainers on data collection. MO is a professional doctor with an MBBS degree and is responsible for delivering curative/preventive services in healthcare settings and often renders administrative duties at these facilities. MOs were trained through a web-based session (Zoom application), which in turn trained the research assistants on-site. The research assistants (RAs) were medical students (4th year MBBS), paid monthly throughout this project. Two RAs were assigned for every 20 facilities, and MOs were responsible for training/calibration and supervision of the data collection process. A joint refresher training (via Zoom application) of all the research assistants as well as MOs was also done once all MOs completed all the formal training sessions of their RAs. A qualified epidemiologist performed all these training sessions using a standard training module duly validated before these training sessions. The training module included two-day on-site training of all recruited staff on medication adherence and how to respond to the common questions related to adherence/non-adherence. The training module also addressed the counseling and support to the participants in filling out the adherence/non-adherence to medication questionnaires.
Training protocols were efficiently maintained throughout, ensuring that all surveyors had a standardized understanding of survey objectives, procedures, and ethical considerations and were proficient in data collection methods to minimize variability. During the data collection, the supervisors (MOs) ensured that the same standardized tools were being used for interviews and that accurate and consistent responses were being recorded with no incomplete data. This was done by immediate data checking and validation by the MOs by conducting spot checks and random re-interviews. Real-time feedback and troubleshooting were done wherever required.
Ethics approval
Rehmatul-Lil-Almeen Institute of Cardiology’s Institutional Ethical Review Board (Reference Number: RAIC-PESSI-963) and Employers Social Security Tertiary Hospital Lahore (PESSI-1026) approved the study protocol. However, we obtained administrative approval from the concerned health facility before data collection. Written informed consent was obtained from all participants. Furthermore, the study and all applied methods followed the relevant guidelines and regulations.
Results
A total of 51,902 patients were approached for the study. After excluding patients (17,210) and those refusing participation (13,241) the remaining patients (21,451) were retained and interviewed regarding their medication adherence (Fig. 2).
Respondents’ demographic profile
The sociodemographic details of the sample are presented in Table 1. The table below shows that around half of the participants were 50–75 years of age (51.1%), had 51,000–100,000 PKR monthly income (44.7%), and had an illness duration of > 5 years (53.2%). Moreover, more than two-thirds of males (69.8%) had graduate-level education (37.7%) and Punjabi ethnic identity (34.3%). Health-related factors included one comorbid condition (88.7%), half of the participants were with obesity as a type of comorbidity, less than five medications (43.6%), and having a once-daily dose (85.3%). The rest of the demographic information is provided in Table 1.
Respondents’ spatial and health facility level distribution
Pakistan has four provinces, Punjab, Sindh, Baluchistan, and Khyber Pakhtunkhwa, and one Capital territory, “Islamabad.” Pakistan also includes one autonomous region: Azad Jammu & Kashmir, which was included in this study. Most of the participants were from the province of Punjab 9471 (44.2%), while the lowest number was from Islamabad 703 (3.3%) (Table 2). Division-level data is fairly similarly distributed across Pakistan, with a similar representation from the primary and secondary healthcare facilities.
The SEAMS responses on non-adherence to medications
The SEAMS questionnaire and the response percentages are depicted in Table 3. As can be seen, the non-adherence to antihyperlipidemic medication was measured through the 13 questions, and their different responses are shown. The frequency of non-adherent respondents to antihyperlipidemic medication using SEAMS score was mean (SD) 26.79 (7.44), whereas the frequency of non-adherent respondents to antihyperlipidemic medication using pill-counting was 12,949 (60.3%).
Non-adherence to antihyperlipidemic medication in the provinces and divisions of Pakistan
Our study depicted that non-adherence was prevalent in Azad Jammu & Kashmir and Khyber Pakhtunkhwa provinces of Pakistan (72% and 69%, respectively), while the least prevalent were Islamabad and Punjab (47% and 55%, respectively). Sindh and Baluchistan provinces had intermediate non-adherence to antihyperlipidemic medication compared to the rest. Division-wise results of non-adherence to antihyperlipidemic medication revealed that the most prevalent divisions were Mirpur Khas (80.2%), Bannu (78.3%), Dera Ghazi Khan (77.5%) and Kohat (76.1%), while Lahore (38.9%) and Karachi (42.3%) were amongst the least non-adherent ones. (Fig. 3). Additional details of the non-adherence in the provinces and the divisions can be found in the supplementary data.
Factors affecting non-adherence to antihyperlipidemic medications
The generalized linear model (GLM) logit model utilizing multivariable logistic regression revealed eight significant variables associated with the probability of having non-adherence to antihyperlipidemic medication. The female gender (AOR = 1.275, 95% CI [0.881–1.845], P < 0.001), no health card (Sehat Sahulat Program government insurance) coverage (AOR = 2.802, 95% CI [1.948–4.032], P < 0.001), less than five-year of illness (AOR = 1.216, 95% CI [1.132–1.306], P < 0.001), less than 5 daily medications (AOR = 1.699, 95% CI [1.535–1.882], P < 0.001) and dose frequency of twice daily (AOR = 4.729, 95% CI [2.998–7.458], P < 0.001) were positively associated with non-adherence. While the 51,000–100,000 monthly income (AOR = 0.623, 95% CI [0.577–0. 0.672], P < 0.001), graduation level of education (AOR = 0.875, 95% CI [0.809–0.946], P < 0.001), Muhajir (AOR = 0.415, 95% CI [0.250–0.689], P < 0.001) and hyperlipidemia with one comorbid condition (AOR = 0.108, 95% CI [0.094–0.124], P < 0.001) were negatively associated with the non-adherence with very strong evidence against the model hypothesis at the sample size (Table 4).
Discussion
The study investigated the prevalence of non-adherence to antihyperlipidemic medication across the country, covering the four provinces and most of the divisions (around two-thirds). Overall, non-adherence to antihyperlipidemic medication in Pakistan was 60.6%. The non-adherence rates at the provincial level were highest in AJK (71.9%) and Khyber Pakhtunkhwa (68.8%) and the lowest in Islamabad (47.7%). Punjab, Sindh, and Baluchistan had non-adherence rates of 55.5%, 63.0%, and 60.5% respectively. Additionally, the study found that the prevalence of non-adherence varied within each province across the divisions.
Our study discovered various statistically significant factors linked with non-adherence to antihyperlipidemic medication. Out of these, factors positively associated with non-adherence were the female gender, having less than five years of illness, having fewer than five daily medications, no health card (Sehat Sahulat Program) coverage, and having a dose frequency of twice daily. Meanwhile, the 51,000–100,000 PKR monthly income, graduation level of education, Muhajir, and hyperlipidemia with one comorbid condition were found to be negatively associated with non-adherence to antihyperlipidemic medication.
Existing literature representing isolated parts of the country supports the evidence generated through our findings; however, our analysis signifies national-level data, which is logically not analogous to the findings of those small-scale studies. Depending on their assessment methods and patient demographics, previous research estimated that the prevalence of antihyperlipidemic medication non-adherence ranged from 20 to 80%29. However, some recent literature stated that non-adherence to cardiovascular treatment has been stretched between 40 and 80%39,40,41. Another study mentioned that the prevalence of good adherence to these medications has improved to 54%42. One of the systematic reviews (done from 2012 to 2016) on older people (> 65 years) showed adherence rates ranged between 28 and 60% for the antihyperlipidemic medication users of 2–10 years, respectively; hence, adherence rates were observed to be declining with years of usage43. A relatively recent systematic review described adherence to antihyperlipidemic medications as prevalent between 17.8 and 79.2%. 44 The most recent evidence from the American region states that the pooled prevalence of antihyperlipidemic medication adherence has been around 78.9%, while non-adherence is around 21%45. As adherence is associated with many sociodemographic characteristics, therefore pooled prevalence comparisons will have vast heterogeneity.
Adherence and/or non-adherence measurement
Although it is challenging to measure adherence and/or non-adherence, both direct and indirect methods for measuring adherence (or non-adherence in some cases) have benefits and drawbacks27. Directly monitored therapies are impractical for everyday use and can be compromised by patients who “cheek” or conceal their tablet intake. The same is true for objective measurements of the drug or its metabolites, which are often expensive, have different degrees of value, and do not take into consideration “white-coat adherence” (better adherence) just before and after a medical interaction. On the other hand, indirect methods often include surveys, self-reporting, and pill counts and are simple but prone to deceit46.
Rates of prescription refills also act as a substitute for adherence as such data are readily available from pharmacies. Still, it is not deemed the same as the ingestion of medication. Most statin adherence trials used an arbitrary cut-off of 80% while defining adherence. However, clinicians should note that those with greater than 80% adherence may derive even further benefits from reduced LDL-C levels 46. The current study used the SEAMS questionnaire and pill counting to assess statin non-adherence. The prevalence of medication non-adherence measured by both approaches did not differ significantly, providing triangulation for our findings to be dependable.
The current study found that non-adherent respondents to antihyperlipidemic medication using SEAMS score was mean (SD) 26.79 (7.44). Prior research has employed SEAMS to assess drug adherence in long-term conditions such as cardiovascular diseases (CVDs), hypertension, and other chronic illnesses, and different findings of SEAMS scores were revealed33,36,47. The median (IQR) SEAMS score was reported in earlier research to be 19.5 (5) and 21 (6), respectively33.
Potential predictors affecting non-adherence to antihyperlipidemic medication
Medication non-adherence is a complicated, multifaceted healthcare issue. Even the most effective treatment will fail if the patient refuses to take it27. The ability of patients to adhere to treatment regimen suggestions is referred to as adherence. On the other side, inadequate implementation of the dosing schedule, non-initiation of the prescribed therapy, or early termination of the treatment may result in non-adherence to medication48,49,50. During various phases of their treatment, patients may not adhere owing to various factors, including gender, education level, income status, duration of illness, presence, and type of comorbidities, number of prescribed medicines, dose frequency, and relation with the physician. It is well-established that non-adherence to antihyperlipidemic medication is linked to increased cardiovascular mortality21,22,28,29. Improvement in adherence to antihyperlipidemic medication results in cost savings in overall healthcare (an increase in drug expenses but a considerable decrease in hospitalization and outpatient care expenditures)51; hence, adherence is a vital element of the drug and cost efficacy. Our study identifies several factors that affect medication non-adherence in hyperlipidemia patients. Statistically significant variables negatively associated with non-adherence to antihyperlipidemic medication were female gender, graduation level of education, good income status, health card (Sehat Sahulat Program) coverage, more than five years of illness, hyperlipidemia with one comorbid condition, up to five prescribed medicines, and dose frequency of once daily. Various factors of treatment adherence in patients receiving antihyperlipidemic medication were elaborated in prior studies. Some of them align with our findings, while others differ.
In the current study, the female gender was found to be less likely to default to antihyperlipidemic medication than males. Previous literature supports our findings52,53. Although age was not a significant contributor to non-adherence to antihyperlipidemic medication in this research, previous studies established that non-adherence to antihyperlipidemic medications declines with an increase in age54,55, and another study quantified this decline, stating that non-adherence probability falls by roughly 5–11% for every decade of age56. In the current study, education had a mixed association with non-adherence; compared to postgraduate education, primary and secondary education had more odds of being non-adherent, while the graduates were less likely to be non-adherent to antihyperlipidemic medications. In the current study, Muhajir’s ethnicity was found to be less likely non-adherent than that of other groups. This could be due to the fact that the majority of these Urdu-speaking participants (Muhajir) are well-educated, which could improve their adherence. Although further studies on different races were in line with our study, some ethnicities are linked with non-adherence, such as African American patients55,57 and the Hispanic population have been linked to the worst drug non-adherence57,58.
In our study, income status remained statistically significant for medication adherence. The participants with a monthly income of 51,000–100,000 rupees demonstrated fewer odds of being non-adherent to antihyperlipidemic medication, while lesser income levels were positively associated with the outcome. A study by Osborn et al. investigated the connections between financial stress and medication compliance and found higher income was significantly correlated with less non-adherence in adjusted models (P < 0.001). Still, this association disappeared when financial stress was observed. Financial stress positively impacts the association of income with non-adherence (r = − 0.17, P < 0.001) and worse self-rated health (r = − 0.23, P < 0.001) 59. Income has been more strongly connected with adherence among men than women44, and it was also found that patients having health insurance exhibited less non-adherence57.
In the current study, the majority of the sociodemographics were linked to non-adherence to antihyperlipidemic medication. Sociodemographic variables like education levels might be too broad to accurately predict a person's medication use. This is consistent with a prior study that found that treatment comprehension matters more than educational attainment60.
Previous studies have demonstrated that non-adherence to antihyperlipidemic medication is also linked to several medication-related factors. In the current study, the participants with less than five years of illness showed higher odds of non-adherence than patients with a history of more than five years, depicting that the recent adoption of antihyperlipidemic medications contributed to non-adherence. This might be due to the appearance of adverse effects of the medicines in users of these chronic disease patients, making them more likely to purposefully break their medication regimen. However, the literature also suggests that non-adherence was more prevalent in patients with newly prescribed lipid-lowering drugs52,61. Additionally, non-adherence to prescribed treatments is more common among patients who experience side effects or have concerns about potential side effects62. These individuals exhibit a 2.89 times higher odds ratio of non-adherence compared to those without side effects63. This highlights the substantial influence of drug-related side effects on patients’ adherence behavior.
Studies showed that various comorbid disorders were also related to non-adherence to antihyperlipidemic medication. Participants in the current study who had more comorbid conditions exhibited higher non-adherence than those with fewer comorbid diseases. Our study opposed the findings from previous studies, revealing that a higher number of comorbidities is associated with a lower non-adherence rate. The probability of non-adherence decreases by 4% for each comorbidity that is present58. This has been evident since the initial comorbidity, which has resulted in a 5% reduction in non-adherence64,65. On the other hand, the absence of concurrent illnesses is associated with a 59% increase in the likelihood of non-adherence66.
We also looked at the correlation between medication adherence and other comorbidities, such as obesity, CVDs, and type 2 diabetes, but we were unable to uncover any statistically significant correlations. Further investigation into the various co-occurring conditions could elucidate the fundamental causes of these results. Previous studies revealed that lower non-adherence is linked to cardiovascular disease event history67,68, patients receiving antiplatelet medication69, and patients having hypertension70. Similarly, less frequent follow-ups and taking medication at night or odd times negatively impact adherence to antihyperlipidemic medication71. Also, it has been demonstrated that patients taking beta-blockers had decreased non-adherence rates. On the other hand, Diabetes has been found to be linked to higher rates of non-adherence52. Furthermore, it was found that various comorbidities had different effects on non-adherence; individuals with the comorbidities experienced increased non-adherence rates, including Alzheimer's disease57, depression57, anxiety72, and chronic obstructive pulmonary disease69.
To the best of our knowledge, there is little information on hyperlipidemia medication non-adherence in Pakistan. The current study attempted to fill this information gap by using a large, nationally representative sample. The current research assessed a range of factors (sociodemographics to medication-related and health-related) associated with non-adherence to antihyperlipidemic medication that had not been thoroughly explored in the preexisting body of literature. The findings of the current study offer important insights on how to improve medication adherence in the local settings, which can be extrapolated to other regions with similar demographics.
Final note and clinical implications
Patients may not adhere to various explanations, including practical, emotional, or perceptual ones, and we cannot tackle these issues without exploring these issues for each particular patient73. Despite the different measurements, each attribute is connected to considerable variance in non-adherence, allowing for adjustment and customization of the therapeutic choice for these individuals. The more of these disorders patients have, the more likelihood of non-adherence is anticipated, and, therefore, healthcare providers should be more concerned.
Despite the lack of systematic counseling in a resource-constrained setting like Pakistan, doctors, at the very least, can direct patients toward dependable services, including pharmacies, health programs, and trustworthy online resources. A recent systematic review recommended additional studies with more sophisticated designs to determine non-adherence predictors and efficient interventions to enhance adherence in CVDs74.
Pakistan is a developing country with many limitations in providing quality health services to its population. In many countries, improving patients' medication adherence has been a significant outcome of quality pharmaceutical services. Non-adherence to the therapy may lead to different problems as a consequence of non-adherence at four levels: individual, institutional, social, and national. Adherence to medications is an essential indicator of the quality of medication management and impacts health outcomes. Moreover, patients’ customized challenges to adherence must be addressed and acknowledged to move patients from the preparation stage to the action stage. This critical stage necessitates questioning patients about their worries regarding statin therapy and what obstacles to statin medication need to be removed. For instance, beginning with a generic statin could be sensible if cost is a concern.
Our findings suggest the prevalence of non-adherence to antihyperlipidemic medication in Pakistan, with significant variation across its provinces and divisions. These results call for tailored interventions to improve medication adherence, especially in provinces and their divisions with high non-adherence rates. Further research is needed to explore the factors contributing to non-adherence in different regions of Pakistan and develop effective strategies to address the issue. Our findings provide baseline statistics for policymakers, healthcare practitioners, and other service providers to plan their future goals and objectives accordingly to cater to the medical needs of this specific population group.
Limitations
Self-reporting was employed to measure non-adherence, which may have led to an underestimation of drug compliance. However, we chose to use the SEAMS questionnaire because it was deemed appropriate for people with low reading levels35,36. The self-reporting pill-counting method was similarly linked to increased adherence measurement validity. An objective evaluation of adherence could be made using pill counts or pharmacy databases, but these tools could not be used in the context of Pakistan. Additionally, data from pharmacy databases and pill counts cannot reveal the kinds of non-adherence (deliberate or otherwise).
Moreover, no causal conclusions can be drawn regarding the relationship between medicine-taking attitudes and non-adherence due to the cross-sectional methodology of the study. The overall relationship of our logit model was relatively high, indicating several potent predictors of non-adherence.
Conclusion
We determined non-adherence among patients taking antihyperlipidemic for primary or secondary prevention of CVDs in a country with constrained resources. Patients with hyperlipidemia generally had high non-adherence rates. We also examined the elements that affect non-adherence to antihyperlipidemic medication among various ethnic groups; some highlighted operational flaws in the healthcare system that require immediate attention. Since non-adherence shouldn’t be viewed as the patient’s fault but rather as a critical warning indicator that needs to be addressed for this significant illness, patients and professionals need to collaborate to address some of the other unknown factors immediately. Antihyperlipidemic medication non-adherence is a multifaceted, multifactorial problem that is abundant and has no simple solution.
Recommendations
There are significant, observable factors that contribute to non-adherence in hyperlipidemic individuals. Healthcare professionals should recognize these traits to approach patients individually and devote more effort to enhancing adherence. Finding the optimum frequency of adherence and exploring factors of non-adherence further, comprehending the particular individual and community behaviors that encourage non-adherence, and examining the generalizability of these predicted factors across contexts and demographics are critical next steps in building on the current work. There is also a need to create new instructional approaches to increase drug adherence. A recent study compared an innovative mHealth strategy to peer counseling to improve non-adherence47.
Moreover, patients with hyperlipidemia generally had high non-adherence rates. Targeting people who were classified as non-adherent and their suggestions will help increase adherence. Therefore, high-quality qualitative designs mixed with new horizons of quantitative research are needed to explore factors in depth.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AJ&K:
-
Azad Jammu and Kashmir
- AOR:
-
Adjusted odds ratio
- BHU:
-
Basic health unit
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular diseases
- DHQ:
-
District head quarter
- FATA:
-
Federally administered tribal areas
- GLM:
-
Generalized linear model
- GIS:
-
Geographic information system
- KP:
-
Khyber Pakhtunkhwa
- LDL:
-
Low-density lipoprotein
- MOs:
-
Medical officers
- OPD:
-
Outpatient department
- RHC:
-
Rural healthcare center
- SEAMS:
-
Self-efficacy for appropriate medication scale
- THQ:
-
Tehsil head quarter
- WHO:
-
World Health Organization
References
Pirillo, A., Casula, M., Olmastroni, E., Norata, G. D. & Catapano, A. L. Global epidemiology of dyslipidaemias. Nat. Rev. Cardiol. 18, 689–700 (2021).
Alwan, A. Global status report on noncommunicable diseases 2010. (2011).
Mihaylova, et al. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 380, 581–590 (2012).
Taylor, F. et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2011(1), (2013).
Guilbert, J. J. The world health report 2002—reducing risks, promoting healthy life. Educ. Health (Abingdon) 16, 230 (2003).
Schuck, R. N., Mendys, P. M. & Simpson, R. J. Jr. Beyond statins: Lipid management to reduce cardiovascular risk. Pharmacother. J. Hum. Pharmacol. Drug Ther. 33, 754–764 (2013).
Shah, R. V. & Goldfine, A. B. Statins and risk of new-onset diabetes mellitus. Circulation 126, e282–e284 (2012).
Liao, J. et al. The NPC1L1 gene exerts a notable impact on the reduction of low-density lipoprotein cholesterol in response to hyzetimibe: A factorial-designed clinical trial. Front. Pharmacol. 13, 755469 (2022).
Mihaylova, B. et al. Cost-effectiveness of statin therapy in categories of patients in the UK. Eur. Heart J. 43, ehac544.2841 (2022).
Lin, F.-J. et al. Cost-effectiveness of statin therapy for secondary prevention among patients with coronary artery disease and baseline LDL-C 70–100 mg/dL in Taiwan. J. Formosan Med. Assoc. 119, 907–916 (2020).
Ratchford, E. V. & Martin, S. S. Statins. Vasc. Med. 22, 442–445 (2017).
Chou, R., Dana, T., Blazina, I., Daeges, M. & Jeanne, T. L. Statins for prevention of cardiovascular disease in adults: Evidence report and systematic review for the US preventive services task force. JAMA 316, 2008–2024 (2016).
Cholesterol Treatment Trialists’ (CTT) Collaboration et al. Efficacy and safety of more intensive lowering of LDL cholesterol: A meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376, 1670–1681 (2010).
World Health Organization. Prevention of cardiovascular disease: guidelines for assessment and management of cardiovascular risk. Geneva: https://www.rethinkobesity.global/global/en/cvd/how-to-communicate-risk-in-cardiovascular-assessments.html (2007).
Morrison, A., Stauffer, M. E. & Kaufman, A. S. Defining medication adherence in individual patients. Patient Prefer Adher. 9, 893–897 (2015).
Raebel, M. A., Schmittdiel, J., Karter, A. J., Konieczny, J. L. & Steiner, J. F. Standardizing terminology and definitions of medication adherence and persistence in research employing electronic databases. Med. Care 51, S11-21 (2013).
Mauskop, A. & Borden, W. B. Predictors of statin adherence. Curr. Cardiol. Rep. 13, 553–558 (2011).
Vlasnik, J. J., Aliotta, S. L. & DeLor, B. Medication adherence: Factors influencing compliance with prescribed medication plans. Case Manag. 16, 47–51 (2005).
Fenton, W. S., Blyler, C. R. & Heinssen, R. K. Determinants of medication compliance in schizophrenia: Empirical and clinical findings. Schizophr. Bull. 23, 637–651 (1997).
Patel, M. X. & David, A. S. Medication adherence: Predictive factors and enhancement strategies. Psychiatry 3, 41–44 (2004).
Gomez Sandoval, Y.-H., Braganza, M. V. & Daskalopoulou, S. S. Statin discontinuation in high-risk patients: A systematic review of the evidence. Curr. Pharm. Des. 17, 3669–3689 (2011).
Rodriguez, F. et al. Association of statin adherence with mortality in patients with atherosclerotic cardiovascular disease. JAMA Cardiol. 4, 206–213 (2019).
Naderi, S. H., Bestwick, J. P. & Wald, D. S. Adherence to drugs that prevent cardiovascular disease: Meta-analysis on 376,162 patients. Am. J. Med. 125, 882-887.e1 (2012).
Banach, M., Stulc, T., Dent, R. & Toth, P. P. Statin non-adherence and residual cardiovascular risk: There is need for substantial improvement. Int. J. Cardiol. 225, 184–196 (2016).
Lemstra, M. & Blackburn, D. Nonadherence to statin therapy: Discontinuation after a single fill. Can. J. Cardiol. 28, 567–573 (2012).
Xu, T. et al. Statin adherence and the risk of stroke: A dose-response meta-analysis. CNS Drugs 31, 263–271 (2017).
Osterberg, L. & Blaschke, T. Adherence to medication. N. Engl. J. Med. 353, 487–497 (2005).
Li, Y.-C. & Huang, W.-L. Effects of adherence to statin therapy on health care outcomes and utilizations in Taiwan: A population-based study. Biomed. Res. Int. 2015, 149573 (2015).
Wu, B. et al. Abstract 11224: Prevalence of statin non-adherence determined by therapeutic drug monitoring (TDM) in patients with uncontrolled hypertension. Circulation 140, A11224–A11224 (2019).
Brown, M. T. & Bussell, J. K. Medication adherence: WHO cares?. Mayo Clin. Proc. 86, 304–314 (2011).
Anselin, L., Syabri, I. & Kho, Y. GeoDa. An introduction to spatial data analysis. In Handbook of applied spatial analysis: Software tools, methods and applications. 73–89 (Berlin, Heidelberg, Springer Berlin Heidelberg, 2009).
GeoDa. Download | GeoDa on Github 1.160. GeoDa https://geodacenter.github.io/download.html (2020).
Arshed, M., Mahmud, A., Minhat, H. S., Lim, P. Y. & Zakar, R. Effectiveness of a multifaceted mobile health intervention (multi-aid-package) in medication adherence and treatment outcomes among patients with hypertension in a low- to middle-income country: Randomized controlled trial. JMIR Mhealth Uhealth 12, e50248 (2024).
Pednekar, P. P. et al. Methods for measuring multiple medication adherence: A systematic review-report of the ISPOR medication adherence and persistence special interest group. Value Health 22, 139–156 (2019).
Culig, J. & Leppée, M. From Morisky to Hill-bone; self-reports scales for measuring adherence to medication. Coll. Antropol. 38, 55–62 (2014).
Risser, J., Jacobson, T. A. & Kripalani, S. Development and psychometric evaluation of the self-efficacy for appropriate medication use scale (SEAMS) in low-literacy patients with chronic disease. J. Nurs. Meas. 15, 203–219 (2007).
Bobrow, K. et al. Mobile phone text messages to support treatment adherence in adults with high blood pressure (SMS-text adherence support [StAR]): A single-blind, randomized trial. Circulation 133, 592–600 (2016).
Farmer, K. C. Methods for measuring and monitoring medication regimen adherence in clinical trials and clinical practice. Clin. Ther. 21, 1074–1090 (1999) (discussion 1073).
Ca, J., Li, P. & Jv, T. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation 117, 1028–1036 (2008).
Newby, L. K. et al. Long-term adherence to evidence-based secondary prevention therapies in coronary artery disease. Circulation 113, 203–212 (2006).
Jackevicius, C. A., Mamdani, M. & Tu, J. V. Adherence with statin therapy in elderly patients with and without acute coronary syndromes. JAMA 288, 462–467 (2002).
Chowdhury, R. et al. Adherence to cardiovascular therapy: A meta-analysis of prevalence and clinical consequences. Eur. Heart J. 34, 2940–2948 (2013).
Ofori-Asenso, R. et al. Adherence and persistence among statin users aged 65 years and over: A systematic review and meta-analysis. J. Gerontol. Ser. A 73, 813–819 (2018).
Hope, H. F. et al. Systematic review of the predictors of statin adherence for the primary prevention of cardiovascular disease. PLoS ONE 14, e0201196 (2019).
Marzà-Florensa, A. et al. Prevalence of cardioprotective medication use in coronary heart disease patients in South America: Systematic review and meta-analysis. Glob. Heart 17, 37 (2022).
Lemstra, M., Blackburn, D., Crawley, A. & Fung, R. Proportion and risk indicators of nonadherence to statin therapy: A meta-analysis. Can. J. Cardiol. 28, 574–580 (2012).
Arshed, M. et al. Efficacy of mHealth and education-led peer counseling for patients with hypertension and coronary artery disease in Pakistan: Study protocol for a double-blinded pragmatic randomized-controlled trial with factorial design. Trials 24, 448 (2023).
Blaschke, T. F., Osterberg, L., Vrijens, B. & Urquhart, J. Adherence to medications: Insights arising from studies on the unreliable link between prescribed and actual drug dosing histories. Annu. Rev. Pharmacol. Toxicol. 52, 275–301 (2012).
Vrijens, B. et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 73, 691–705 (2012).
Adherence to Long-Term Therapies: Evidence for Action. (World Health Organization, Geneva, 2003)
Esposti, L. D. et al. Direct healthcare costs by level of adherence of a real-world population of statin users in Italy. CEOR 14, 139–147 (2022).
Booth, J. N. et al. Statin discontinuation, reinitiation, and persistence patterns among medicare beneficiaries after myocardial infarction: A cohort study. Circ. Cardiovasc. Qual. Outcomes 10, e003626 (2017).
Phan, D. Q. et al. Statin adherence and mortality in patients aged 80 years and older after acute myocardial infarction. J. Am. Geriatr. Soc. 67, 2045–2049 (2019).
Al-Foraih, M. & Somerset, S. Factors affecting adherence to statins in hypercholesterolemic Kuwaiti patients: A cross-sectional study. Med. Princ. Pract. 26, 35–40 (2017).
Cheetham, T. C. et al. Primary nonadherence to statin medications in a managed care organization. J. Manag. Care Pharm. 19, 367–373 (2013).
Chodick, G. et al. Long-term persistence with statin treatment in a not-for-profit health maintenance organization: A population-based retrospective cohort study in Israel. Clin. Ther. 30, 2167–2179 (2008).
Hickson, R. P. et al. Changes in statin adherence following an acute myocardial infarction among older adults: Patient predictors and the association with follow-up with primary care providers and/or cardiologists. J. Am. Heart Assoc. 6, e007106 (2017).
Batal, H. A., Krantz, M. J., Dale, R. A., Mehler, P. S. & Steiner, J. F. Impact of prescription size on statin adherence and cholesterol levels. BMC Health Serv. Res. 7, 175 (2007).
Osborn, C. Y., Kripalani, S., Goggins, K. M. & Wallston, K. A. Financial strain is associated with medication nonadherence and worse self-rated health among cardiovascular patients. J. Health Care Poor Underserved 28, 499–513 (2017).
Krueger, K. P., Berger, B. A. & Felkey, B. Medication adherence and persistence: A comprehensive review. Adv. Ther. 22, 313–356 (2005).
Simoens, S. & Sinnaeve, P. R. Patient co-payment and adherence to statins: A review and case studies. Cardiovasc. Drugs Ther. 28, 99–109 (2014).
Kriegbaum, M. & Lau, S. R. Medication non-adherence and uncertainty: Information-seeking and processing in the Danish LIFESTAT survey. Res. Soc. Adm. Pharm. 14, 736–741 (2018).
Shakarneh, J. K., Hallak, H. O., Awadallah, H. B., Al-Hamed, D. H. & Khdour, M. R. Necessity and concerns about lipid-lowering medical treatments and risk factors for non-adherence: A cross-sectional study in Palestine. Int. J. Clin. Pract. 74, e13511 (2020).
Said, A. H., Abd Rahim, I. S., Binti Mohamad Zaini, N. N. & Binti Saiful Nizam, N. I. Factors affecting adherence to lipid-lowering drugs: A scoping review. Oman Med. J. https://doi.org/10.5001/omj.2023.67 (2022).
Warren, J. R., Falster, M. O., Tran, B. & Jorm, L. Association of continuity of primary care and statin adherence. PLoS ONE 10, e0140008 (2015).
Di Martino, M. et al. Underuse of lipid-lowering drugs and factors associated with poor adherence: A real practice analysis in Italy. Eur. J. Clin. Pharmacol. 61, 225–230 (2005).
Bruckert, E. et al. Patient characteristics, treatment patterns, and adherence to lipid-lowering therapies following an acute coronary syndrome. Rev. Cardiovasc. Med. 21, 643–650 (2020).
Seamon, K. et al. Predictors of ceasing or reducing statin medication following a large increase in the consumer copayment for medications: A retrospective observational study. Public Health Res. Pract. 30, 29121905 (2020).
Chen, S.-T. et al. Long-term statin adherence in patients after hospital discharge for new onset of atherosclerotic cardiovascular disease: A population-based study of real world prescriptions in Taiwan. BMC Cardiovasc. Disord. 19, 62 (2019).
Wawruch, M. et al. Age-related differences in non-persistence with statin treatment in patients after a transient ischaemic attack. Clin. Drug. Investig. 37, 1047–1054 (2017).
Devaraj, N. K., Mohamed, M. & Hussein, N. Prevalence, factors influencing and knowledge about adherence to lipid-lowering therapy among hyperlipidemia patients. Med. J. Malays. 72, 157–164 (2017).
Korhonen, M. J., Pentti, J., Hartikainen, J., Kivimäki, M. & Vahtera, J. Somatic symptoms of anxiety and nonadherence to statin therapy. Int. J. Cardiol. 214, 493–499 (2016).
Rosenbaum, L. Beyond belief—how people feel about taking medications for heart disease. N. Engl. J. Med. 372, 183–187 (2015).
Arshed, M., Mahmud, A. B., Minhat, H. S., Ying, L. P. & Umer, M. F. Effectiveness of mHealth interventions in medication adherence among patients with cardiovascular diseases: A systematic review. Diseases 11, 41 (2023).
Acknowledgements
We are grateful to Ghulam Hussain Buledi, Suhail Bijarani, Hasan Mujtaba, Ahsanullah Khan, Shakaib Magsi, Nusrat Parveen, Farzana Marwat, Inam Kakar, Farzeen Masood, Ikram Bangash, Inayatullah Khatak, Muhammad Rafi, Dr. Adnan Ashraf, Dr. Naveed Mansoori, Dr. Sajid Sahi, Dr. Irfan Asgher, Usman Ameer, Suhail Tanweer, Laiba Dar, Nusrat Buzdar and Irfan Maqbool for their efforts and support throughout this project. Qatar University funded the publication of this article.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.A., M.F.U.; Methodology, M.A., M.F.U., M.N.K.; Validation, M.A. and A.F.; formal analysis, M.A.; Investigation, Data collection and Data curation, M.A., M.K., A.H.G., A.B.K., S.Z., A.M.A.; writing—original draft preparation, M.A., M.F.U.; Writing—Review and Editing, M.F.U., M.N.K., A.F. and M.K.; supervision, M.A., M.F.U., M.N.K. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Arshed, M., Umer, M.F., Kiran, M. et al. Prevalence and associated factors of non-adherence to antihyperlipidemic medication: a nationwide cross sectional survey in Pakistan. Sci Rep 14, 20613 (2024). https://doi.org/10.1038/s41598-024-71120-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-71120-z