Abstract
Neoadjuvant radiotherapy is the standard care of locally advanced rectal cancer. Although a majority of patients received the same dose, the curative efficacy varies among individuals. In recent years, cancer treatment has entered the era of precise medical care, and how to identify patients for proper treatment by molecular signature is an important path of individualized therapy. This study aimed to establish and validate a genome-based model for adjusting radiation dose (GARD) for Chinese locally advanced rectal cancer through gene expression microarrays, and to evaluate the response of the GARD model in predicting the efficacy of neoadjuvant radiotherapy. Fresh-frozen primary tumor from 64 patients with locally advanced rectal cancer undergoing neoadjuvant radiotherapy from 2015 to 2018 were included. The gene expression profile was analyzed using Affymetrix 3000Dx gene-chip scanner. The radiosensitivity index (RSI) and GARD were calculated using the pGRT™ algorithm. Neoadjuvant rectal cancer score (NAR) was selected as efficacy evaluation indicators. Patients were divided into high and low NAR scoring groups, and two-sample t-test was used to analyze the differences in GARD values between different NAR subgroups. ROC curves were used to calculate the cut-off values and the area under the curve (AUC) for assessing the validity of the GARD models. The personalized radiation dose ( pGRT dose )can be computed using the formula nd = GARD / (α + βd). Among patients, 1.5% T2, 46.3% T3, and 52.2% T4. Wherein pCR (n = 10; 15.6%) and no pCR (n = 54; 84.4%). The median NAR is 8.43 (rang from 0 to 50.34, IQR 3.75–14.98). NAR > 8.43 (n = 27; 42.2%) and NAR ≤ 8.43 (n = 37; 57.8%), suggesting that there are significant individual differences in clinical efficacy of patients with similar tumor stages and under the same treatment conditions. The median RSI is 0.48 (rang from 0.22 to 0.92, IQR 0.41–0.55). Median GARD was 18.40 rang from (rang from 2.26 to 37.52, IQR 14.94–22.28) within tumor tissue, suggesting individual differences in the efficacy of radiation therapy. The RSI value was significantly lower in the NAR low group (NAR ≤ 8.43) than in NAR high group (NAR > 8.43) (0.44 vs. 0.54, p = 0.0003). The GARD value was significantly higher in the NAR low group (NAR ≤ 8.43) than in NAR high group (NAR > 8.43) (21.01 vs. 15.88, p = 0.0004). Using the Receiver Operating Characteristic (ROC) curve analysis, a GARD threshold of 17 was identified as optimal, covering 37.5% of the 64-patient sample, with an area under the curve (AUC) of 0.75. In the external validation cohort, the high GARD score group demonstrated superior DFS compared to the low GARD score group(p < 0.001). Only 17% of patients had pGRT dose within the guideline recommended dose (45–50 Gy). The differences in NAR values among LARC patients receiving standard neoadjuvant radiotherapy suggest significant individual differences in clinical outcomes among patients with similar tumor stage and the same treatment conditions. Patients with a GARD value exceeding 17 exhibit a more favorable prognosis. Our results suggest that the gene expression-based pGRT™ algorithm has good efficacy prediction performance in preoperative concurrent radiotherapy for locally advanced rectal cancer, suggesting the potential clinical application of this method to guide the designation of individualized radiotherapy doses.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is one of the common malignant tumors in the digestive system1.Recent research data suggests a continuous increase in the incidence of rectal cancer. The National Central Cancer Registry (NCCR) of China reported 376,300 newly diagnosed cases and 191,000 deaths due to CRC in 20152,3.The treatment approach for locally advanced rectal cancer (AJCC stage T3-4 and/or N+) involves neoadjuvant chemoradiotherapy followed by total mesorectal excision (TME) and postoperative/adjuvant chemotherapy4,5. Multiple clinical trials have demonstrated that pCR rate after neoadjuvant chemoradiotherapy can reach 10-27%6,7,8, with downstaging rates of approximately 80%9,10, indicating that the majority of patients achieve the expected response under current radiation dosage conditions. However, there are still 20% of patients who exhibit a poor response to chemoradiotherapy with minimal downstaging.
In recent decades, precise and personalized treatment of tumors has been the focus of scientists11. The National Institutes of Health in the United States defines precision medicine as an approach to disease prevention and treatment that takes into account individual differences based on environment, genetis, and lifestyle12,13. While the genomic era has transformed the treatment landscape with chemotherapy and targeted biologics14, its application to radiation therapy has not been widely adopted. Currently, there is a lack of biomarkers to guide the development of radiation treatment strategies. The dosing regimens for radiation therapy still follow a one-size-fits-all approach, where the same dose is used for all patients with the same disease, assuming that every patient has an equal chance of benefiting from radiation therapy. This treatment model is based on the assumption that each patient will benefit from the same radiation dose, without considering their unique biology and tumor characteristics11. For patients with locally advanced rectal cancer, the standard dose for preoperative neoadjuvant radiation therapy is 45 Gy to the pelvic area (including the primary tumor and metastatic lymph nodes, rectal mesentery, presacral tissue, as well as the internal iliac and obturator lymphatic drainage areas), with or without additional radiation to the rectosigmoid area, totaling 50.4 Gy. A phase II study led by Ballonoff aimed to increase the radiation dose in combination with synchronous capecitabine treatment for stage II/III rectal cancer. The dose to the primary tumor was escalated from the standard 50 Gy to 55 Gy in 25 fractions, while the dose to the pelvic area remained at 45 Gy in 25 fractions. The pCR rate was 37.5%15. Additionally, a systematic review and meta-analysis by Burbach et al. suggested that increasing the radiation dose to ≥ 60 Gy in preoperative radiation therapy for LARC achieved higher pCR rates16, indicating that higher radiation doses may lead to improved pCR rates for some patients. This suggests that the standard radiation dose of 45 Gy to 50.4 Gy may be insufficient for certain patients. Our previous research found that some patients in the long-term follow-up after treatment developed late complications such as pelvic fibrosis, indicating that this group of patients may have received excessive radiation therapy17,18. Therefore, it is evident that the same radiation dose can produce different clinical outcomes and varying degrees of radiation injury, highlighting the need for individualized radiation therapy doses for each patient. Thus, the key to improving efficacy and enhancing patients’ quality of life lies in selecting personalized radiation therapy doses.
In previous studies, the definition of precision radiation therapy usually referred to the anatomical and geometric accuracy in delivering a fixed radiation dose to the tumor target. It was generally described based on clinical features, such as tumor size, tumor response, and imaging characteristics. Although previous research has indicated the existence of biological differences determining tumor and normal tissue responses to radiation, no clinical strategies have been developed so far to integrate these biological differences into clinical practice for guiding radiation therapy strategies. Identifying predictive factors for tumor response and determining pathways for early response will be crucial for future individualized and precision treatments. With the further development of chip technology and DNA/RNA sequencing techniques, the cost of detection is decreasing, making it possible to use high-throughput genomics approaches to guide treatment. Future research may discover more precise assessment methods based on genomic information, providing more information and a foundation for exploring the occurrence and development mechanisms of colorectal cancer and playing a greater role in precision radiation therapy for colorectal cancer19,20.
Genomic research has indicated that biological heterogeneity is a key characteristic of cancer21. Previously, the research team led by EschrichS developed a gene expression-based Radiosensitivity Index (RSI) as a predictive marker for cell survival fraction at 2 Gy (SF2). Using the expression of ten specific genes extracted through systems biology approaches, a linear regression model was constructed to predict SF2 values for 48 cancer cell lines from nine different cancer types22,23. The RSI index based on gene expression was validated in vitro cell experiments and also in various tumor types24,25,26,27,28,29,30,31. These studies revealed inconsistency in clinical benefits from radiotherapy among patients with significant genomic (i.e., radiosensitivity) differences. Therefore, incorporating individual biological variations into radiotherapy protocols is a crucial step toward achieving precision radiation therapy. Javier F. from the Moffitt Cancer Centerdeveloped a gene expression-based Radiosensitivity Index using a linear quadratic model to establish GARD as the foundation for precise radiation therapy of tumors. This model can predict the effectiveness of radiotherapy and adjust radiation doses based on radiation sensitivity to achieve optimal treatment outcomes. The model has been validated in more than 20 solid tumors, such as esophageal cancer, breast cancer, head and neck cancer, glioblastoma, and pancreatic cancer. In the future, genomic-guided GARD models are expected to be utilized for designing clinical trials in radiation therapy, enabling precise radiation treatment of tumors.
Currently, models used to predict the therapeutic effects of neoadjuvant radiotherapy in rectal cancer typically utilize gene expression levels to assess the radiosensitivity of tumor patients and forecast the outcomes of radiation therapy. However, these multi-gene expression models focus exclusively on the intrinsic sensitivity of tumors and do not provide information related to radiation dosage, which limits their predictive capability32,33.This study aims to RSI of patients based on gene expression related to radiation sensitivity in Chinese patients with LARC and establish a GARD(A model combining RSI and radiation physical dose to quantify the biological effects of a given dose on individual patients) model based on the RSI index. To assess the efficacy of neoadjuvant therapy in LARC, George et al.34. proposed a surrogate endpoint called the NAR. The predictive value of NAR has been validated in several retrospective and prospective studies. Therefore, the effectiveness of this model in predicting the outcomes of neoadjuvant radiotherapy for Chinese patients with locally advanced rectal cancer will be evaluated using the NAR score as the outcome variable.
This study will provide a theoretical basis for subsequent personalized radiation therapy of rectal cancer based on its genomic characteristics, aiming to improve prognosis, reduce side effects, and enhance patient survival by optimizing treatment strategies.
Methods
Patients and samples
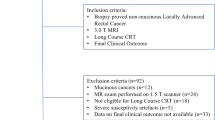
Patients with locally advanced rectal cancer who underwent neoadjuvant chemoradiotherapy followed by surgery in Fujian Medical University Union Hospital (Fujian, China) between 2015-01-01 and 2018-12-31 were consecutively enrolled in this study based on the following inclusion criteria: histologically proven rectal adenocarcinoma, no distant metastasis; Eastern Cooperative Oncology Group performance status of 0–1; fresh frozen biopsy tumor tissue samples available; neoadjuvant concurrent chemoradiotherapy with total mesorectal excision (TME) surgery.
To further limit potential confounding factors along these lines, included patients were given similar chemoradiotherapy strategy. A total of 64 patients with LARC met the criteria for inclusion, all the patients treated with preoperative radiotherapy plus Capecitabine standardised neoadjuvant chemo radiotherapy regime consisting of Capecitabine (Xeloda®, 825 mg/m2, Welwyn Garden City, United Kingdom), twice daily and one dose of radiotherapy (50.4 Gy in 28 fractions of 180 cGy/fr).
Clinical staging was determined according to the TNM classification of the AJCC/UICC (8th edition) published in 201635, based on the synthesis of a pile of medical history and physical examination supplemented by imaging and pathology data.
Pathologic examination and definition of pathological complete response (pCR) and NAR
pCR was defined as the absence of viable cells in the primary tumor and lymph nodes (ypT0N0) of surgical specimens as evaluated by two pathologists. NAR scores were calculated using the following formula as reported previously9: [5pN-3(cTpT) + 12]2/9.61, where cT = 3–4, pT = 0–4, and pN = 0–2.
Definitions of RSI and GARD
RSI was developed by Javier and his colleagues as a molecular estimate for cellular survival fraction at 2 Gy, based on the expression of ten specific genes ranked from lowest to highest (Eq. 1): RSI= − 0·0098009 * AR + 0·0128283 * cJun + 0·0254552 * STAT1–0·0017589 * PKC – beta – 0·0038171 * RelA + 0·1,070,213 * cABL – 0·0002509 * SUMO1–0·0092431 * PAK2–0·0204469 * HDAC1–0·0441683 * IRF1.
They also derived GARD scores using the linear quadratic model, RSI, and the standard radiation dose and fractionation schedule for each patient. The calculation for GARD is similar to biologically effective dose36 (Eq. 2: E = nd(α + βd)), except that patient-specific α is derived by substituting radiosensitivity index for survival (S) in Eq. 1, where dose (d) is fractionated dose, n is Number of fractions, and β is a constant (0·05/Gy²).α=(-0.5lnRSI)-0.137. A higher GARD value predicts a better radiotherapy effect29. After establishing the optimal cut-off value for GARD through analysis of the ROC curve, the personalized radiation therapy dose (pGRT dose) can be computed using the formula nd = GARD / (α + βd).
Procedures
We assayed tumors from patients enrolled in the study on Affymetrix Hu-RSTA-2a520709 (Aff ymetrix; Santa Clara, CA, USA), which contains approximately 60 000 probesets representing 25 000 genes. Chips were normalised using iterative rank-order normalization38. Batch effects were reduced using partial-least squares.
To calculate radiosensitivity index scores for this cohort, we normalised gene expression values from Affymetrix U133A CEL files using the robust multiarray average (RMA) algorithm39 and did linear scaling to avoid negative values.
Statistical analysis
Statistical analysis was performed using SPSS version 24.0 (SPSS, INC, Chicago). Categorical variables were presented as frequencies and percentages, and assessed using Chi-square or Fisher’s exact test, when appropriate. Continuous variables were described as means and standard deviation, and assessed via the analysis of variance (ANOVA) test. P < 0.05 was considered statistically significant.
The Mann Whitney U test was used for variables that were not normally distributed. Spearman rank correlation was also used in analyses of correlations between variables. Kaplan-Meier log-rank tests were conducted to assess differences in overall survival (OS) and disease-free survival (DFS) between high and low GARD score groups. These analyses were performed using R (version 4.1.2) with the “survival” (version 3.5) and “survminer” (version 0.9.9) packages.
Results
Patients characteristics
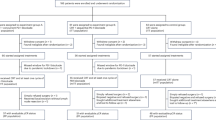
Among the 64 patients, T2 accounts for 3.1%, T3 accounts for 45.3%, T4 accounts for 51.6%; N + accounts for 98.4%. Ten patients (15.6%) achieve pCR. The median NAR is 8.43 (range: 0-50.34, IQR was 3.75 to 14.98). There are 27 cases (42.2%) with NAR > 8.43 (NAR high group) and 37 patients (57.8%) with NAR ≤ 8.43 (NAR Low group) (Table 1).
RSI and GARD value for 64 locally advanced rectal cancer samples
The gene expression-based RSI, which can estimate the biological heterogeneity in tumor intrinsic radiosensitivity, was calculated by Eq. 1. Here we show the median RSI values for 64 locally advanced rectal cancer samples is 0.48 (rang from 0.22 to 0.92, IQR 0.41–0.55) (Fig. 1A). The distribution of RSI values demonstrates a Unimodal peak (Fig. 1A). Then, we generate GARD scores for these patients which received 50.4 Gy as a standard dose, the median GARD is 18.40 (rang from 2.26 to 37.52, IQR 14.94–22.28). Similar to the RSI distribution, GARD scores show heterogeneity of clinical effect with a Uni-modal distribution (Fig. 1B). There was no significant difference in RSI (0.43 ± 0.1 VS 0.49 ± 0.11 p = 0.22)and GARD score (21 ± 6.4 VS 18 ± 5.7 p = 0.22) between the pCR group and the non-pCR group, ( Supplementary Fig. 1A, B).
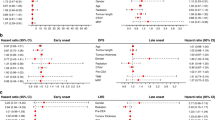
A higher GARD score predicts a higher radiation therapeutic effect
The correlation between GARD and NAR was shown in Fig. 2A, GARD has a significant negative correlation with NAR with a correlation coefficient of -0.36 (P = 0.0033). The GARD scores are significantly higher in the NAR-low group (NAR ≤ 8.43) than in NAR-high group (NAR > 8.43) (21.01 vs. 15.88, p = 0.0004) (Fig. 2B). Using NAR state (low = 0, high = 1) as the outcome variable, ROC curve is used to analyze the predictive effect of GARD on neoadjuvant radiotherapy in patients with LARC patients. According to the Receiver Operating Characteristic (ROC) curve analysis, a GARD value of 17 is identified as the optimal classification threshold. This accounts for 37.5% of the 64 patient sample. With GARD = 17 as the threshold, the sensitivity of this model for predicting is 66.67%, specificity is 81.08%, positive predictive rate is 72%, and negative predictive rate is 76.9%, area under the curve (AUC) is 0.759 (Fig. 2C).
In our cohort, Kaplan-Meier analysis revealed a trend towards improved disease-free survival (DFS) (71% vs. 57%, p = 0.273) and overall survival (OS) (92%vs.75%, p = 0.09) in patients with high GARD scores compared to those with low scores, respectively (Fig. 3A, B). In the external validation cohort GSE40492, we standardized the cut-off for GARD scores using the same percentile (37.5th percentile) to adjust for technical variations due to different sampling methodologies. Kaplan-Meier survival analysis indicated that patients with high GARD scores exhibited significantly better disease-free survival (DFS) compared to those with low scores, with five-year DFS rates of 72% and 57%, respectively (p = 0.049) (Fig. 3C).
Clinical significance of GARD
among 64 patients with locally advanced rectal cancer in China, 40 cases (62.5%) had GARD > 17, while 24 cases (37.5%) had GARD ≤ 17. This result suggests that a significant proportion of patients cannot achieve favorable outcomes with neoadjuvant radiotherapy (Fig. 4B).We subsequently defined the pGRT dose required to achieve a GARD value of 17. The pGRT dose can be computed using the formula nd = GARD / (α + βd). where dose (d) is fractionated dose, n is Number of fractions, and β is a constant (0·05/Gy²).α=(-0.5lnRSI)-0.1. By inputting each patient’s personalized tissue-specific α and GARD17, calculated from RSI into the formula, the patient’s pGRT dose can be determined. The personalized genomic RT dose for each patient is represented by the blue line in the graph. The actual empiric dose received by each patient is marked by the dots (Fig. 4A). The results showed that only 17% of patients had pGRT doses within the recommended range (45–55 Gy) according to guidelines (Fig. 4C). Additionally, 38% of patients had pGRT doses higher than 55 Gy, indicating that these patients may not achieve optimal treatment outcomes with the current radiation dose. Furthermore, 45% of patients had pGRT doses lower than 45 Gy.
Discussion
In recent decades, precision treatment of tumors has been a focus of research. Scientists have been working diligently to transform current general clinical treatment models into more precise personalized treatment approaches, aiming to maximize treatment efficacy and improve patients’ quality of life. In the field of radiation oncology, researchers have made efforts in various aspects, including altering fractionation dose, fractionation techniques, shortening treatment duration, optimizing physical techniques, selecting radiation sources, overcoming hypoxia and proliferation, tumor molecular imaging. However, there has been limited progress in predicting individualized radiation therapy doses, particularly through the use of biomarkers. As mentioned in the introduction of this article, regardless of differences in tumor staging, age, weight, and other relevant factors, the dose of neoadjuvant radiotherapy for locally advanced rectal cancer (LARC) remains uniform at 45–50.4 Gy/25–28 fractions for all patients. However, under consistent radiation dose conditions, patients do not achieve consistent treatment outcomes or experience consistent toxic side effects. There is a pCR rate of 10–27%, but also around 20% of cases with no response, and 3–5% of patients develop severe pelvic fibrosis as a result of radiation therapy. Therefore, exploring a method to predict the response of patients to radiochemotherapy and subsequently devising individualized radiation doses has become an urgent research topic.
The use of surrogate endpoints, such as the NAR score, aids in predicting long-term outcomes like overall and disease-free survival based on initial clinical data. Validated across multiple studies, the NAR score offers an immediate assessment of neoadjuvant radiotherapy efficacy. A cohort study of 787 patients at our research center showed that using the median NAR score as a cutoff, it serves as a reliable short-term endpoint for survival outcomes in Chinese patients with locally advanced rectal cancer. Kaplan-Meier analysis further revealed a significant survival advantage for patients with NAR ≤ 8.43, demonstrating a five-year survival rate of 78%, compared to 52% for those with NAR > 8.43 (p < 0.001) (Supplementary Fig. 2), with a concordance index of 0.681, outperformed pCR (0.59), CEA (0.58), and CA199 (0.59) in predicting prognosis. Consequently, the NAR score has been adopted as the outcome variable for evaluating the efficacy of neoadjuvant radiotherapy in this patient population.In the cohort of 64 patients with locally advanced rectal cancer (LARC), the median Radiosensitivity Index (RSI) was 0.48 (range: 0.22–0.92, IQR: 0.41–0.55), and the median Genomic Adjusted Radiation Dose (GARD) value was 18.40 (range: 2.26–37.52, IQR: 14.94–22.28). The low NAR group had significantly lower RSI values compared to the high NAR group (0.44 vs. 0.54, p = 0.0003). Additionally, the low NAR group had significantly higher GARD values compared to the high NAR group (21.01 vs. 15.88, p = 0.0004). There was no significant difference in RSI and GARD score between the pCR group and the non-pCR group (RSI, 0.43 ± 0.1 vs. 0.49 ± 0.11, p = 0.22); (GARD, 21 ± 6.4 vs. 18 ± 5.7, p = 0.22). The absence of a statistically significant difference may be attributed to the small sample size on one hand, and on the other hand, it might be due to the low pCR rate in rectal cancer, which results in a reduced number of cases in the pCR group. This might also suggest that using the NAR score could reflect tumor tissue radiosensitivity more effectively than the pCR indicator. These results indicate that the high NAR group, which had a worse prognosis, exhibited higher RSI scores, indicating increased radiation resistance, and lower GARD values, suggesting a lower biological dose effect. Lower RSI values and higher GARD values are indicative of better radiation treatment outcomes. When comparing the distribution characteristics of RSI and GARD in Chinese LARC patients with those in Western countries, it can be observed that the median RSI and GARD values of Chinese LARC patients are similar to those of Western countries. However, the distribution patterns of RSI and GARD values in Chinese patients differ from those in Western populations. Chinese LARC patients exhibit a clear unimodal distribution of RSI and GARD values, while Western populations demonstrate a bimodal curve28. Although RSI and GARD have been validated as predictors of radiotherapy efficacy in multiple clinical datasets, their distributions vary significantly among different populations and tumor types. Therefore, assessing the effectiveness of the GARD model in predicting the efficacy of neoadjuvant radiotherapy in Chinese LARC patients holds important clinical significance.
The purpose of studying GARD is to assist in adjusting the clinical radiation therapy prescription dose to match the radiation sensitivity characteristics of each patient’s tumor genomics. Theoretically, higher GARD values indicate better treatment efficacy. Therefore, it is reasonable to test the clinical effectiveness of GARD by examining whether patients with higher GARD values have better clinical outcomes. In this study, we used NAR as the outcome variable and performed ROC curve analysis to evaluate the predictive performance of GARD for neoadjuvant radiotherapy efficacy in Chinese LARC patients. The results showed that using an RSI threshold of 0.50 and a GARD threshold of 17, both models exhibited the same predictive efficacy. The sensitivity for predicting radiotherapy was 66.67%, specificity was 81.08%, positive predictive value was 72%, negative predictive value was 76.9%, and the area under the curve (AUC) was 0.759. In our cohort, Kaplan-Meier analysis indicated a trend towards better disease-free survival (DFS) and overall survival (OS) in patients with high GARD scores compared to those with low scores. Specifically, the DFS was 71% versus 57% (p = 0.273), and the OS was 92% versus 75% (p = 0.09) (Fig. 3A, B). In the external validation cohort GSE40492, the five-year DFS rate for the high GARD score group was 72%, while for the low GARD score group, it was 57% (Fig. 3C).These findings suggest that GARD can effectively reflect the neoadjuvant radiotherapy outcomes in LARC patients.
Furthermore, a key potential application of this model is to use the GARD threshold to calculate genome-based radiation doses in order to enhance the clinical benefits for patients. GARD is not just a predictive indicator or biomarker for clinical prognosis but a model that can be used to evaluate radiation doses to match individual tumor radiation sensitivity. Therefore, using a GARD threshold of 17 and the calculation formula, pGRTdose for each patient, which may lead to better neoadjuvant radiotherapy outcomes, can be derived based on their RSI values. The results showed that only 17% of patients had pGRTdose within the recommended dose range (45–50 Gy) according to guidelines, while 38% of patients had pGRTdose higher than 55 Gy, suggesting that this subgroup of patients may not achieve favorable treatment outcomes with the existing radiation dose. Additionally, 45% of patients had pGRTdose lower than 45 Gy, indicating that this subgroup of patients may achieve good treatment outcomes with a lower radiation dose. Therefore, in the future, we may be able to calculate pGRTdose for each patient based on their genomic radiation sensitivity represented by the RSI index, which would allow for appropriate dose reduction in radiation-sensitive patients to alleviate radiation reactions without compromising prognosis, and dose escalation or change of treatment strategy in radiation-resistant patients, such as combination with sensitizers or alternative treatment modalities.
The use of brachytherapy to boost the dose delivered to the gross tumor volume (GTV) in rectal cancer radiotherapy is a promising approach with emerging evidence for favorable long-term outcomes40. The RSI based on genomic radiosensitivity, can theoretically be applied to brachytherapy models as well. However, due to significant differences in dosage and radiation sources compared to conventional radiotherapy in close-distance treatments, varying radiobiological effects may occur. Therefore, further validation through clinical cohort studies is necessary to clarify these aspects.
However, in our clinical cohort study, a limited sample size introduces significant challenges, primarily diminishing the study’s statistical power which hampers the detection of genuine effects such as treatment efficacy. Moreover, a small sample size constrains the generalizability of the findings and impedes effective subgroup analysis. Our model did not consider the individual variations in radiation sensitivity of normal tissues, which could further enhance the personalization of clinical radiation prescription doses. Additionally, although we used the RSI index based on gene expression as the basis for modeling, the calculation of GARD could incorporate other measures of radiation sensitivity and further expand to include other biological parameters, such as hypoxia, DNA repair, proliferation, and immune system indicators.
In summary, neoadjuvant chemoradiotherapy remains the cornerstone for managing locally advanced rectal cancer, yet treatment responses vary significantly among individuals due to biological heterogeneity. The paradigm of cancer care has shifted towards precision medicine, which involves tailoring treatments based on the molecular profiles of individual tumors. This approach is informed by human genome sequencing, which facilitates targeted therapy according to each patient’s genetic makeup, lifestyle, and environmental factors, as described by the National Institutes of Health (NIH). In this context, traditional radiation therapy, which applies uniform doses across all patients, is being re-evaluated. Our study introduces the GARD model, which utilizes a gene chip to predict individual responses to neoadjuvant radiotherapy in Chinese patients with locally advanced rectal cancer. This model represents a significant step towards integrating genomic data into clinical practice, enabling personalized radiation therapy strategies based on high-throughput genomic analysis. By offering a method to stratify patients by risk and personalize treatment plans, this research enhances the precision of radiotherapy and provides critical insights into the mechanisms driving colorectal cancer, thus laying a theoretical foundation for guiding future precision radiotherapy in rectal cancer treatment.
Conclusion
In summary, the GARD model based on the combination of RSI and radiation physical dose can well predict the efficacy of neoadjuvant radiotherapy in patients with colorectal cancer, and high GARD score indicates the high efficacy. A clinical model with GARD = 17 (37.5%) as the critical value calculate the personalized radiation dose for colorectal cancer patients. Only a small number of patients have a pGRT dose within the recommended range (45–55 Gy). This pGRT™ algorithm based on gene expression has potential clinical application value in preoperative concurrent radiotherapy for locally advanced rectal cancer and can be used to guide the specification of individualized radiotherapy doses.
Data availability
External validation datasets GSE40492 were obtained from Gene Expression Omnibus (http://www.ncbi.nlm.nih.gov/geo/). The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality Worldwide for 36 cancers in 185 countries. CA Cancer J. Clin.71(3), 209–249 (2021).
Chiang, T. Y. et al. Colorectal cancer in Taiwan: A case-control retrospective analysis of the impact of a case management programme on refusal and discontinuation of treatment. J. Adv. Nurs.74(2), 395–406 (2018).
Hsu, S. H. et al. The association between hypertriglyceridemia and colorectal cancer: A long-term community cohort study in Taiwan. Int. J. Environ. Res. Public. Health19(13), (2022).
Schrag, D. et al. Preoperative treatment of locally advanced rectal cancer. N Engl. J. Med.389(4), 322–334 (2023).
Akiyoshi, T. et al. Non-operative management after chemoradiotherapy plus consolidation or sandwich (induction with bevacizumab and consolidation) chemotherapy in patients with locally advanced rectal cancer: A multicentre, randomised phase II trial (NOMINATE trial). BMJ Open.12(3), e055140 (2022).
Sato, K. et al. Comparable regional therapeutic effects between neoadjuvant chemotherapy and neoadjuvant chemoradiotherapy for locally advanced lower rectal cancer in terms of histopathological analysis. Mol. Clin. Oncol.10 (6), 619–624 (2019).
Boublikova, L. et al. Total neoadjuvant therapy in rectal cancer: The evidence and expectations. Crit. Rev. Oncol. Hematol.192, 104196 (2023).
Lin, W. et al. Surgical outcomes in total neoadjuvant therapy for rectal cancer versus standard long-course chemoradiation: A systematic review and meta-analysis of randomized controlled trials. Ann. Surg.279(4), 620–630 (2024).
George, T. J., Allegra, C. J. & Yothers, G. Neoadjuvant rectal (NAR) score: A new surrogate endpoint in rectal cancer clinical trials. Curr. Colorectal Cancer Rep.11(5), 275–280 (2015).
Troester, A. M. & Gaertner, W. B. Contemporary management of rectal cancer. Surg. Open. Sci.18, 17–22 (2024).
Weiser, M. R. Rectal cancer: Time for precision medicine?. Ann. Surg. Oncol.23(1), 12–15 (2016).
Fradkin, J. E., Hanlon, M. C. & Rodgers, G. P. NIH precision medicine initiative: Implications for diabetes research. Diabetes Care39(7), 1080–1084 (2016).
Roper, N. et al. The landscape of precision cancer medicine clinical trials in the United States. Cancer Treat. Rev.41 (5), 385–390 (2015).
Roeder, F. et al. Recent advances in (chemo-)radiation therapy for rectal cancer: A comprehensive review. Radiat. Oncol.15(1), 262 (2020).
Burbach, J. P. et al. Impact of radiotherapy boost on pathological complete response in patients with locally advanced rectal cancer: A systematic review and meta-analysis. Radiother Oncol.113(1), 1–9 (2014).
Shenghui, et al. Factors influencing delayed anastomotic leakage and clinical characteristics after rectal cancer preservation surgery. Chin. J. Gastrointest. Surg.19(04), 390–395 (2016).
Pan, C. et al. Diagnosis and treatment of pelvic wall and intestinal fibrosis with low bowel obstruction after neoadjuvant chemoradiotherapy for rectal cancer. Chin. J. Gastrointest. Surg.18(11), 1092–1097 (2015).
Situ, Y. et al. MRN (MRE11-RAD50-NBS1) complex in human cancer and prognostic implications in colorectal cancer. Int. J. Mol. Sci.20(4), (2019).
Lawrence, M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature. 499 (7457), 214–218 (2013).
Dey, A. et al. Recent advancements, limitations, and future perspectives of the use of personalized medicine in treatment of colon cancer. Technol. Cancer Res. Treat.22, 15330338231178404 (2023).
Eschrich, S. et al. Systems biology modeling of the radiation sensitivity network: A biomarker discovery platform. Int. J. Radiat. Oncol. Biol. Phys.75(2), 497–505 (2009).
Zhao, P. et al. Identification of hub genes and potential molecular mechanisms related to radiotherapy sensitivity in rectal cancer based on multiple datasets. J. Transl Med.21 (1), 176 (2023).
Fontana, E. et al. Context matters-consensus molecular subtypes of colorectal cancer as biomarkers for clinical trials. Ann. Oncol.30 (4), 520–527 (2019).
Torres-Roca, J. F. et al. Prediction of radiation sensitivity using a gene expression classifier. Cancer Res.65 (16), 7169–7176 (2005).
Ahmed, K. A. et al. The radiosensitivity index predicts for overall survival in glioblastoma. Oncotarget. 6 (33), 34414–34422 (2015).
Strom, T. et al. Radiosensitivity index predicts for survival with adjuvant radiation in resectable pancreatic cancer. Radiother Oncol.117 (1), 159–164 (2015).
Torres-Roca, J. F. et al. Integration of a radiosensitivity molecular signature into the assessment of local recurrence risk in breast cancer. Int. J. Radiat. Oncol. Biol. Phys.93(3), 631–638 (2015).
Ahmed, K. A. et al. Differences between colon cancer primaries and metastases using a molecular assay for tumor radiation sensitivity suggest implications for potential oligometastatic SBRT patient selection. Int. J. Radiat. Oncol. Biol. Phys.92(4), 837–842 (2015).
Scott, J. G. et al. A genome-based model for adjusting radiotherapy dose (GARD): a retrospective, cohort-based study. Lancet Oncol.18 (2), 202–211 (2017).
Yuan, Z. et al. Modeling precision genomic-based radiation dose response in rectal cancer. Fut. Oncol.16(30), 2411–2420 (2020).
Tobiasz, J. et al. Multivariate piecewise linear regression model to predict radiosensitivity using the association with the genome-wide copy number variation. Front. Oncol.13, 1154222 (2023).
Qin, F. et al. A novel high-risk model identified by epithelial-mesenchymal transition predicts prognosis and radioresistance in rectal cancer. Mol. Carcinog., (2024).
Domingo, E. et al. Identification and validation of a machine learning model of complete response to radiation in rectal cancer reveals immune infiltrate and TGFbeta as key predictors. EBioMedicine. 106, 105228 (2024).
Smith, J. J. & Garcia-Aguilar, J. Advances and challenges in treatment of locally advanced rectal cancer. J. Clin. Oncol.33 (16), 1797–1808 (2015).
Amin, M. B. et al. The Eighth Edition AJCC Cancer staging Manual: Continuing to build a bridge from a population-based to a more personalized approach to cancer staging. pp. 93–99. (2017).
Hall, E. J. & Giaccia, A. J. Radiobiology for the RadiologistVol. 6 (Lippincott Williams & Wilkins, 2006).
Jeong, J., Shoghi, K. I. & Deasy, J. O. Modelling the interplay between hypoxia and proliferation in radiotherapy tumour response. Phys. Med. Biol.58 (14), 4897–4919 (2013).
Welsh, E. A. et al. Iterative rank-order normalization of gene expression microarray data. BMC Bioinform.14, 153 (2013).
Bolstad, B. M. et al. A comparison of normalization methods for high density oligonucleotide array data based on variance and bias. Bioinformatics. 19 (2), 185–193 (2003).
Saeedian, A. et al. Complication and response assessment of high-dose-rate endorectal brachytherapy boost in neo-adjuvant chemoradiotherapy of locally advanced rectal cancer with long-term outcomes. J. Contemp. Brachytherapy. 15 (2), 117–122 (2023).
Acknowledgements
Not applicable.
Funding
This work was supported by National Natural Science Foundation of Fujian Province, China (2022J02037), Fujian provincial health technology project (No. 2021CXA011), Excellent Young Scholars Cultivation Project of Fujian Medical University Union Hospital (2022XH034Z), and Fujian Provincial Natural Science Foundation of China (No.2020J011014).
Author information
Authors and Affiliations
Contributions
RZ and BX conceived the funding acquisition and supervision. HX and YQW performed the bioinformatics analysis. YNL, ZYL and HX, LJZ prepared the manuscript. YL prepared Fig. 3. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of Fujian Medical University Union Hospital. All patients had written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xia, H., Li, Z., Lin, Y. et al. Validation of a genome-based model for adjusting radiotherapy dose (GARD) in patients with locally advanced rectal cancer. Sci Rep 14, 21572 (2024). https://doi.org/10.1038/s41598-024-72818-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-72818-w