Abstract
The triglyceride glucose (TyG) index has been suggested as a reliable substitute to indicate insulin resistance. Several studies have identified the association between the TyG index and cardiovascular disease. However, the association between the TyG index and the incidence of myocardial ischemia in patients with minimal to moderate coronary artery disease (CAD) has not been clearly assessed. We aimed to investigate the association between the TyG index and the incidence of myocardial ischemia in patients with minimal to moderate CAD. A total of 1,697 patients who underwent coronary computed tomography angiography (CTA) examinations and had minimal to moderate CAD were retrospectively included in the study. The TyG index and computed tomography–derived fractional flow reserve (CT-FFR) were used to assess insulin resistance (IR) and myocardial ischemia, respectively. Myocardial ischemia was defined as a CT-FFR value ≤ 0.80. Logistic regression models were used to explore the associations between the TyG index and myocardial ischemia. The incidence of myocardial ischemia was higher in the highest TyG index tertile (T3) group than in the lowest TyG index tertile (T1) group. After adjusting for other variables, the T3 group remained associated with a higher risk of myocardial ischemia than the T1 group did (OR, 1.43; 95% CI, 1.01–2.04; p = 0.047). A 1- standard deviation (SD) increase in the TyG index was correlated with a 19–24% elevated risk of myocardial ischemia when regarding the TyG index was considered as a continuous variable. Subgroup analysis revealed similar effects. A TyG index is associated with a higher risk of myocardial ischemia detected by CT-FFR in patients with minimal to moderate CAD.
Similar content being viewed by others
Background
Coronary computed tomography angiography (CTA) has achieved significant clinical validation for accurate detection and evaluation of coronary artery disease (CAD)1. Computed tomography–derived fractional flow reserve (CT-FFR) has recently been recommended as a class 2a for evaluating lesion-specific ischemia in patients with intermediate stenosis and it is expected to simplify the clinical care pathway2. In addition, the updated 2022 Coronary Artery Disease Reporting and Data System (CAD-RADS) 2.0 has added CT-FFR as a new modifier for lesion-specific ischemia assessment, as an increasing number of studies have demonstrated excellent consistency between CT-FFR and invasive FFR had better clinical management guidance than coronary CTA alone1.
Most studies have focused on the assessment and management of patients with obstructive CAD (i.e., stenosis > 70% or lumen stenosis > 50%)3. However, previous studies have shown that a significant portion (up to 70%) of patients receiving coronary CTA belongs to non-obstructive CAD4. Compared with patients with no CAD, the presence of non-obstructive CAD detected by coronary CTA was associated with more severe cardiovascular events5,6.
The triglyceride glucose (TyG) index was originally proposed as a reliable substitute to indicate insulin resistance and metabolic syndrome which composed of fasting blood glucose (FBG) and triglycerides7. Researches have indicated a strong relationship between the TyG index and cardiovascular disease (CVD) events8,9. Insulin resistance has been shown to promote atherosclerosis and plaque progression via several mechanisms, including the down-regulation of the insulin and signaling endothelial cell damage pathway10. Clinical studies have confirmed that insulin resistance is associated with CAD and the progression of coronary atherosclerosis. Thus, we speculated that the TyG index was related to CAD and the degree of CAD severity. A higher TyG index has been demonstrated to be associated with a higher incidence of CVD. Moreover, a recent study including 1841 hypertensive patients revealed that the TyG index was positively associated with the incidence of obstructive CAD (odds ratios [ORs] from 2.01 to 2.63 as a categorical variable and OR = 1.49 as a continuous variable)11. However, research focusing on the association between the TyG index and the incidence of myocardial ischemia in patients with minimal to moderate CAD, is still lacking. We therefore aimed to investigate the association between the TyG index and the incidence of myocardial ischemia in patients with minimal to moderate CAD.
Methods
Study population
This was an observational cross-sectional study. The study included patients who underwent coronary CTA examinations at our hospital from November 2018 to December 2020. The inclusion criteria were adults over 18 years old of age who underwent CCTA examination via a 64- or above detector row scanner and well-documented electronic records. We excluded patients who (1) previously underwent percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) surgery; (2) were missing basic clinical data or coronary CTA images; (3) had poor CTA image quality; (4) had missing information on FBG or triglycerides; (5) were lost to follow-up; or (6) had a CAD-RADS score of 0, 4 A, 4B or 5, as defined by coronary CTA. Finally, 1,697 patients with CAD-RADS 1–3 were included in the present study. The flowchart of the study design and patients recruitment was showed in Fig. 1. The study protocol was approved by the Ethics Review Committee of The Central Hospital of Wuhan (WHZXKYKL2022-140) and the written informed consent was waived by the institutional ethics committee of The Central Hospital of Wuhan because of the retrospective observational nature of the study. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Data collection and definitions
All the basic parameters (age, sex, smoking status and drink status), clinical history (hypertension and diabetes), and laboratory test information were collected from electronic medical records. The laboratory tests included triglyceride, total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), serum creatinine (SCR) and FBG. The TyG index was calculated according to the following formula: Ln [(triglyceride, mg/dl) × (FBG, mg/dl)/2].
Coronary CTA examination and features
All coronary CTA examinations were performed with prospectively or retrospectively with an ECG- triggered on a dual-source CT scanner (Somatom Definition Flash, Siemens Medical Solutions, Forchheim, Germany). The coronary CTA images were subsequently analyzed automatically via an AI platform (Computer Aided Diagnosis of Coronary Artery, Version 6.0, Shukun technology, Beijing, China). Interpretation of the AI-based structured reporting for coronary CTA includes the severity, extent, ___location of coronary stenosis, component of coronary plaque, and CT-FFR values. Details of this AI-based coronary CTA platform were presented in previous work12,13 and the National Medical Products Administration has approved this platform (No.20203210844 and No.20233210146). The standardized anatomical CAD-RADS classification using coronary CTA images was defined with the highest degree of coronary artery stenosis: CAD-RADS 0 (0%), CAD-RADS 1 (1–24%), CAD-RADS 2 (25–49%), CAD-RADS 3 (50–69%), CAD-RADS 4 A (70–99% in 1 or 2 vessels), CAD-RADS 4B (left main > 50% or 70–99% in 3-vessels) and CAD-RADS 5 (100%). Minimal to moderate CAD classification was defined as CAD-RADS 1 to 3 (stenosis 1–69%). Computed tomography-adapted Leaman score (CT_LeSc) is a comprehensive coronary CTA score that uses 3 categories of weighting factors, incorporating ___location, severity and plaque component. In the present study, CT_LeSc was evaluated in two categories: CT_LeSc (≤ 5) and CT_LeSc (> 5). Myocardial ischemia was defined as a CT-FFR value ≤ 0.80.
Statistical analysis
Non-normally and normally distributed continuous variables were presented as medians (interquartile ranges, IQRs) and means (standard deviations, SDs), respectively. Categorical variables were showed as absolute values (percentages). One-way analysis of variance or the Kruskal-Wallis test was performed to compare the differences between continuous variables. Categorical variables were compared via Chi-square tests or Fisher’s exact tests. To evaluate the association between the TyG index and myocardial ischemia, univariable and multivariable logistic regression analyses with ORs and 95% confidence intervals (CIs) were conducted. Three models of multivariable logistic regression with backward stepwise selection were performed. Model 1 was adjusted for age, gender, smoke, hypertension, and diabetes. Model 2 was adjusted for age, gender, smoke, hypertension, diabetes, and SCR. Model 3 was adjusted for age, gender, smoke, hypertension, diabetes, SCR, CT_LeSc, and coronary stenosis. In addition, the results of logistic regression were showed based on TyG tertiles (categorical variables) with the T1 group (lowest tertile) used as the reference and by the increase per SD in the TyG index (continuous variable) in the interpretation of the results. The Restricted cubic spline regression was performed to evaluate the non-linear connection between the TyG index and myocardial ischemia. Finally, analyses stratified by sex, hypertension, CT_LeSc and stenosis were performed with an adjusted model. P < 0.05 was considered to indicate statistical significance. All the statistical analyses were carried out via the R statistical package (version 4.3.3, R foundation for Statistical Computing, Vienna, Austria) and SPSS (version 18, SPSS, Inc., Chicago, IL, USA).
Results
Basic characteristics of the study patient
A total of 1,697 patients with non-obstructive CAD were finally analyzed in the current study. The average age of the 1,697 patients was 62.7 ± 9.9 years, and 50.7% were male. The median TyG index was 8.82 (IQR, 8.54–9.09). Compared with patients in the T1 group, patients in the T3 group were more likely to be younger, smokers, drinkers, had a history of hypertension and diabetes. In addition, the prevalence of CT_LeSc > 5 and myocardial ischemia (CT-FFR ≤ 0.8) was increased in the T3 group than in the T1 group (Table 1).
Associations between the TyG index and myocardial ischemia
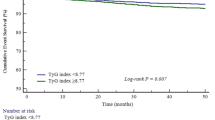
To analysze the non-linear association between the TyG index and myocardial ischemia, restricted cubic splines were performed for flexible modeling. The restricted cubic splines curve appeared to be J-shaped (Fig. 2). The OR (per SD) for the occurrence of myocardial ischemia was significantly increased to 1.38 (1.12–1.69, p = 0.002), with a TyG index ≥ 8.82. However, for the TyG index < 8.82, the OR per SD was 1.03 (95% CI, 0.69–1.53; p = 0.888), which was not significantly associated with the occurrence of myocardial ischemia.
The restricted cubic spline of TyG index and the incidence of myocardial ischemia. The purple columns present the distribution density of the TyG index. The black dashed line represents the OR = 1. The pink line shows the OR value. The pink shaded area represents the 95% CI. TyG, triglyceride glucose; OR, odds ratio; CI, confidence interval; SD, standard deviation; *, statistically significant (P < 0.05).
In univariable analysis, the T3 group was associated with a significantly higher risk of myocardial ischemia than the T1 group (OR, 1.41; 95% CI, 1.01–1.91; p = 0.027). When TyG was regarded as a continuous variable, TyG per SD showed a similar trend (OR, 1.24; 95% CI, 1.09–1.40; p = 0.001) (Table 2). After adjusting for other variables, the T3 group remained associated with a higher risk of myocardial ischemia when the T1 group was regarded as the reference in Model 1, Model 2 and Model 3 (OR, 1.45, 95% CI, 1.04–2.01, p = 0.029; OR, 1.45, 95% CI, 1.01–2.02, p = 0.028; OR, 1.43, 95% CI, 1.01–2.04, p = 0.047) (Table 3; Fig. 3A). Moreover, a 1-SD increase in the TyG index was correlated with a 19–24% elevated risk of myocardial ischemia in the three models (all p < 0.05) (Table 3; Fig. 3B).
Risk of myocardial ischemia based on model 3. TyG index was regarded as categorical variable (A) and continuous variable (B). Model 3 was adjusted by adjust by age, gender, smoke, hypertension, diabetes, SCR, CT_LeSc, coronary stenosis. TyG, triglyceride glucose; SCR, serum creatinine; CT_LeSc, computed tomography-adapted Leaman score; *, statistically significant (P < 0.05).
Subgroup analysis
The associations between the TyG index and myocardial ischemia were further evaluated according to several subgroups by adjusting for confounding factors. The subgroup analysis revealed that female sex, no hypertension, and CT_LeSc > 5 were positively correlated with myocardial ischemia and the TyG index. In addition, 50-69% stenosis showed borderline significance between myocardial ischemia and the TyG index (Fig. 4).
Stratified analyses for the association of TyG with myocardial ischemia based on model 3. Model 3 was adjusted by adjust by age, gender, smoke, hypertension, diabetes, SCR, CT_LeSc, coronary stenosis. TyG, triglyceride glucose; SCR, serum creatinine; CT_LeSc, computed tomography-adapted Leaman score; *, statistically significant (P < 0.05).
Discussion
In our cross-sectional study, we found a significant positive correlation between the TyG index and the incidence of myocardial ischemia in patients with minimal to moderate CAD. Consequently, this study revealed that a higher TyG index was correlated with a 19–24% elevated risk of myocardial ischemia detected by CT-FFR in patients with minimal to moderate CAD. These findings suggest that the TyG index may help identify patients at high risk of myocardial ischemia and guide further examinations and treatments in patients with minimal to moderate CAD.
Historically, coronary CTA has been widely used to diagnose CAD in patients with low to moderate cardiovascular risk and the vast majority of myocardial infarction (MI) cases are caused by non-obstructive plaques14. Furthermore, accumulated evidence from recent coronary CTA trials has confirmed that the MI observed in the follow-up of patients with non-obstructive CAD is as common as that in patients with obstructive CAD15,16. Moreover, recent studies have shown that approximately 50% to two-thirds of patients who undergo coronary CTA have non-obstructive CAD17,18. In addition, researches assessing the presence and degree of stenosis, as well as the plaque ___location and plaque burden of coronary atherosclerosis in patients with non-obstructive CAD, have indicated of strong associations with the prediction of future cardiovascular events4,19,20,21. Other studies further increased the discrepancy of the results. Hadamitzky et al. reported an observational single-center study involving 1,584 suspected CAD patients who underwent coronary CTA during 5.6 years of follow-up and revealed that the non-obstructive CAD for predicting composite endpoint (all-cause death and non-fatal MI) was significant compared with no CAD (HR, 2.46; 95% CI: 1.02–5.90), whereas cardiac events (cardiac death and MI) were not (HR, 6.16; 95% CI: 0.80–47.3)21. Maddox et al. further investigated a large cohort of 37, 674 patients with a 1-year follow-up and reported that 1-vessel or 2-vessel of non-obstructive CAD was not associated with mortality, whereas 3-vessel of non-obstructive CAD was significantly associated with mortality (HR, 1.6; 95% CI: 1.1–2.5)20. Together, these findings indicate the clinical importance of non-obstructive CAD, and most importantly, further risk stratification is needed. CT-FFR has gained a reliable role in assessing lesion-specific ischemia beyond stenosis on coronary CTA for predicting clinical outcomes22. Currently, a CT-FFR ≤ 0.80 is regarded as a positive result of myocardial ischemia and has been proven valuable for guiding treatment and assessing prognosis. However, few studies have focused on myocardial ischemia in patients with non-obstructive CAD. A recent study reported that the current clinical management would have missed nearly 20% of non-obstructive CAD patients with myocardial ischemia23. The current study revealed that 16.9% (286/1697) of non-obstructive patients had myocardial ischemia according to the CT-FFR values, which was similar to the findings of a previous study.
Metabolic syndrome is associated with the incidence of CVD. A previous Canadian cohort study revealed that 51% of the CAD population had metabolic syndrome24. In addition, metabolic syndrome severity has been reported to be closely correlated with the angiographic severity of CAD25. Recent researches have indicated that the blood flow function of the coronary artery (e.g., CT-FFR) outweights the effect of the anatomy of the coronary artery on clinical outcomes26. Although the precise mechanism underlying the relationship between metabolic syndrome and the CT-FFR value is unclear, insulin resistance and metabolic syndrome can impair vasodilation of the coronary arteries and cause inflammation, thus damaging hemodynamic function and reducing the blood flow of the coronary artery27,28.
Accumulated studies have indicated that the TyG index palys a positive role in identifying those at a high risk for developing atherosclerosis in asymptomatic patients. A retrospective registered study recruited 888 asymptomatic type 2 diabetics without CAD history and revealed that the highest tertile of the TyG index was significantly correlated with a high risk of coronary artery stenosis detected by coronary CTA after adjustment for clinical confounders (OR: 3.19; 95% CI, 1.371–7.424)29. Moreover, consistent clinical studies have revealed that an elevated TyG index is associated with an increased incidence of obstructive CAD in patients with type 2 diabetes, non-alcoholic fatty liver disease, established CAD and hypertension29,30,31,32. Nevertheless, compared with previous results, the current study focused on the functional significant stenosis of minimal to moderate CAD subjects detected by coronary CTA and CT-FFR and revealed that the highest tertile of the TyG index was positively associated with an increased incidence of myocardial ischemia in patients with minimal to moderate CAD, which fills some gaps in the research field of the associations between the TyG index and CAD. In addition, subgroup analysis was further conducted to verify the universality of the conclusions and the results suggested that a higher TyG index can predict the occurrence of myocardial ischemia on the basis of CT-FFR in patients with minimal to moderate CAD, irrespective of sex, hypertension, CT_LeSc and coronary stenosis. Thus, the conclusions of the present study have broad practicality in patients with minimal to moderate CAD.
In addition to being associated with an increased incidence of CAD, the TyG index has recently been reported as a useful marker for predicting the prognosis and risk stratification of patients with acute coronary syndrome (ACS), ST-segment elevation myocardial infarction (STEMI) with and without type 2 diabetes, prefrail hypertension, and PCI in STEMI. Wang et al. recruited 101,113 ACS patients and reported that a higher TyG index was associated with an increased risk of in-hospital major adverse cardiovascular events (MACEs)33. Similarly, Rokicka et al. reported that the TyG index was an independent risk factor for in-hospital mortality in patients with STEMI or NoN-ST-segment elevation myocardial infarction (NSTEMI)34. Moreover, a recent retrospective study recruited 404 patients with new-onset STEMI and reported that the prediction nomogram based on the TyG index had greater predictive value for the long-term prognosis of new onset STEMI after PCI35. Furthermore, the TyG index combined with plaque characteristics presented strong diagnostic value for predicting MACEs after PCI in STEMI patients36. In addition, Santulli et al. reported that insulin resistance, defined by the TyG index was significantly associated with physical impairment in older adults with prefrail hypertension37. These studies support the view that the TyG index is an independent marker that might be used to predict poor prognosis both in CAD patients and in individuals after revascularization. Because the TyG index is easier to obtain and less expensive than coronary CTA is, it can be used to screen high-risk patients for further follow-up examinations and more effective clinical strategies.
This study has several strengths. We included relatively large samples. Additionally, we used different models and two perspectives (the TyG index as categorical and continuous variables) to increase the credibility of the results. The current study also has several limitations. First, because the present study relied on observational data, rather than on the results of a cohort or a randomized trial, the potential for patient selection bias remains, and a causal relationship between the TyG index and myocardial ischemia risk could not be determined. Thus, further prospective and multi-center studies are needed to confirm these findings. Second, although the study adjusted for potential clinical risk factors of myocardial ischemia and CAD, some unmeasured or residual confounding factors still exist in the present study, such as other parameters of metabolic syndrome and as some treatments, such as antiplatelets, statins and anti-diabetic drugs which may cause confounding bias in the statistical results. Third, invasive FFR is still the gold standard for determining specific myocardial ischemia rather than CT-FFR, although the perfect consistency between these two examinations has been proven. Finally, the generalizability of our findings is limited by the single-center enrollment.
Conclusions
In conclusion, the present study revealed that a higher TyG index was associated with a higher risk of myocardial ischemia detected by CT-FFR in patients with minimal to moderate CAD. This may provide useful information in risk stratification for myocardial ischemia, directing further detections and guiding more aggressive treatments in patients with minimal to moderate CAD.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
Change history
19 November 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41598-024-79450-8
References
Cury, R. C. et al. CAD-RADS 2.0 - 2022 coronary artery disease-reporting and data system: An expert consensus document of the society of cardiovascular computed tomography (SCCT), the American College of Cardiology (ACC), the American College of Radiology (ACR), and the North America Society of Cardiovascular Imaging (NASCI). JACC Cardiovasc. Imaging 15, 1974–2001. https://doi.org/10.1016/j.jcmg.2022.07.002 (2022).
Writing Committee, M. & AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 78, 2218–2261. https://doi.org/10.1016/j.jacc.2021.07.052 (2021).
Arbab-Zadeh, A. & Fuster, V. From detecting the vulnerable plaque to managing the vulnerable patient: JACC state-of-the-art review. J. Am. Coll. Cardiol. 74, 1582–1593. https://doi.org/10.1016/j.jacc.2019.07.062 (2019).
Han, D. et al. Prognostic significance of plaque ___location in non-obstructive coronary artery disease: From the CONFIRM registry. Eur. Heart J. Cardiovasc. Imaging 23, 1240–1247. https://doi.org/10.1093/ehjci/jeab223 (2022).
Leipsic, J. et al. Sex-based prognostic implications of nonobstructive coronary artery disease: Results from the international multicenter CONFIRM study. Radiology 273, 393–400. https://doi.org/10.1148/radiol.14140269 (2014).
Emami, H. et al. Nonobstructive coronary artery disease by coronary CT angiography improves risk stratification and allocation of statin therapy. JACC Cardiovasc. Imaging 10, 1031–1038. https://doi.org/10.1016/j.jcmg.2016.10.022 (2017).
Simental-Mendia, L. E., Rodriguez-Moran, M. & Guerrero-Romero, F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab. Syndr. Relat. Disord. 6, 299–304. https://doi.org/10.1089/met.2008.0034 (2008).
Kim, M. K. et al. Relationship between the triglyceride glucose index and coronary artery calcification in Korean adults. Cardiovasc. Diabetol. 16, 108. https://doi.org/10.1186/s12933-017-0589-4 (2017).
Sanchez-Inigo, L., Navarro-Gonzalez, D., Fernandez-Montero, A., Pastrana-Delgado, J. & Martinez, J. A. The TyG index may predict the development of cardiovascular events. Eur. J. Clin. Invest. 46, 189–197. https://doi.org/10.1111/eci.12583 (2016).
Yuan, W., Shao, Y., Zhao, D. & Zhang, B. Correlation analysis of lipid accumulation index, triglyceride-glucose index and H-type hypertension and coronary artery disease. PeerJ. 11, e16069. https://doi.org/10.7717/peerj.16069 (2023).
Pan, W. et al. Triglyceride glucose index is associated with obstructive coronary artery disease in hypertensive patients. Cardiovasc. Diabetol. 22https://doi.org/10.1186/s12933-023-01739-1 (2023).
Huang, Z. et al. Comparison of prognostic value between CAD-RADS 1.0 and CAD-RADS 2.0 evaluated by convolutional neural networks based CCTA. Heliyon 9, e15988. https://doi.org/10.1016/j.heliyon.2023.e15988 (2023).
Huang, Z. et al. Clinical evaluation of the Automatic Coronary Artery Disease Reporting and Data System (CAD-RADS) in Coronary computed Tomography Angiography using Convolutional neural networks. Acad. Radiol. 30, 698–706. https://doi.org/10.1016/j.acra.2022.05.015 (2023).
Dweck, M. R. & Newby, D. E. Non-obstructive coronary artery disease can no longer be ignored. Eur. Heart J. Cardiovasc. Imaging 21, 489–490. https://doi.org/10.1093/ehjci/jeaa022 (2020).
Douglas, P. S. et al. Outcomes of anatomical versus functional testing for coronary artery disease. N. Engl. J. Med. 372, 1291–1300. https://doi.org/10.1056/NEJMoa1415516 (2015).
Investigators, S. H. et al. Coronary CT angiography and 5-Year risk of myocardial infarction. N. Engl. J. Med. 379, 924–933. https://doi.org/10.1056/NEJMoa1805971 (2018).
Hoffmann, U. et al. Prognostic value of noninvasive cardiovascular testing in patients with stable chest pain: Insights from the PROMISE trial (prospective Multicenter Imaging Study for evaluation of chest Pain). Circulation. 135, 2320–2332. https://doi.org/10.1161/CIRCULATIONAHA.116.024360 (2017).
Min, J. K. et al. Rationale and design of the CONFIRM (COronary CT angiography EvaluatioN for clinical outcomes: An InteRnational Multicenter) Registry. J. Cardiovasc. Comput. Tomogr. 5, 84–92. https://doi.org/10.1016/j.jcct.2011.01.007 (2011).
van Rosendael, A. R. et al. Clinical risk factors and atherosclerotic plaque extent to define risk for major events in patients without obstructive coronary artery disease: The long-term coronary computed tomography angiography CONFIRM registry. Eur. Heart J. Cardiovasc. Imaging 21, 479–488. https://doi.org/10.1093/ehjci/jez322 (2020).
Maddox, T. M. et al. Nonobstructive coronary artery disease and risk of myocardial infarction. JAMA 312, 1754–1763. https://doi.org/10.1001/jama.2014.14681 (2014).
Hadamitzky, M. et al. Prognostic value of coronary computed tomography angiography during 5 years of follow-up in patients with suspected coronary artery disease. Eur. Heart J. 34, 3277–3285. https://doi.org/10.1093/eurheartj/eht293 (2013).
Ihdayhid, A. R. et al. Prognostic value and risk continuum of noninvasive fractional flow reserve derived from coronary CT angiography. Radiology 292, 343–351. https://doi.org/10.1148/radiol.2019182264 (2019).
Zhao, N. et al. CT-FFR vs a model of combined plaque characteristics for identifying ischemia: Results from CT-FFR CHINA trial. Eur. J. Radiol. 138, 109634. https://doi.org/10.1016/j.ejrad.2021.109634 (2021).
Solymoss, B. C. et al. Incidence and clinical characteristics of the metabolic syndrome in patients with coronary artery disease. Coron. Artery Dis. 14, 207–212. https://doi.org/10.1097/01.mca.0000065744.52558.9f (2003).
Solymoss, B. C. et al. Effect of increasing metabolic syndrome score on atherosclerotic risk profile and coronary artery disease angiographic severity. Am. J. Cardiol. 93, 159–164. https://doi.org/10.1016/j.amjcard.2003.09.032 (2004).
Norgaard, B. L. et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (analysis of Coronary Blood Flow using CT angiography: next steps). J. Am. Coll. Cardiol. 63, 1145–1155. https://doi.org/10.1016/j.jacc.2013.11.043 (2014).
Yu, B. et al. Triglyceride-glucose index is associated with quantitative flow ratio in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Front. Cardiovasc. Med. 9, 1002030. https://doi.org/10.3389/fcvm.2022.1002030 (2022).
Schulman, I. H. & Zhou, M. S. Vascular insulin resistance: A potential link between cardiovascular and metabolic diseases. Curr. Hypertens. Rep. 11, 48–55. https://doi.org/10.1007/s11906-009-0010-0 (2009).
Lee, E. Y. et al. Triglyceride glucose index, a marker of insulin resistance, is associated with coronary artery stenosis in asymptomatic subjects with type 2 diabetes. Lipids Health Dis. 15https://doi.org/10.1186/s12944-016-0324-2 (2016).
Wang, J., Huang, X., Fu, C., Sheng, Q. & Liu, P. Association between triglyceride glucose index, coronary artery calcification and multivessel coronary disease in Chinese patients with acute coronary syndrome. Cardiovasc. Diabetol. 21, 187. https://doi.org/10.1186/s12933-022-01615-4 (2022).
Su, J. et al. Triglyceride glucose index for the detection of the severity of coronary artery disease in different glucose metabolic states in patients with coronary heart disease: A RCSCD-TCM study in China. Cardiovasc. Diabetol. 21, 96. https://doi.org/10.1186/s12933-022-01523-7 (2022).
Zhao, J. et al. TyG index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients. Cardiovasc. Diabetol. 21, 123. https://doi.org/10.1186/s12933-022-01548-y (2022).
Wang, W. et al. Association between the triglyceride-glucose index and in-hospital major adverse cardiovascular events in patients with acute coronary syndrome: Results from the improving care for Cardiovascular Disease in China (CCC)-Acute Coronary Syndrome project. Cardiovasc. Diabetol. 23, 170. https://doi.org/10.1186/s12933-024-02270-7 (2024).
Rokicka, D. et al. The prognostic impact of insulin resistance surrogates in patients with acute myocardial infarction with and without type 2 diabetes. Cardiovasc. Diabetol. 23, 147. https://doi.org/10.1186/s12933-024-02240-z (2024).
Ye, Z. et al. Predicting long-term prognosis after percutaneous coronary intervention in patients with new onset ST-elevation myocardial infarction: Development and external validation of a nomogram model. Cardiovasc. Diabetol. 22, 87. https://doi.org/10.1186/s12933-023-01820-9 (2023).
Zhao, X. et al. Triglyceride glucose index combined with plaque characteristics as a novel biomarker for cardiovascular outcomes after percutaneous coronary intervention in ST-elevated myocardial infarction patients: An intravascular optical coherence tomography study. Cardiovasc. Diabetol. 20, 131. https://doi.org/10.1186/s12933-021-01321-7 (2021).
Santulli, G. et al. Prediabetes increases the risk of Frailty in Prefrail older adults with hypertension: Beneficial effects of Metformin. Hypertension 81, 1637–1643. https://doi.org/10.1161/HYPERTENSIONAHA.124.23087 (2024).
Acknowledgements
This work was supported by The Funding for Scientific Research Projects from Wuhan Municipal Health Commission (WX23B17).
Author information
Authors and Affiliations
Contributions
Study concepts: X.W., Z.F.H., Study design: X.W., Z.F.H., R.Y.T., Y.D., W.P.W., Data acquisition and analysis: X.W., X.Y.D, Z.Q.L., J.W.X., Statistical analysis: Z.F.H., R.Y.T., Manuscript preparation: Z.F.H., R.Y.T., Y.D., W.P.W., Manuscript editing and review: X.W., Z.F.H.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Ethics Review Committee of The Central Hospital of Wuhan (WHZXKYKL2022-140). The written informed consent was waived by institutional ethics committee of The Central Hospital of Wuhan because of retrospective observational nature of the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article Zengfa Huang, Ruiyao Tang, Yi Ding and Wanpeng Wang were omitted as equally contributing authors. Full information regarding the corrections made can be found in the correction for this Article.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, Z., Tang, R., Ding, Y. et al. Association of the triglyceride glucose index with myocardial ischemia in patients with minimal to moderate coronary artery disease. Sci Rep 14, 26093 (2024). https://doi.org/10.1038/s41598-024-76530-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-76530-7
Keywords
This article is cited by
-
Predictive value of the triglyceride-glucose index for coronary artery bypass grafting-acute kidney injury patients
BMC Cardiovascular Disorders (2025)
-
Association of triglyceride-glucose index and derived indices with cataract in middle-aged and elderly Americans: NHANES 2005–2008
Lipids in Health and Disease (2025)