Abstract
Based on the characteristics of Kummell’s disease (KD) and related anatomical structures of the thoracolumbar spine, a novel bone cement screw system has been designed to effectively avoid the cement loosening and displacement. This experiment aimed to assess the biological effects of the novel bone cement screw system in KD on fresh cadaveric thoracolumbar spine specimens, thereby discussing its potential application value and providing a foundation for clinical implementation. This study employed a total of 50 fresh female adult cadaver specimens. Each specimen underwent extraction of the T12 to L2 segment followed by the creation of an artificial KD model at the L1 segment and subsequent establishment of five distinct types of bone cement repair models. Model A represents the percutaneous vertebroplasty (PVP) model, Model B combines PVP with unilateral percutaneous pediculoplasty (PPP), Model C combines PVP with bilateral PPP, Model D introduces the novel bone cement screw combined with unilateral PVP, and Model E combines the novel screw with bilateral PVP, each group consists of 10 specimens. Subsequently, the six-axis spine robot was employed to execute cement three-dimensional biomechanical strength tests in six directions, including anterior flexion and posterior extension, left and right lateral bending, as well as left and right rotation. The novel bone cement screw, whether used unilaterally or bilaterally in combination with the PVP model, exhibits significantly reduced bone cement mobility and superior biomechanical stability during anterior flexion, posterior extension, left lateral bending, and right lateral bending (P<0.05).No significant differences were observed among the five models under both left and right rotation (P > 0.05).When comparing the novel bone cement screw combined with PVP unilaterally and bilaterally, no statistically significant difference was observed in the stability of bone cement across all six directions of motion (P>0.05). To conclude, this novel bone cement bridging screw system exhibits superior biomechanical stability compared to commonly used treatments. Furthermore, both unilateral and bilateral implementations of the novel bone cement screw system yield without significant differences observed. These findings present a reliable and innovative approach for clinical management of KD.
Similar content being viewed by others
Introduction
With the aging population growth in the world, the incidence of spinal fractures, especially osteoporotic vertebral compression fractures (OVCFs) has increased yearly1,2. About one-third of the patients with OVCFs have the risk of developing to Kummell’s disease (KD). KD is defined as a clinical condition in which patients gradually develop severe thoracolumbar pain, progressive kyphosis and even symptoms of neurological damage to varying degrees following an asymptomatic period of months or years after a minor trauma. KD occurs most commonly in the elderly population, and usually affects thoracolumbar region of the spine, with T12-L1 vertebrae being the most frequently affected. KD is also more common in women than in men, with a male to female ratio of approximately 10:13,4.
In recent years, percutaneous vertebroplasty (PVP) has become a main method for the treatment of KD without neurological damage due to the advantages of less trauma, good patient tolerance, rapid pain relief, and effective deformity correction5,6,7,8,9. However, due to the existence of intravertebral vacuum cleft (IVC) in KD, polymethyl methacrylate (PMMA) bone cement, widely used in PVP, is not suitable to be served as an effective filling material, because it cannot penetrate the necrotic sclerotic wall of IVC, and can loosen or even displace easily without rigid internal fixation10. Therefore, even though good clinical results have been achieved after bone cement augmentation5,8, but the frequent occurrence of cement loosening or displacement during the follow-up period has begun to cause concern.
Nakamae et al.11 reported that cement loosening occurred in 25% of OVCF patients with the presence of IVC after 6 months of PVP. Once cement displacement occurred, revision surgery using open posterior, anterior, or combined anterior and posterior approaches is required to remove the displaced cement, reestablish spinal stability, and restore spinal sequence and fusion. Therefore, some scholars adopted short- or long-segment pedicle screw fixation combined with PVP to treat KD in order to avoid cement loosening and displacement, but these methods have disadvantages such as large surgical trauma, loss of spinal mobility, and high treatment costs compared with PVP alone5,12. In order to effectively avoid the occurrence of cement loosening and displacement while preserving the advantages of PVP, the authors’ team has invented a novel bone cement bridging screw system combined with PVP to treat KD. An important indicator for assessing the effectiveness of the novel bone cement bridging screw system is whether the bone cement bridging screw and especially the bone cement that is stabilized in the IVC by the screw can provide better biomechanical stability under three-dimensional (3D) motions, thus effectively avoiding cement loosening and displacement13. In the present study, fresh cadaveric thoracolumbar spine specimens were used, the biomechanical stability of the novel bone cement bridging screw system and other traditional treatment methods were compared. The aim of present study was to clarify the mechanical properties of the novel bone cement bridging screw system, and provide a theoretical basis for its use in the clinical treatment of KD.
Methods
Design of the novel bone cement bridging screw system
Based on the currently used cement-augmented thoracolumbar pedicle screws, a novel bone cement bridging screw system was designed and manufactured using Ti6Al4V alloy to lock the bong cement and avoid cement loosening and displacement. The structural features of the novel bone cement bridging screw system include (Fig. 1): (1) the screw used is minimally invasive percutaneous screw. It has a hollow path in the center of the screw, allowing the guide wire to pass through. The tail of the screw is connected with the holder that can be inserted percutaneously. (2) Multiple cement outlets are set on the front of the screw, which gradually increase from the tail to the head of the screw to facilitate better bone cement filling in the anterior, middle columns of the injured vertebra and IVC. (3) The screw does not fix the adjacent segments of the injured vertebra and does not affect the spine mobility, so a screw without a tail cap is adopted, which can be embedded in the pedicle after insertion. (4) In order to increase the fixation strength of the novel bone cement bridging screw system, the portion of the screw inserted into the pedicle is double-threaded with local enlargement and thickening, while the portion of the screw inserted into the vertebral body is single-threaded, this design can facilitate the creation of cement outlets and accelerate screw insertion.
Additionally, the structural features of the bone cement injection device of the novel bone cement bridging screw system are listed as following: (1) the device consists of a holder, a connecting rod and a syringe or a cement pusher (Figs. 2 and 3), the holder is equipped with an operating channel, and the connecting rod is equipped with a bone cement channel. (2) The novel bone cement bridging screw is connected with one end of the holder. One end of the connecting rod is extended into the operating channel of the holder, where it is connected with the tail of the novel bone cement bridging screw. (3) The other end of the connecting rod is connected with the syringe or pusher, through which the bone cement is finally injected into the injured vertebra. The bone cement injection device designed in this study can not only provide safe and easy injection of bone cement, but also effectively reduce bone cement leakage at the connections of the device.
Biomechanical testing
Specimen preparation
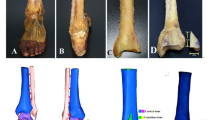
Fifty fresh thoracolumbar spine (T12-L2) specimens were obtained from elderly female cadavers. All specimens were confirmed to have skeletal integrity, without abnormal bone development or bone damage by gross observation, computed tomography (CT) and X-ray. The bone mineral density (BMD) of all specimens was less than − 2.5 g/cm3, which met the diagnostic criteria for osteoporosis (Fig. 4). All muscles were removed from the specimens, and all posterior ligaments, joint capsules, intervertebral discs and bony structures were retained. The specimens were stored in sealed plastic bags in a refrigerator at -80 °C during the experimental preparation phase, which were then thawed at room temperature prior to experimental analysis. Biomechanical testing was performed within 1 week after all specimens were obtained.
Model establishment and grouping
After thawing the specimens, anterior and posteriorvertebral body heights of all specimens were measured. Based on the measurement results, the diameter of the wedge-shaped IVC required to simulate KD was calculated, then an IVC with an angle of 15° was created by osteotomy from 1/4 below the superior endplate of L1 to 2/3 of the sagittal diameter of the vertebral body with an osteotome. All exposed cancellous surfaces were covered with bone wax to simulate margin sclerosis of the IVC, thus creating KD model (Fig. 5).
According to the different ways of bone cement filling in the IVC, all specimens were randomly divided into five groups (n = 10 per group): PVP alone (group A), PVP combined with unilateral percutaneous pediculoplasty (PPP, group B), PVP combined with bilateral PPP (group C), unilateral novel bone cement bridging screw combined with PVP (group D), and bilateral novel bone cement bridging screw combined with PVP (Group E) groups. The procedures involved in establishing models in each group were as follows:
In Group A, for the establishment of PVP alone model, the puncture point was determined according to the herringbone crest vertex insertion method, a 3.0-mm diameter drill was used to create a bony channel by drilling along the central axis of the pedicle at a medial inclination angle of 10°-15° to the spinous process. The bony channel reached a depth of 80% of the anterior edge of the vertebral body, and entered the target IVC in anterior vertebral column. Subsequently, bone cement (2:1 PMMA powder-to-liquid ratio, Tecres S.p.A., Italy) was used and injected into the bony channel until a toothpaste-like consistency had been reached. Bone cement injection was stopped after the IVC was completely filled. The injection device was removed after the cement solidified.
In Group B, for the establishment of PVP combined with unilateral PPP model, the procedures for PVP were the same as mentioned above. After PVP performed by unilateral approach was completed, the injection device in the channel was slowly retracted while bone cement injection was continued until unilateral PPP was completed.
In Group C, for the establishment of PVP combined with bilateral PPP model, procedures for PVP were the same as mentioned above. After PVP performed by bilateral approach was completed, the injection device was slowly retracted while bone cement injection was continued until completion of bilateral PPP.
In Group D, for the establishment of unilateral novel bone cement bridging screw combined with PVP model, the puncture point was determined according to the herringbone crest vertex insertion method, a 3.0-mm diameter drill was used to create a bony channel by drilling along the central axis of the pedicle at a medial inclination angle of 10°-15° to the spinous process. The bony channel reached a depth of 80% of the anterior edge of the vertebral body, and entered the target IVC in anterior vertebral column. A ball-tip probe was used to confirm the integrity of four bony walls of the screw channel. After tapping the screw channel with a 6.0 mm-diameter tap, screw channel was probed with a probe again. The screw was then screwed to ensure that the bone cement outlets on the front of the screw were located in the wedge-shaped IVC. Then bone cement was prepared, “toothpaste-like” cement was injected into the novel bone cement bridging screw until PVP was completed.
In Group E, for the establishment of bilateral novel bone cement bridging screw combined with PVP model, procedures for novel bone cement bridging screw insertion and PVP were the same as mentioned above, bilateral pedicle screw placement was performed, bone cement was injected into the bilateral novel bone cement bridging screws until bilateral PVP was completed.
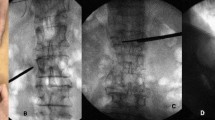
After model establishment in each group, CT scan was performed on each specimen to observe bone cement filling status, screw position, the presence and absence of vertebral body damage or spinal cord compression caused by bone cement leaking into the spinal canal (Fig. 6). All specimens were stored at -80° and subjected to biomechanical testing within 1 week.
Postoperative CT images: (a) percutaneous vertebroplasty (PVP) alone; (b): PVP combined with unilateral percutaneous pediculoplasty (PPP); (c): PVP combined with bilateral PPP; (d): unilateral novel bone cement bridging screw combined with PVP; (e): bilateral novel bone cement bridging screw combined with PVP.
3D biomechanical stability testing
Before biomechanical testing, the specimens were thawed at room temperature. An appropriate amount of mixture of acrylic modified epoxy resin and amine was poured into the embedding module, and the lumbar 2 vertebral body of the specimen was placed into the embedding module, and the embedding medium was allowed to fully solidify for 3 min. The same method was used to embed specimens of the lumbar 1 vertebral body. The embedded specimens were then obtained (Fig. 7) and stored at -25 ℃. Then the lower end of specimens was held in place in the center of the fixture attached to the base of the six-axis spinal motion testing machine (SY-03-108, Shanghai Tuoteng Biomechanics Laboratory, Shanghai, China).
Biomechanical testing was performed on all cadaveric specimens using the same six-axis spinal motion testing machine in a non-destructive manner. After thawing the embedded specimens at room temperature, two Kirschner wires (K-wires) were inserted proximally to the superior and inferior margins of the L1 bone cement-filled vertebral body, respectively. Three light point balls of the optical motion capture system (OptiTrack, NaturalPoint, Inc., USA) were subsequently attached to the tip of the K-wires. The specimens of each group were placed on the six-axis spinal motion testing machine sequentially. A 500-N vertical compressive load was applied to the top of the specimens in order to simulate the weight of the human upper body. The specimens of each group was loaded with a moment of 10 N/m in 6 motion conditions, including forward flexion, backward extension, left lateral bending, right lateral bending, left axial rotation and right axial rotation (Fig. 8). The infrared camera of the optical motion capture system captured the light point balls fixed on the tip of the K-wires to record the 3D motions (roll, pitch and yaw motions) of the superior and inferior K-wires. The overall deflection angles of the K-wires was then calculated by using the angle equation of the optical motion capture system (Fig. 9), the differences between the deflection angles of the superior and inferior K-wires were used to represent the range of motion (ROM) in the cement-augmented area of the vertebra. The specimen was kept moist with saline spray every 5 min during the test. After completion of the test, all specimens were examined by CT to assess the status of internal fixation.
Angle calculation equation of the optical motion capture system. (A) Schematic diagram illustrating the calculation of angles (θ, φ, and ψ) of range of motion; (B) the transformation matrix between coordinate systems; (C) coordinates of the vectors after completion of loading; (D) angle γ of range of motion after loading and before loading).
Main observation indicators
After bone cement augmentation, the motion of bone cement in the human cadaveric model of KD in 6 motion directions including forward flexion, backward extension, right/ left lateral bending, right/left axial rotation was compared between the five groups.
Statistical analysis
SPSS 26.0 software (IBM Inc., USA) was used for the statistical analyses in this study. The results are presented as mean ± standard deviation (SD). The Kruskal-Wallis test was used for the comparison of multiple groups. Wilcoxon test was used for pairwise comparison between two groups. A P value < 0.05 was regarded as statistically significant. The statistical level was set at alpha = 0.05 (two-sided).
Results
The BMD T-scores of specimens in each group are shown in Table 1. The BMD T-scores of the specimens were similar and were not statistically different among the five groups (P = 0.779), indicating this experiment is not interfered by the difference in BMD of the specimens among groups.
3D motions of the bone cement with the use of different methods for surgical repair of KD in 6 motion states were compared. As shown in Table 2; Fig. 10, the use of unilateral and bilateral novel bone cement bridging screws combined with PVP both showed better cement stability compared with other three groups in four motion directions, flexion, extension, left and right lateral bending (both P < 0.05), suggesting that the novel bone cement bridging screw could better stabilize the cement in these four directions of motion.
Comparison between Groups D and E showed that although there was a slight difference in motion of the bone cement between the two groups, but the difference was not statistically significant (P > 0.05), indicating that the unilateral and bilateral novel bone cement bridging screws may have similar effects in stabilizing the bone cement in the IVC.
Additionally, although there were some differences in the motion of the bone cement between five groups in left and right axial rotation, but the differences were not statistically significant (P > 0.05), suggesting that the novel bone cement bridging screw could not achieve better cement stability in the axial rotation directions.
Discussion
With the increasing aging of the population, the prevalence of OVCFs is alarmingly high, affecting up to 50% of women aged ≥ 80 years and up to 25% of women aged 70–79 years, some patients with OVCFs can develop KD14,15,16,17. Thus, the prevalence of KD is also rising as the aging population grows.
The treatment options for KD are still highly controversial. Initially, conservative treatments such as bed rest, the use of analgesics, drugs such as bisphosphonates, and immobilization with braces are adopted in an attempt to relieve pain, stabilize and restore bone mineral density, and increase the stability of the vertebral body14,18. However, conservative treatment has proved ineffective in many patients, leads to treatment delay, and even the occurrence of severe symptoms. Therefore, patients have to abandon conservative treatment and receive surgical treatment14. PVP as the primary treatment method for KD has achieved satisfactory results, which can markedly reduce postoperative pain16,19. However, for the treatment of patients with KD and those presenting with IVC, PVP has its drawbacks, i.e. cement loosening and displacement may easily occur during and after PVP5,14,20. In order to reduce cement loosening and displacement, many scholars have proposed the use of short-segment percutaneous pedicle screw fixation with cement augmentation, and received good results21,22,23. Tang et al.24 also proposed the use of multilevel cement-augmented pedicle screws fixation to effectively avoid postoperative complications. Wang et al.25 used robot-assisted PVP combined with PPP for the treatment of single-segment KD, and obtained good clinical results. However, there is currently no effective method to prevent cement loosening and displacement following PVP alone for KD.
Based on the analysis of the causes of cement loosening and displacement, the authors’ team innovatively invented a novel bone cement bridging screw system. During bone cement injection, the bone cement can be released slowly through the multiple lateral bone cement outlets on the front of the screw and completely fill the IVC, the screw is firmly connected with the bone cement. Meanwhile, the screw is inserted into the vertebral body, that acts as a “bridge” to interlock bone cement and the surrounding bone tissue, and even the pedicle (a strongest point of attachment of the spine), thus creating a tight interlock between bone cement and the vertebral body, this is the most important innovative point in this novel cement bridging screw system.
A previous study conducted by authors’ team used 3D finite element analysis to explore the biomechanical stability of the novel bone cement bridging screw system, and found that the use of novel bone cement bridging screw for surgical repair of KD obviously improved the cement stability in four directions of motion, including flexion, extension, right and left lateral bending, but this 3D finite element study has some limitations. Therefore, this biomechanical study using human cadaveric thoracolumbar spine was conducted to investigate whether bone cement stability can be achieved in human cadaveric model of KD by using the novel bone cement bridging screw, so as to provide a basis for future clinical application of this system in the treatment of KD.
Biomechanical stability of the novel bone cement bridging screw system in motion states of flexion and extension. In the present study, biomechanical testing results showed that the mean ROM for the cadaveric models in groups A-E were 1.65 ± 0.10°, 1.11 ± 0.14°, 1.03 ± 0.08°, 0.40 ± 0.12°, 0.39 ± 0.09°, respectively, in flexion, 3.08 ± 0.23°, 1.57 ± 0.25°, 1.48 ± 0.44°, 0.42 ± 0.11°, 0.40 ± 0.10°, respectively, in extension. Unilateral and bilateral novel bone cement bridging screws combined with PVP both exhibited better bone cement stability compared with other three groups in motion states of flexion and extension (P < 0.05). The results indicate that under flexion and extension conditions, the use of novel bone cement bridging screw for surgical repair of KD have excellent effects in stabilizing the bone cement, results in less motion and enhanced stability of the cement in the vertebral body. Consistent with our goal for design of the novel bone cement screw system, the novel bone cement screw has the ability to avoid cement loosening and displacement by closely connecting the bone cement in the IVC with surrounding bone tissue through hollow channel inside the screw and lateral bone cement outlets on the front of the screw.
Biomechanical stability of the novel bone cement bridging screw system in motion states of left and right lateral bending. In the present study, biomechanical testing results showed that the mean ROM of models in Groups A-E were 2.92 ± 0.54°, 0.72 ± 0.14°, 0.70 ± 0.16°, 0.44 ± 0.08°, and 0.43 ± 0.06°, respectively, in left lateral bending, and 4.07 ± 1.07°, 0.81 ± 0.15°, 0.79 ± 0.12°, 0.45 ± 0.07°, and 0.48 ± 0.14°, respectively, in right lateral bending. Unilateral and bilateral novel bone cement bridging screws combined with PVP both exhibited better bone cement stability compared with other three groups in these two motions (P < 0.05), indicating that under these two motion states, the novel bone cement bridging screw is effective for stabilization of the bone cement in the injured vertebra, allows the bone cement and the vertebral body to interlock, and prevents lateral loosening and displacement of the bone cement after surgery.
Biomechanical stability of the novel bone cement bridging screw system in states of left and right axial rotation. Biomechanical testing results also showed that the mean ROM of models in Groups A-E were 2.67 ± 0.16°, 2.78 ± 0.19°, 2.69 ± 0.21°, 2.82 ± 0.20°, 2.79 ± 0.17°, respectively, in left axial rotation, and 2.66 ± 0.11°, 2.65 ± 0.10°, 2.60 ± 0.17°, 2.62 ± 0.16, and 2.58 ± 0.24°, respectively, in right axial rotation, but there was no significant difference in cement stability between the five groups under these two motion states (P > 0.05). This result is consistent with the findings from our previous study, indicating that the novel bone cement bridging screw did not exert stabilizing effects during vertebral rotation, which only improved cement stability in four directions of flexion, extension, right and left lateral bending, but did not improve cement stability in left and right axial rotation, this is a disadvantage of novel bone cement bridging screw.
Comparison of the biomechanical performance of unilateral and bilateral novel bone cement bridging screw fixation. In the present study, no statistically significant difference was found in the motion of bone cement between the unilateral and bilateral novel bone cement bridging screw combined with PVP groups in four directions of flexion, extension, left and right lateral bending (P = 0.976, P = 0.806, P = 0.747, P = 0.645, respectively). Comparison of unilateral and bilateral PVP for severe OVCFs conducted by Chen et al.26 documented that unilateral PVP achieved the same clinical results compared with bilateral PVP. The results of the present also showed that clinical outcomes of unilateral and bilateral novel bone cement bridging screw fixation were almost identical. So theoretically, the use of a single novel bone cement bridging screw may achieve good cement stability. The findings provide a theoretical basis for the clinical application of unilateral novel bone cement bridging screw fixation in the treatment of KD.
In previous investigations, the researchers conducted three-dimensional finite element analysis and biomechanical experiments on animal specimens. The findings of this human cadaveric biomechanical study were consistent with those of the prior experiments, providing additional substantiation for the stability and efficacy of this innovative bone cement bridging screw system27,28.
Conclusions
The findings of the present study demonstrated that the novel bone cement bridging screw can better stabilize the bone cement on human cadaveric thoracolumbar spine specimens, and enhance cement stability in the injured vertebra. The cadaveric specimens used in the present study were obtained from elderly women with osteoporosis, which can simulate the bone quality of patients with KD to a certain extent, and resemble human clinical situation more closely. Due to the difficulty in obtaining cadaveric specimens, the sample size included in this study was small, which may lead to bias. Despite this limitation, this biomechanical study provides insight into the stabilizing effect of the novel bone cement bridging screw system on the bone cement in the injured vertebra. Our findings suggest that compared with conventional cement augmentation procedures for KD, the use of the novel bone cement bridging screw system provided superior cemented stability in the four directions of motion, including flexion, extension, left and right lateral bending. Furthermore, unilateral and bilateral novel bone cement bridging screws achieved similar effects for stabilization of bone cement injected into the injured vertebra. The findings provide strong evidence for the clinical application of the novel bone cement bridging screw system in the future, which is of great importance to optimize treatment options for KD in clinical practice.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chi, L. et al. Vertebral fracture in postmenopausal Chinese women: a population-based study. Osteoporos. International: J. Established as Result Cooperation between Eur. Foundation Osteoporos. Natl. Osteoporos. Foundation USA. 28(9), 2583–2590. https://doi.org/10.1007/s00198-017-4085-1 (2017).
Rajasekaran, S. et al. Osteoporotic thoracolumbar fractures-how are they different?-Classification and treatment algorithm. J. Orthop. Trauma. 31 Suppl.(4), S49–S56. https://doi.org/10.1097/BOT.0000000000000949 (2017).
Osterhouse, M. D. & Kettner, N. W. Delayed posttraumatic vertebral collapse with intravertebral vacuum cleft. J. Manip. Physiol. Ther. 25(4), 270–275. https://doi.org/10.1067/mmt.2002.123164 (2002).
Young, W. F., Brown, D., Kendler, A. & Clements, D. Delayed post-traumatic osteonecrosis of a vertebral body (Kummell’s disease). Acta Orthop. Belg. 68(1), 13–19 (2002).
Chen, L., Dong, R., Gu, Y. & Feng, Y. Comparison between Balloon Kyphoplasty and short segmental fixation combined with Vertebroplasty in the treatment of Kümmell’s Disease. Pain Physician. 18(4), 373–381 (2015).
Ma, R., Chow, R. & Shen, F. H. Kummell’s disease: delayed post-traumatic osteonecrosis of the vertebral body. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European section. Cerv. Spine Res. Soc. 19(7), 1065–1070. https://doi.org/10.1007/s00586-009-1205-4 (2010).
Liu, F. et al. Anterior reconstruction versus posterior osteotomy in treating Kümmell’s disease with neurological deficits: a systematic review. Acta Orthop. Traumatol. Turc. 52(4), 283–288. https://doi.org/10.1016/j.aott.2018.05.002 (2018).
Krauss, M., Hirschfelder, H., Tomandl, B., Lichti, G. & Bär, I. Kyphosis reduction and the rate of cement leaks after vertebroplasty of intravertebral clefts. Eur. Radiol. 16(5), 1015–1021. https://doi.org/10.1007/s00330-005-0056-6 (2006).
Chen, G. D. et al. Percutaneous kyphoplasty for Kummell Disease with severe spinal canal stenosis. Pain Physician. 18(6), E1021–E1028 (2015).
Lee, S. H., Kim, E. S. & Eoh, W. Cement augmented anterior reconstruction with short posterior instrumentation: a less invasive surgical option for Kummell’s disease with cord compression. J. Clin. Neuroscience: Official J. Neurosurgical Soc. Australasia. 18(4), 509–514. https://doi.org/10.1016/j.jocn.2010.07.139 (2011).
Nakamae, T. et al. Risk factors for cement loosening after vertebroplasty for osteoporotic vertebral fracture with Intravertebral cleft: a retrospective analysis. Asian Spine J. 12(5), 935–942. https://doi.org/10.31616/asj.2018.12.5.935 (2018).
Li, H. K. et al. Percutaneous kyphoplasty versus posterior spinal fixation with vertebroplasty for treatment of Kümmell disease: a case-control study with minimal 2-year follow-up. Medicine. 96(51), e9287. https://doi.org/10.1097/MD.0000000000009287 (2017).
Zahaf, S. & Kebdani, S. Biomechanical Study between the rigid and dynamic fixation systems of the spinal column analyzed by the finite element method. Nano Biomed. Eng. 9(2), 169–183. https://doi.org/10.5101/nbe.v9i2.p169-183 (2017).
Adamska, O., Modzelewski, K., Stolarczyk, A. & Kseniuk, J. Is Kummell’s Disease a misdiagnosed and/or an underreported complication of osteoporotic vertebral compression fractures? A pattern of the condition and available treatment modalities. J. Clin. Med. 10(12), 2584. https://doi.org/10.3390/jcm10122584 (2021).
Zhu, Y. et al. Therapeutic effect of kyphoplasty and balloon vertebroplasty on osteoporotic vertebral compression fracture: a systematic review and meta-analysis of randomized controlled trials. Medicine. 98(45), e17810. https://doi.org/10.1097/MD.0000000000017810 (2019).
Lou, S. et al. Percutaneous vertebroplasty versus non-operative treatment for osteoporotic vertebral compression fractures: a meta-analysis of randomized controlled trials. Osteoporos. International: J. Established as Result Cooperation between Eur. Foundation Osteoporos. Natl. Osteoporos. Foundation USA. 30(12), 2369–2380. https://doi.org/10.1007/s00198-019-05101-8 (2019).
Xu, J., Lin, J., Li, J., Yang, Y. & Fei, Q. Targeted percutaneous vertebroplasty versus traditional percutaneous vertebroplasty for osteoporotic vertebral compression fracture. Surg. Innov. 26(5), 551–559. https://doi.org/10.1177/1553350619853134 (2019).
Pierce, T. P. et al. A current review of core decompression in the treatment of osteonecrosis of the femoral head. Curr. Rev. Musculoskelet. Med. 8(3), 228–232. https://doi.org/10.1007/s12178-015-9280-0 (2015).
Wang, Y., Liu, B., Sun, Z., Zhang, Y. & Su, J. Comparative efficacy of three minimally invasive procedures for Kümmell’s disease: a systematic review and network meta-analysis. Front. Surg. 9, 893404. https://doi.org/10.3389/fsurg.2022.893404 (2022).
Wei, H., Dong, C., Zhu, Y. & Ma, H. Analysis of two minimally invasive procedures for osteoporotic vertebral compression fractures with intravertebral cleft: a systematic review and meta-analysis. J. Orthop. Surg, Res. 15(1), 401. https://doi.org/10.1186/s13018-020-01938-6 (2020).
Park, S. J., Kim, H. S., Lee, S. K. & Kim, S. W. Bone cement-augmented percutaneous short segment fixation: an effective treatment for Kummell’s Disease? J. Korean Neurosurg. Soc. 58(1), 54–59. https://doi.org/10.3340/jkns.2015.58.1.54 (2015).
Cho, Y. Posterior vertebrectomy and circumferential fusion for the treatment of advanced thoracolumbar Kümmell disease with neurologic deficit. Asian Spine J. 11(4), 634–640. https://doi.org/10.4184/asj.2017.11.4.634 (2017).
Huang, Y. S. et al. Bone cement-augmented short-segment pedicle screw fixation for Kümmell Disease with spinal canal stenosis. Med. Sci. Monitor: Int. Med. J. Experimental Clin. Res. 24, 928–935. https://doi.org/10.12659/msm.905804 (2018).
Tang, Y. C. et al. Effect and potential risks of using multilevel cement-augmented pedicle screw fixation in osteoporotic spine with lumbar degenerative disease. BMC Musculoskelet. Disord. 21(1), 274. https://doi.org/10.1186/s12891-020-03309-y (2020).
Wang, B. et al. Pediculoplasty combined with vertebroplasty for the treatment of Kummell’s disease without neurological impairment: robot-assisted and fluoroscopy-guided. Am. J. Translational Res. 12(12), 8019–8029 (2020).
Chen, C. et al. Unilateral versus bilateral vertebroplasty for severe osteoporotic vertebral compression fractures. J. Spin. Disord. Tech. 27(8), E301–E304. https://doi.org/10.1097/BSD.0000000000000118 (2014).
Wang, B. et al. Biomechanical analysis of a novel bone cement bridging screw system for the treatment of Kummell disease: a finite element analysis. Am. J. Translational Res. 14(10), 7052–7062 (2022).
Zhan, Y. et al. Biomechanical analysis of a novel bone cement bridging screw system combined with percutaneous vertebroplasty for treating Kummell’s disease. Front. Bioeng. Biotechnol. 11, 1077192. https://doi.org/10.3389/fbioe.2023.1077192 (2023).
Acknowledgements
This research was funded by Key Research and Development Program of Shaanxi Province, grant number No.2020GXLH-Y-003; Key Research and Development Program of Shaanxi Province, grant number No. 2020SFY-095; Shaanxi Province Science and Technology Nova Project, grant number No. 2022KJXX-64; General Cultivation Project of Xi ‘an Health Bureau, grant number No. 2024ms11.
Author information
Authors and Affiliations
Contributions
B.W. and D.H. conceived the experiment(s), Y.Z. and J.W. conducted the experiment(s), H.Y. and J.Y. analyzed the results, Y.Z., H.Y. and L.L. wrote the manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethics Committee of Honghui Hospital Affiliated to Xi ‘an Jiaotong University (No: 20211012). The informed consent from “body donors” was obtained before the death and any personal data was hidden.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhan, Y., Yang, H., Wang, J. et al. A biomechanical investigation comparing a novel bone cement bridging screw system with conventional treatment methods for Kummell’s disease. Sci Rep 14, 25545 (2024). https://doi.org/10.1038/s41598-024-77511-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77511-6